Abstract
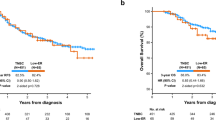
The aim of this study is to reveal likely demographic, clinical, and pathological differences among hormone receptor negative breast cancer patients according to their HER-2 status. The medical records of hormone receptor negative breast cancer patients with known HER-2 status between January 1999 and December 2006 were reviewed, retrospectively. A total of 91 cases were included in the study (68 HER-2 negative cases and 23 HER-2 positive cases). The results obtained showed that median age, menarche age, childbearing age, number of children, menopause age, and body-mass indexes were similar in both groups. The HER-2 negative patients had more family history of breast cancer than HER-2 positive patients (13.2% and 0%, respectively, P = 0.091). Eighty-three patients received neoadjuvant/adjuvant chemotherapy. Recurrence occurred in 41 (46.6%) patients. Neither recurrence nor disease-free survival of those patients was associated with HER-2 status. Tumor size (P = 0.042) and number of involved lymph nodes (P = 0.001) were found to be independent prognostic factors for disease-free survival. A tendency for more frequent cerebral metastasis was found in HER-2 positive advanced stage patients (P = 0.052). HER-2 positive patients were less responsive to taxanes (P = 0.071). The number of involved lymph nodes (P = 0.004) and HER-2 status (P = 0.043) were found to be prognostic factors for overall survival. HER-2 positive and negative patients should be followed and treated with different strategies. HER-2 positive patients are at least as resistant to systemic therapies as the HER-2 negative patients. Genetic counseling should be routinely provided to triple negative patients and their families. HER-2 positive patients may be candidates for prophylactic treatment strategies concerning cerebral metastasis.


Similar content being viewed by others
References
Ferlay J, et al. Estimates of the Cancer incidence and mortality in Europe in 2006. Ann Oncol. 2007;18:581–92. doi:10.1093/annonc/mdl498.
Jemal A, et al. Cancer Statistics, 2007. CA Cancer J Clin. 2007;57:43–66.
Ravdin PM, et al. The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med. 2007;356:1670–4. doi:10.1056/NEJMsr070105.
Cinieri S, et al. Adjuvant strategies in breast cancer: new prospectives, questions and reflections at the end of 2007 St. Gailen International Expert Consensus Conference. Ann Oncol. 2007;18 Suppl 6:63–5. doi:10.1093/annonc/mdm227.
Cleator S, Heller W, Coombes RC. Triple-negative breast cancer: therapeutic options. Lancet Oncol. 2007;8:235–44. doi:10.1016/S1470-2045(07)70074-8.
Liu H, et al. Basal-HER2 phenotype shows poorer survival than basal-like phenotype in hormone receptor-negative invasive breast cancers. Hum Pathol. 2008;39:167–74. doi:10.1016/j.humpath.2007.06.012.
Kim MJ, et al. Clinicopathologic significance of the basal-like subtype of breast cancer: a comparison with hormone receptor and Her2/neu-overexpressing phenotypes. Hum Pathol. 2006;37:1217–26. doi:10.1016/j.humpath.2006.04.015.
Carey LA. Race, breast cancer subtypes, and survival in the Carolina breast cancer study. JAMA. 2006;295:2492–502. doi:10.1001/jama.295.21.2492.
Brown M, Tsodikov A, Bauer KR, Parise CA, Caggiano V. The role of human epidermal growth factor receptor 2 in the survival of women with estrogen and progesterone receptor-negative, invasive breast cancer: the California Cancer Registry, 1999–2004. Cancer. 2008;112:737–47. doi:10.1002/cncr.23243.
llis IO, et al. Updated recommendations for her-2 testing in the UK. J Clin Pathol. 2004;57:233–7.
Greene FL, et al. AJCC cancer staging manual. 6th ed. New York (NY): Springer-Verlag; 2002.
Turner NC, et al. BRCA1 dysfunction in sporadic basal-like breast cancer. Oncogene. 2007;26:2126–32. doi:10.1038/sj.onc.1210014.
Kennedy RD, Quinn JE, Mullan PB, Johnston PG, Harkin DP. The role of BRCA1 in the cellular response to chemotherapy. J Natl Cancer Inst. 2004;96:1659–68.
