Abstract
Background
We aimed to provide a systematic description of our 2-year experience using a standardized bedside, single burr hole approach to intracranial multimodality monitoring (MMM) in patients with severe traumatic brain injury (sTBI), focusing on safety and probe reliability.
Methods
We performed this observational cohort study at a university-affiliated, Level I trauma center with dedicated 20-bed neuroscience intensive care unit. We included 43 consecutive sTBI patients who required MMM to guide clinical care based on institutional protocol and had a four-lumen bolt placed to measure intracranial pressure, brain tissue oxygen, regional cerebral blood flow, brain temperature, and intracranial electroencephalography.
Results
sTBI patients were aged 41.6 ± 17.5 years (mean ± SD) and 84% were men. MMM devices were placed at a median of 12.5 h (interquartile range [IQR] 9.0–21.4 h) after injury and in non-dominant frontal lobe in 72.1% of cases. Monitoring was conducted for a median of 97.1 h (IQR 46.9–124.6 h) per patient. While minor hemorrhage, pneumocephalus, or small bone chips were common, only one (2.4%) patient experienced significant hemorrhage related to device placement. Radiographically, device malpositioning was noted in 13.9% of patients. Inadvertent device discontinuation occurred for at least one device in 58% of patients and was significantly associated with the frequency of travel for procedures or imaging. Devices remained in place for > 80% of the total monitoring period and generated usable data > 50% of that time.
Conclusions
A standardized, bedside single burr hole approach to MMM was safe. Despite some probe-specific recording limitations, MMM provided real-time measurements of intracranial pressure, oxygenation, regional cerebral blood flow, brain temperature, and function.
Similar content being viewed by others
Background
The measurement of intracranial pressure (ICP) is a cornerstone of modern neurointensive care management after severe traumatic brain injury (sTBI). ICP acts as a corollary measure of intracranial volume, but also allows calculation of cerebral perfusion pressure and the pressure-reactivity index as surrogates of cerebral blood flow and autoregulation. Thus, it is increasingly recognized that the use and interpretation of ICP is more complicated than the traditional volume–pressure relationship ascribed to Monro and Kellie [1]. This is highlighted by the guidelines from the Brain Trauma Foundation, which contain no Level I or Level IIa recommendations for physiologic monitoring or treatment thresholds, including ICP [2].
For more advanced monitoring, technologies are commercially available for the continuous measurement and integrated bedside display of not only ICP, but also brain tissue oxygen (PbtO2), regional cerebral blood flow (rCBF), intracranial temperature (ICT), and intracranial electroencephalography (iEEG). The use of PbtO2 can guide reductions in brain tissue hypoxia burden by 77% [3] and has been recommended along with rCBF and continuous EEG in a consensus statement of the Neurocritical Care Society [4]. The utility of iEEG has expanded with recent evidence that the presence of spreading depolarizations [5, 6] and periodic discharges or seizures [7] provide information on the metabolic status of local brain tissue. Comprehensive measurement of these parameters provides an opportunity to guide management in a more precise, patient-specific way.
We standardized a bedside approach to perform intracranial multimodality monitoring (MMM) in patients following sTBI in order to optimize the detection and treatment of secondary brain injuries at our institution. Our approach includes a single, four-lumen bolt through which multiple catheters are passed into the frontal lobe and connected to an integrated, time-locked bedside display. We describe here our experience over a 2-year period, focusing on the safety and reliability of intracranial measurements in a population of patients with sTBI.
Methods
Settings and Design
We performed a retrospective analysis of prospectively identified sTBI patients undergoing MMM between March 2015 and March 2017 at the University of Cincinnati Medical Center, an American College of Surgeons-designated Level I Trauma Center. All sTBI patients were admitted to our dedicated Neuroscience Intensive Care Unit (NSICU), which provides care per national guidelines. MMM was recommended based on a separate clinical protocol (see Additional File 1). Patients < 80 years old were eligible if motor Glasgow Coma Scale (GCS) subscore ≤ 5 and eye GCS ≤ 2, accounting for patients with GCS ≤ 8 resulting from aphasia or severe orbital edema precluding eye-opening. The decision to place MMM was made at the treating team’s discretion with periodic reassessment for intoxicated patients or those with other reversible causes for coma. This study was approved by the University of Cincinnati’s Institutional Review Board and complied with international standards for clinical research. Informed consent was not required for this observational study. All devices were used according to their FDA-approved indications.