Lal P, Tan LK, Chen B. Correlation of HER-2 status with estrogen and progesterone receptors and histologic features in 3, 655 invasive breast carcinomas. Am J Clin Pathol. 2005;123:541–6. doi:10.1309/YMJ3A83TB39MRUT9.
Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9:606–16. doi:10.1634/theoncologist.9-6-606.
Lin NU, Bellon JR, Winer EP. CNS metastases in breast cancer. J Clin Oncol. 2004;22:3608–17. doi:10.1200/JCO.2004.01.175.
Ryberg M, et al. Predictors of central nervous system metastasis in patients with metastatic breast cancer. A competing risk analysis of 579 patients treated with epirubicin-based chemotherapy. Breast Cancer Res Treat. 2005;91:217–25. doi:10.1007/s10549-005-0323-x.
Tham YL, Sexton K, Kramer R, Hilsenbeck S, Elledge R. Primary breast cancer phenotypes associated with propensity for central nervous system metastases. Cancer. 2006;107:696–704. doi:10.1002/cncr.22041.
Gabos Z, et al. Prognostic signifıcance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol. 2006;24:5658–63. doi:10.1200/JCO.2006.07.0250.
Palmieri D, et al. Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res. 2007;67:4190–8. doi:10.1158/0008-5472.CAN-06-3316.
Gori S, et al. Central nervous system metastases in HER-2 positive metastatic breast cancer patients treated with trastuzumab: incidence, survival, and risk factors. Oncologist. 2007;12:766–73. doi:10.1634/theoncologist.12-7-766.
Nam BH, et al. Breast cancer subtypes and survival in patients with brain metastases. Breast Cancer Res. 2008;10:R20. doi:10.1186/bcr1870.
Banerjee S, et al. Basal-like breast carcinomas: clinical outcome and response to chemotherapy. J Clin Pathol. 2006;59:729–35. doi:10.1136/jcp.2005.033043.
Tsai CM, et al. Enhanced chemoresistance by elevation of the level of p185neu in HER-2/neu transfected human lung cancer cells. J Natl Cancer Inst. 1995;87:682–4. doi:10.1093/jnci/87.9.682.
Yu D, Hung MC. Overexpression of ErbB2 in cancer and ErbB2-targeting strategies. Oncogene. 2000;19:6115–21. doi:10.1038/sj.onc.1203972.
Pritchard KI, et al. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med. 2006;354:2103–11. doi:10.1056/NEJMoa054504.
Hayes DF, et al. HER2 and response to paclitaxel in node-positive breast cancer. N Engl J Med. 2007;357:1496–506. doi:10.1056/NEJMoa071167.
Chen JS, Lan K, Hung MC. Strategies to target HER2/neu overexpression for Cancer therapy. Drug Resist Updat. 2003;6:129–36. doi:10.1016/S1368-7646(03)00040-2.
Piccart-Gebhart MJ, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353:1659–72. doi:10.1056/NEJMoa052306.
Romond EH, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673–84. doi:10.1056/NEJMoa052122.
Hudis CA. Trastuzumab-mechanism of action and use in clinical practice. N Engl J Med. 2007;357:39–51. doi:10.1056/NEJMra043186.
Burstein HJ, et al. Trastuzumab plus vinorelbine or taxane chemotherapy for HER2-overexpressing metastatic breast cancer: the trastuzumab and vinorelbine or taxane study. Cancer. 2007;110:965–72. doi:10.1002/cncr.22885.
Slamon DJ, et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–82. doi:10.1126/science.3798106.
Borg A, et al. HER-2/neu amplification predicts poor survival in node-positive breast cancer. Cancer Res. 1990;50:4322–7.
Winstanley J, et al. The long term prognostic significance of c-erb-2 in primary breast cancer. Br J Cancer. 1991;63:447–50.
Paterson MC, et al. Correlation between c-erb-2 amplification and risk of recurrent disease in node-negative breast cancer. Cancer Res. 1991;51:566–7.
Clark GM, McGuire WL. Follow-up study of HER-2/neu amplification in primary breast cancer. Cancer Res. 1991;51:944–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cicin, I., Karagol, H., Usta, U. et al. Triple negative breast cancer compared to hormone receptor negative/HER2 positive breast cancer. Med Oncol 26, 335–343 (2009). https://doi.org/10.1007/s12032-008-9126-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-008-9126-3