Study Procedures
Bedside placement of MMM devices was performed by neurosurgical house staff upon arrival to the NSICU once the clinical decision for MMM was made. Procedural consent was obtained from family, legal representative, or was done under emergency consent. Procedural contraindications were observed, including the presence of irreversible coagulopathies. Routine prophylactic antibiotics were not used. MMM devices were targeted to frontal white matter by default. Focal disturbances in brain tissue oxygen [8], blood flow [9], or electrical activity [5] occur in proximity to injured tissue. In order to increase the probability of capturing pathological conditions potentially amenable to intervention, our approach was to monitor the most injured hemisphere preferentially except when craniectomy or unstable skull fractures necessitated contralateral placement.
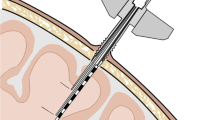
All patients underwent sterile bedside burr hole placement. An area approximately 1–2 cm in front of the coronal suture in the mid-pupillary line was prepped and draped. This area was infiltrated with lidocaine and a stab incision was made. A burr hole was created using a handheld drill fitted with a 5.3-mm-diameter drill bit and the dura was incised. A four-lumen titanium bolt (Hemedex, Inc.; Cambridge, MA) was secured into place. The angle at which probes exit the bolt is oriented away from center, such that probes are splayed and do not come into contact with each other. ICP/PbtO2 and rCBF/ICT probes were placed approximately 2.5–3 cm below the inner table of the skull. The iEEG array was targeted to 1.5 cm deep to maximize the likelihood of cortical location for some contacts, allowing detection of spreading depolarizations [10]. A confirmatory head computed tomography (CT) was obtained immediately thereafter.
To measure ICP/PbtO2, we used the Neurovent®-PTO (Raumedic Inc.; Mills River, NC). rCBF/ICT were measured using the QFlow 500™ Perfusion Probe (Hemedex Inc.; Cambridge, MA). iEEG was recorded with an 8-contact Spencer® Depth Electrode (Ad-Tech Medical Instrument Corporation; Racine, WI). All data were recorded through a bedside central nervous system Monitor (Moberg Research Inc.; Ambler, PA) with full-band EEG amplifier capable of recording direct current signals. In all cases, an external reference was used: Either a platinum needle electrode was placed subdermally at the mastoid or a Ag–AgCl plastic cup was placed at the vertex. The decision to place a simultaneous external ventricular drainage catheter (EVD) was considered separately on a patient-by-patient basis. MMM data were available for clinical decision-making in all cases.
Following completion of monitoring, all data were archived in their original format. We retrospectively collected clinical data including demographics, medical history and current medications, injury severity, and details about monitoring devices and placement. Laboratory values including platelet count, thromboelastography (TEG) R time, and international normalized ratio (INR) were collected as part of routine trauma protocols at our institution and obtained from medical records. Patient outcomes were obtained from medical records based on outpatient clinic visits or follow-up phone calls.
Review of MMM Safety and Data Validity
For each patient, radiographic placement was reviewed by one of the authors (LBN). Perilesional placement was defined as MMM device position ≤ 2 cm from contusion or hypodensity. Malposition was defined as MMM device position outside of expected location within the frontal subcortical white matter. Device-related hemorrhage was documented if a) hemorrhage was absent prior to monitor placement and b) located within the immediate vicinity of the devices. Significant hemorrhage was considered if hemorrhage expanded or was symptomatic, defined as requiring treatment. Infection was documented if there was clinical suspicion leading to antibiotic administration or if cerebrospinal fluid cultures were positive.
All raw monitoring data and bedside annotations were reviewed by one of the authors (BF). Periods in which devices were recalibrating or temporarily disconnected were quantified as recording gaps. Inadvertent device discontinuation, such as from individual probes being dislodged or unplugged during the course of care, was documented when any device stopped providing data prior to the end of the monitoring period.
The PbtO2 probe measures the dissolution of gaseous O2; however, placement induces local microtrauma and the movement of dissolved oxygen may be impeded initially. PbtO2 trends were examined and annotations identifying O2 challenges (an increase in the fraction of inspired oxygen to 100% on the ventilator) were used to establish reliability, defined as PbtO2 increase ≥ 10 mmHg after O2 challenge or spontaneous variability correlated with other monitoring data (e.g., blood pressure). The difference between start of data collection and the point at which PbtO2 appeared reliable was termed the PbtO2 lag.
The QFlow 500™ Perfusion Probe stops measuring periodically in order to recalibrate for measurement validity, and recalibration cycles were set at 120 min. With each recalibration, a Probe Placement Assistant (PPA) value is generated to quantify mechanical displacement related to local pulsatility that may skew rCBF measurement. Periods of PPA > 2 and PPA > 5 were separately quantified. PPA > 2 reflects pulsatility, but PPA > 5 suggests an unstable thermal field and inaccurate data.
Statistical Analysis
Normally distributed variables were reported as mean ± standard deviation. Non-normally distributed variables were reported as medians with interquartile range (IQR). Where appropriate, Fisher’s exact and Wilcoxon rank-sum tests were performed to compare groups. p values < 0.05 were accepted as statistically significant.
Results
Patient Characteristics
A total of n = 43 patients underwent clinically indicated MMM during the 2-year study period. The mean age was 41.6 ± 17.5 years and 84% (36/43) were men (Table 1). The majority (55.8% [24/43]) who underwent MMM had nonsurgical sTBI. MMM was placed a median of 12.5 h (IQR 9.0–21.4 h) from the time of injury. The mean intensive care unit length-of-stay was 10.4 ± 6.5 days and hospital length-of-stay was 14.8 ± 11.3 days. Based on the IMPACT core variables (age, pupillary findings, and motor GCS) [11], the predicted mortality of our cohort was 25 ± 18%. 51.2% (22/43) survived with a median Glasgow Outcome Score of severe disability (3; IQR 3–4) reported a median of 4.4 months (IQR 2.7–5.5 months) after injury.
Monitoring Device Placement, Imaging Findings, and Complications
MMM devices were placed most commonly in the non-dominant frontal lobe (72.1% [31/43]) (Fig. 1a). Of those placed in dominant frontal lobe, 75% (9/12) were placed contralateral to craniectomy (7/12), unstable skull fracture (1/12), or non-operative subdural hematoma (1/12).
Device placement examples. a Correct placement of intracranial multimodality monitoring (MMM) devices. Head computed tomography (CT) image showing placement in relatively uninjured left frontal white matter. Inset shows the scout image from the CT scan, demonstrating the placement of the three probes. b Malpositioned MMM devices placed too deeply within the white matter, in this case approaching the midline structures as seen on head CT. The inset shows the scout image from the CT with devices placed > 3 cm from the bolt at the skull surface. c CT prior to device placement in a 44-year-old man who presented after motorcycle collision. His initial post-resuscitation Glasgow Coma Scale score was 6T. He was not taking antiplatelet or anticoagulants and his initial platelets, international normalized ratio, and thromboelastography were normal. d CT following placement demonstrates position of the MMM devices in the left frontal white matter after craniotomy and evacuation of the previously seen right frontal subdural hematoma. Notice region of hypodensity surrounding the MMM devices and hemorrhagic conversion of ischemic tissue (denoted by black arrow). MMM devices recorded a normal intracranial pressure with relative brain tissue hypoxia and oligemia with suppressed cortical signaling
The majority of devices (60.5% [26/43]) were placed in injured frontal lobe (Table 1): 69.2% (18/26) were placed in patients with bifrontal injury, of which five were perilesional and two were within injured cortex. 15.3% (4/26) were placed near focal frontal contusion, of which three were perilesional, and 15.3% (4/26) were placed in a hemisphere with diffuse traumatic subarachnoid hemorrhage.
34.9% (15/43) had surgery prior to bedside placement of monitors. Of these, 46.1% (7/15) were placed in relatively uninjured tissue; all were placed contralateral to surgical skull defect. In 4/43 patients, surgery was performed after monitoring was initiated; in three, devices were replaced for continued monitoring. Overall, device placement was noted to be too deep in 4 patients (Fig. 1b) and too shallow in two patients. Only two were devices affected. In one, PbtO2 was too shallow and did not provide reliable values. In the second, the ICP waveform became attenuated as the sensor migrated out of the cortex and the catheter was replaced.
Clinically asymptomatic minor hemorrhage, pneumocephalus, or small bone chips within the path of devices were observed in 17/42 (40.5%). A single, significant intracranial hemorrhagic complication related to probe placement was observed during the 2-year period (Fig. 1c, d); however, no surgical or medical intervention was required. Four patients had a history of antiplatelet/anticoagulant use; none developed significant hemorrhage and two had minor, asymptomatic tract hemorrhage. Similarly, there was no relationship between the presence of device-related hemorrhage and either admission INR (Wilcoxon rank-sum test, p = 0.23), TEG R time (Wilcoxon rank-sum test, p = 0.24), or platelet count (Wilcoxon rank-sum test, p = 0.77). No patients with MMM had signs of central nervous system infection.
Monitoring Devices and Data Reliability
MMM was performed for a median 97.1 h (IQR 46.9–124.6 h). We monitored ICP/PbtO2 in all patients, rCBF/ICT in 95.3% (41/43) patients, and iEEG in 90.7% (39/43) patients. Device discontinuation was noted at some point in 58% (25/43) of patients: ICP/PbtO2 in 16.3% (7/43), rCBF/ICT in 41.4% (17/41), and iEEG in 15.4% (6/39). During monitoring, two-thirds (29/43) of patients travelled for procedures or imaging, with a median of 1 trip (IQR 0–2) lasting 50.0 ± 17.5 min. The number of trips was significantly associated with device discontinuation (Wilcoxon rank-sum test, p = 0.03). There were no bleeding or imaging findings associated with discontinued probes.
Available usable data from each device are shown in Fig. 2. As a result of recording gaps and device discontinuation, not all devices recorded data for the entire monitoring period. The lag time between PbtO2 placement and the first reliable value was a median 8.3 h (IQR 4.0–19.8 h). For the rCBF probe, recalibration was more frequent when PPA was in the range of 2–5 (Spearman’s rho 0.41, p = 0.01). All probes remained in place for > 80% of the total monitoring period and generated usable data for > 50% of that time. Figures 3 and 4 illustrate representative cases in which MMM provided clinically relevant information beyond that available from ICP monitoring alone.
Usable data recorded during intracranial multimodality monitoring. Bar graph showing the average percentage of the total monitoring period for each device recorded. Unplanned device discontinuation resulted in devices that did not record for the entire monitoring period. Gaps in recorded data as a result of temporary device disconnection or recalibration are also shown as a percentage of the overall recording period. By way of example, arterial blood pressure (ABP) either was not in place or was removed an average of 1% of the total monitoring time. An average of 3.1% of the total monitoring time, there were temporary gaps in ABP data due to arterial blood draws, flushing, or temporary disconnections. The Raumedic PbtO2 measurement exhibited a lag in data reliability, in most cases thought to be related to local microtrauma, referred to here as “ % PbtO2 Lag,” accounting for an average of 17.3% of the total monitoring duration. The QFlow 500™ rCBF measurement exhibited gaps in recording specifically related to recalibration cycles that are required for measurement validity, and therefore no measurements were available during 19.1% of the total recording period. In addition, data recording with a Probe Placement Assistant (PPA) value of > 2 may be usable, but a PPA value of > 5 is not accurate and the probe may require repositioning
rCBF and brain tissue oxygenation depend on adequate perfusion pressure. a, b Case illustration of a 21-year-old man who presented after high-speed motorcycle collision. Initial post-resuscitation Glasgow Coma Scale score was 6T. a CT on admission (post-trauma day [PTD] 0) showed no intracranial hemorrhage but concern for diffuse axonal injury. On PTD2, intracranial multimodality monitoring (MMM) was initiated, 51 h following injury. CT immediately after placement of probes demonstrated “new parenchymal hypodensities involving the periphery of the frontal and occipital lobes” (white triangles) suggestive of developing infarction. The location of the regional cerebral blood flow probe is circled in red. b The initial intracranial pressure (ICP) was 15 mmHg and cerebral perfusion pressure (CPP) was 60 mmHg. Nonetheless, regional cerebral blood flow (perfusion) remained < 5 ml/100 g/min and brain tissue oxygen (PbtO2) was 15–20 mmHg. Vasopressors were started (dashed arrow), resulting in a rapid increase in CPP to 70 mmHg and a decrease in ICP to 12 mmHg. As the CPP continued to rise to 80 mmHg, the perfusion increased to 30 ml/100 g/min. CT performed the following day (post-trauma day 3) demonstrated resolution of previously observed hypodensities; the rCBF probe is not seen as it had pulled out during travel to CT. c, d Case illustration of another 21-year-old male pedestrian who was struck by a motor vehicle and presented with a post-resuscitation Glasgow Coma Scale score of 4T. c Initial CT demonstrated left subdural hematoma with midline shift. Following decompressive hemicraniectomy, MMM was initiated at 39 h post-injury in the contralateral frontal lobe. d Initially, ICP was poorly controlled between 20 and 30 mmHg despite adequate sedation and hyperosmotic treatment. In order to interpret the PbtO2 measurement, we first tested for reliability by performing an oxygen challenge. The fraction of inspired oxygen (FiO2) was briefly increased to 100%, leading to an elevated PbtO2 value of 43 mmHg (black arrowhead). The FiO2 was then returned to 40%, while peripheral oxygen saturation (SpO2) remained near 100% for the duration of the record. The brain tissue oxygen measured 1 mmHg despite an ‘adequate’ CPP of 60 mmHg and a regional cerebral blood flow (perfusion) > 35 ml/100 g/min, consistent with hyperemia. The clinical team chose to more aggressively fluid resuscitate the patient, leading to an increase in the CPP to 85 mmHg (red dashed arrow). While ICP improved, the PbtO2 increased only to 5 mmHg, and therefore vasopressors were started (black dashed arrow). With this step, CPP climbed to 95 mmHg, further driving down ICP to < 20 mmHg and increasing the brain tissue oxygen to 21 mmHg
Spreading depolarizations and periodic discharges reflect ischemic vulnerability of the cortex. a–c Case illustration of a 68-year-old man who suffered a fall down stairs. Initial post-resuscitation Glasgow Coma Scale score was 9T and declined to 7T shortly after admission to the NSICU. Seven spreading depolarizations (SDs) were observed through the course of multimodality monitoring (MMM) and were associated with changes in multiple variables. a CT demonstrated multifocal contusions and diffuse subarachnoid blood. Intracranial MMM was initiated 6 h following injury, and the depth electrode location is shown on the lateral scout image. b Representative SD is observed as a large negative DC shift on iEEG (e.g., dashed box, top trace, electrode 2) and simultaneous depression of high-frequency (0.5–50 Hz) spontaneous activity. The inset shows the time delay (arrows; 39 s) of DC shift between electrode 1 and 2 (2.2 mm separation), which demonstrates a propagation speed of 3.4 mm/min. Simultaneous with the SD, there is a transient increase in intracranial temperature and rCBF [32], in addition to longer lasting increases in rCBF and PbtO2. There are no corresponding changes in MAP, ICP, or CPP, illustrating that SD is a local tissue phenomenon indicating focal, rather than global, ischemic vulnerability [5, 6]. c The metabolic response to SD was stereotyped, as illustrated by overlay of tracings from two consecutive SDs occurring with an interval of 12.5 h. d MMM in a 44-year-old man who presented with post-resuscitation Glasgow Coma Scale score of 4T following a motorcycle collision. MMM was placed contralateral to a right frontal depression skull fracture 8 h following injury. As highlighted in the solid black box, the initial depth electrode recording demonstrated nearly continuous 0.5–1 Hz periodic sharp wave discharges with superimposed faster frequencies. During this period, the regional cerebral blood flow (perfusion) was < 10 ml/100 g/min. Vasopressors were begun, leading to a gradual increase in perfusion to 20 ml/100 g/min (red vertical line). As perfusion is sustained, the depth electrode then shows an increase in faster frequencies and resolution of the periodic discharges. This is shown by the increasingly bright colors in the digital spectral array (DSA) and in the tracings shown in the dashed black box
Discussion
This study confirms the safety of a bedside, single burr hole approach to MMM that yields high-resolution clinical data with implications for clinical management. This represents the first study to systematically evaluate MMM specifically in patients with sTBI and provides critical data about risks and expectations that can be used by others evaluating a similar approach. We found an acceptable 2.4% risk of significant hemorrhage, with no complication that required treatment. Across patients, devices provided continuous measurements of ICP, PbtO2, rCBF, ICT, and iEEG for more than half of the median 4 days of monitoring.
ICP monitoring is frequently used as an indicator of secondary brain injury [12]. Up to 89% of those with sTBI have elevations in ICP [13], but the impact of elevated ICP alone in survivors of sTBI is not clear [14]; ICP-guided treatment has not been shown to improve outcome in a randomized controlled trial [15] despite contrary evidence from large meta-analyses [16, 17]. ICP may be more useful when interpreted in the context of additional physiologic data, such as PbtO2 [3, 18].
To date, there is no Level I evidence to support the use of MMM and few published guidelines for how MMM should be implemented. In the most comparable study to date, 61 patients with SAH underwent MMM in which evolving techniques were described; a dual burr hole technique was safely used in 39% (24/61) [19]. Due to differences in managing SAH versus sTBI, the placement time for our sTBI patients was earlier (median 12.5 h compared with median 2 days in those with SAH) with a shorter average monitoring duration (median 4 days compared to 7 days). In both cohorts, placement strategies were similar, with most probes placed near injured tissue or contralateral to skull defects (65.5% in sTBI compared with 71% of those with focal injuries related to SAH). While we preferentially target the most injured hemisphere, there is no strong evidence to guide the placement of MMM and more than one-third of our patients were monitored using the relatively uninjured hemisphere.
Our study demonstrated an overall hemorrhage rate of 40.5% (17/42), the majority of which (14/17) consisted of incidental tract hemorrhage. Reported hemorrhage rates after EVD placement often disregard such incidental and small tract hemorrhages and thus report hemorrhage rates as low as 1.8% [20]. Meta-analyses have showed rates of 6–7% in mixed neurosurgical patient populations [21, 22]. In studies that have reported small, incidental hemorrhages with EVD placement, overall hemorrhage rates were 33–41% [23, 24], with larger hemorrhages comprising 5–20%. In comparison, single intraparenchymal monitors, which are placed using small drill bits (typically 2.7 mm diameter) and are either tunneled beneath the scalp or use a single-lumen bolt, are associated with lower overall hemorrhage rates of 3–5% [25, 26] and rates of significant hemorrhage as low as 1.1% (7/631 in one series) [27]. In our sTBI patients, in which we use a 5.3-mm-diameter drill bit and placement of a four-lumen bolt for insertion of multiple intraparenchymal devices, we had only one patient (2.4%) exhibit significant hemorrhage, although no surgical treatment was required. Similarly, only one significant hemorrhage was observed in a SAH patient undergoing MMM while on antiplatelet agents [19]. Significant bleeding complications related to MMM are similar to single intraparenchymal devices: When combining published data on MMM complications in patients with SAH [19] and sTBI from our cohort, the significant hemorrhage rate is 1.9% across 326 individual probes placed in 104 patients. The overall hemorrhage rate, including incidental tract hemorrhages, although greater than single parenchymal monitoring, is comparable to EVD placement.
Whereas PbtO2 is often measured using Clark electrode devices (e.g., Licox [Integra Life Sciences Corporation; Plainsboro, NJ]), we used a second-generation fluorescence-based device, the Neurovent®-PTO [28]. Compared with the only randomized controlled trial of PbtO2 monitoring, which found 3% of their data was unreliable, we found a similar proportion of our recorded data (4.2%) was not usable due to gaps in recording or device discontinuation. [3]. While Licox can take up to 2 h to equilibrate [29], Neurovent’s larger fiberoptic catheter exhibited a lag period lasting a median of 8 h. We found the lowest quantity of usable data was rCBF, approximately 62.1% of total monitoring time. This may appear low, but the rCBF monitor has several built-in quality control measures, including periodic recalibration, to ensure the validity and accuracy of real-time rCBF measurements when displayed [30]. Nonetheless, a mean of 39 h of rCBF data per patient is a clear improvement on single time-point modalities with limited availability, e.g., Xe-CT or single-positron emission computed tomography. Finally, we uncovered an important association between travel and inadvertent device discontinuation, highlighting a risk of travel in spite of precautions. At our institution, travel is facilitated by at least one critical care nurse and a respiratory therapist and device connectors are securely wrapped during travel to reduce the likelihood of damage or displacement. Guidance on cable management and adequate strain-relief measures may be useful for clinical teams re-connecting devices after travel.
Our study was limited in that we included only sTBI patients that both met our protocol’s criteria and were deemed appropriate for invasive monitoring by the clinical team. Patients may have been excluded from invasive monitoring due to expected mortality, irreversible coagulopathy, expected resolution of intoxication, or clinical improvement shortly after presentation. The mortality rate observed in this study, which was higher than predicted by existing models, suggests a net selection bias for use of MMM in our most severely injured patients. In view of this bias, the low rate of complications is particularly noteworthy. More definitive criteria are required to capture the “clinical judgement” inherent in our decisions regarding who is deemed appropriate for monitoring. Additional limitations include retrospective rather than prospective clinical data abstraction and that our ability to make a definitive diagnosis of intracerebral infection, which relies on positive cerebrospinal fluid cultures [31]. Only 9.3% (4/43) in our cohort had concurrent EVD for sampling. Infection related to MMM in SAH occurred in 4.9% (3/61) [19], two of whom had concurrent EVD. EVD harbor 8% incidence of infection [31], while intraparenchymal monitors have 0.6–2.1% incidence [27, 31]. Finally, the ‘validity’ and the clinical relevance of data from these devices are subject to interpretation. For instance, there is no gold-standard for PbtO2 signal validity. Periods of artifact within the signal that did not completely obscure the data were not quantified, which may have resulted in overestimation of usable data.
Conclusions
We report our experience over a 2-year period using a standardized bedside, single burr hole approach to intracranial multimodality monitoring. We were able to safely and consistently measure ICP, oxygenation, regional cerebral blood flow, temperature, and function. This approach generated real-time neuromonitoring data and provides a benchmark for the future use of MMM to guide a precision-medicine approach to the clinical management of patients with severe acute neurological injuries, such as sTBI. Future studies will be needed to determine whether MMM-driven management protocols improve clinical outcomes compared to more conventional monitoring based only on single modalities or serial neurological examination.
References
Hawthorne C, Piper I. Monitoring of intracranial pressure in patients with traumatic brain injury. Front Neurol. 2014;5:121.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Okonkwo DO, Shutter LA, Moore C, et al. Brain oxygen optimization in severe traumatic brain injury phase-II: a phase II randomized trial. Crit Care Med. 2017;45:1907–14.
Le Roux P, Menon DK, Citerio G, et al. Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care: a statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1189–209.
Dreier JP, Fabricius M, Ayata C, et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J Cereb Blood Flow Metab. 2017;37:1595–625.
Hartings JA. Spreading depolarization monitoring in neurocritical care of acute brain injury. Curr Opin Crit Care. 2017;23:94–102.
Vespa P, Tubi M, Claassen J, et al. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann Neurol. 2016;79:579–90.
Hawryluk GWJ, Phan N, Ferguson AR, et al. Brain tissue oxygen tension and its response to physiological manipulations: influence of distance from injury site in a swine model of traumatic brain injury. J Neurosurg. 2016;125:1217–28.
Cunningham AS, Salvador R, Coles JP, et al. Physiological thresholds for irreversible tissue damage in contusional regions following traumatic brain injury. Brain. 2005;128:1931–42.
Jeffcote T, Hinzman JM, Jewell SL, et al. Detection of spreading depolarization with intraparenchymal electrodes in the injured human brain. Neurocrit Care. 2014;20:21–31.
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165.
Cnossen MC, Huijben JA, van der Jagt M, et al. Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care Lond Engl. 2017;21:233.
Jones PA, Andrews PJ, Midgley S, et al. Measuring the burden of secondary insults in head-injured patients during intensive care. J Neurosurg Anesthesiol. 1994;6:4–14.
Badri S, Chen J, Barber J, et al. Mortality and long-term functional outcome associated with intracranial pressure after traumatic brain injury. Intensive Care Med. 2012;38:1800–9.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471–81.
Yuan Q, Wu X, Sun Y, et al. Impact of intracranial pressure monitoring on mortality in patients with traumatic brain injury: a systematic review and meta-analysis. J Neurosurg. 2015;122:574–87.
Shen L, Wang Z, Su Z, et al. Effects of intracranial pressure monitoring on mortality in patients with severe traumatic brain injury: a meta-analysis. PLoS ONE. 2016;11:e0168901.
Nangunoori R, Maloney-Wilensky E, Stiefel M, et al. Brain tissue oxygen-based therapy and outcome after severe traumatic brain injury: a systematic literature review. Neurocrit Care. 2012;17:131–8.
Stuart RM, Schmidt M, Kurtz P, et al. Intracranial multimodal monitoring for acute brain injury: a single institution review of current practices. Neurocrit Care. 2010;12:188–98.
Patil V, Lacson R, Vosburgh KG, et al. Factors associated with external ventricular drain placement accuracy: data from an electronic health record repository. Acta Neurochir (Wien). 2013;155:1773–9.
Binz DD, Toussaint LG, Friedman JA. Hemorrhagic complications of ventriculostomy placement: a meta-analysis. Neurocrit Care. 2009;10:253–6.
Bauer DF, Razdan SN, Bartolucci AA, et al. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011;69:255–60.
Gardner PA, Engh J, Atteberry D, et al. Hemorrhage rates after external ventricular drain placement. J Neurosurg. 2009;110:1021–5.
Maniker AH, Vaynman AY, Karimi RJ, et al. Hemorrhagic complications of external ventricular drainage. Neurosurgery. 2006;59:ONS419–24.
Poca M-A, Sahuquillo J, Arribas M, et al. Fiberoptic intraparenchymal brain pressure monitoring with the Camino V420 monitor: reflections on our experience in 163 severely head-injured patients. J Neurotrauma. 2002;19:439–48.
Koskinen L-OD, Grayson D, Olivecrona M. The complications and the position of the Codman MicroSensor™ ICP device: an analysis of 549 patients and 650 Sensors. Acta Neurochir (Wien). 2013;155:2141–8.
Bekar A, Doğan S, Abaş F, et al. Risk factors and complications of intracranial pressure monitoring with a fiberoptic device. J Clin Neurosci. 2009;16:236–40.
Wolf S, Horn P, Frenzel C, et al. Comparison of a new brain tissue oxygenation probe with the established standard. Acta Neurochir Suppl. 2012;114:161–4.
Ngwenya LB, Burke JF, Manley GT. Brain tissue oxygen monitoring and the intersection of brain and lung: a comprehensive review. Respir Care. 2016;61:1232–44.
Hinzman JM, Andaluz N, Shutter LA, et al. Inverse neurovascular coupling to cortical spreading depolarizations in severe brain trauma. Brain J Neurol. 2014;137:2960–72.
Lozier AP, Sciacca RR, Romagnoli MF, et al. Ventriculostomy-related infections: a critical review of the literature. Neurosurgery. 2002;51:170–81.
Li C, Narayan RK, Wang P, et al. Regional temperature and quantitative cerebral blood flow responses to cortical spreading depolarization in the rat. J Cereb Blood Flow Metab. 2017;37:1634–40.
Acknowledgements
The authors wish to acknowledge the hard work and expertise of the Neurosurgery Residents and Neurocritical Care Fellows at the University of Cincinnati.
Funding
This work was supported in part by the Office of the Assistant Secretary of Defense for Health Affairs, through the Defense Medical Research and Development Program under Award No. W81XWH-16-2-0020. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense. Funding was also provided by National Institute of Neurological Disorders and Stroke and Mayfield Education and Research Foundation.
Author information
Authors and Affiliations
Contributions
BF and LBN are involved in study concept and design, data collection, data analysis, and manuscript draft. ES collected the data. JMH collected the data and revised the manuscript. NA involved in study concept and manuscript revisions. JAH contributed to study concept and design, and critical manuscript review.
Corresponding author
Ethics declarations
Conflict of interest
There are no competing interests related to this study. Study authors BF, LBN, and JH participate in federally funded clinical and translational research that includes intracranial electroencephalography and multimodality monitoring technologies. BF receives consulting fees from Sage Therapeutics, Inc. and speaking fees from UCB.
Ethical Approval
This study was approved by the University of Cincinnati’s Institutional Review Board and complied with international standards for clinical research.
Informed consent
Informed consent was not required for this observational study. All devices were used according to their FDA-approved indications.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Advanced Neuromonitoring Protocol.
An institutional protocol used to standardize an approach to multimodal monitoring in patients with acute brain injuries such as traumatic brain injury (DOCX 44 kb)
Rights and permissions
About this article
Cite this article
Foreman, B., Ngwenya, L.B., Stoddard, E. et al. Safety and Reliability of Bedside, Single Burr Hole Technique for Intracranial Multimodality Monitoring in Severe Traumatic Brain Injury. Neurocrit Care 29, 469–480 (2018). https://doi.org/10.1007/s12028-018-0551-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0551-7