Abstract
The Zika virus outbreaks highlight the growing importance need for a reliable, specific and rapid diagnostic device to detect Zika virus, as it is often recognized as a mild disease without being identified. Many Zika virus infection cases have been misdiagnosed or underreported because of the non-specific clinical presentation. The aim of this review was to provide a critical and comprehensive overview of the published peer‐reviewed evidence related to clinical presentations, various diagnostic methods and modes of transmission of Zika virus infection, as well as potential therapeutic targets to combat microcephaly. Zika virus is mainly transmitted through bites from Aedes aegypti mosquito. It can also be transmitted through blood, perinatally and sexually. Pregnant women are advised to postpone or avoid travelling to areas where active Zika virus transmission is reported, as this infection is directly linked to foetal microcephaly. Due to the high prevalence of Guillain-Barre syndrome and microcephaly in the endemic area, it is vital to confirm the diagnosis of Zika virus. Zika virus infection had been declared as a public health emergency and of international concern by the World Health Organisation. Governments and agencies should play an important role in terms of investing time and resources to fundamentally understand this infection so that a vaccine can be developed besides raising awareness.
Similar content being viewed by others
Introduction
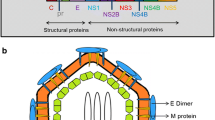
Recent international media attention has focused on microcephaly, which is a potential neurological and immunological complication. Clinical and epidemiological reports showed that there is a link between microcephaly and of Zika virus (ZIKV). ZIKV is a mosquito-borne disease transmissible from human to human through bites of Aedes species. The genome of the ZIKV, of Flaviviridae family and of the Flavivirus genus [1] is a single positive-strand RNA closely related to Spondweni virus [2, 3]. ZIKV was initially distinguished in rhesus monkeys in the Zika forest of Uganda throughout the period of a yellow fever study [3].
Despite its first isolation 6 decades ago, little attention has been given to ZIKV compared with the other mosquito-borne flaviviruses. Only 14 cases of human ZIKV infection had been recognized globally, and no outbreak had been reported until 2007, when ZIKV spread further to the Pacific Island of Yap [4, 5]. This was the first outbreak reported beyond the confines of Africa and Asia [4, 6]. The second and largest outbreak occurred in French Polynesia [7, 8]. With 383 confirmed cases, it is estimated that ZIKV disease may be the reason why approximately 32,000 patients sought medical care between October 2013 and April 2014 [9]. It has only come to international attention recently after the outbreak on Yap Island in 2007 and the current epidemic on Brazil in 2015 [10]. Indigenous dissemination of ZIKV has been detected, as ZIKV infection has been confirmed in 18 states of Brazil [9]. The geographical distribution of ZIKV has steadily broadened given the wide distribution of the mosquito vector. ZIKV infection has been spotted in the USA territories of Puerto Rico, the US Virgin Islands and American Samoa [11–13]. Although mosquito-borne transmission of ZIKV infection has not been reported yet in continental USA, cases of imported ZIKV infection have been reported in pregnant and non-pregnant travellers [14–16]. Figure 1 shows all countries and territories with active ZIKV transmission.
All countries and territories with active Zika virus transmission. As of May 5, 2016, retrieved from Centers for Disease Control and Prevention. http://www.cdc.gov/zika/geo/active-countries.html
This has negatively impacted the safety of other regions, putting them at greater risk, as there is a greater connectivity between the continents as a result of millions of international travellers across the globe. Between 2007 and 2016, 66 countries and territories reported ZIKV transmission. Since 2015, 42 countries are experiencing their first outbreak of ZIKV, with no previous evidence of circulation, and with on-going transmission by mosquitos. Other than a mosquito-borne transmission, eight countries (Argentina, Chile, France, Italy, New Zealand, Peru, Portugal and the United States of America) have reported evidence of person-to-person transmission of ZIKV [17]. Upon scrutinizing the cases reported worldwide, the Central and South American countries could be the most burdened by ZIKV outbreak, because the estimated number of cases reported was around 440,000 to 1,300,000, which is much higher than that in other countries [18, 19]. The prospect of ZIKV spreading across regions and continents, along with neurological disorders can be anticipated from the recent outbreaks [20]. Figure 2 summarizes the timeline of global spread of ZIKV infection
Clinical Presentation
The manifestation of human ZIKV infection ranges from asymptomatic to influenza-like symptoms. Clinical manifestations of infection include fever, headache, retro-orbital pain, arthralgia, asthenia, malaise, myalgia, anorexia, rash, oedema, lymphadenopathy and diarrhoea; in most cases, the infection appeared mild and self-limiting, with a mean symptom duration of 3–6 days [21, 22]. Conjunctivitis is commonly present, whereas arthralgia, headache, and malaise are less prominent. Shock complications and haemorrhagic signs have not been reported. However, Guillain-Barre syndrome, a neurologic complication, was reported in French Polynesia [23]. Laboratory tests revealed transient leukopenia and thrombocytopenia. Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) concentrations may or may not be raised [10]. In 2008, Foy et al. reported two unusual cases of ZIKV infection presenting with aphthous ulcers, prostatitis and hematospermia which are not common [24]. ZIKV infection has been regarded as benign in most cases until the Brazil Ministry of Health considered a link between the ZIKV infection and microcephaly in 2015, with the discovery of the presence of virus in the amniotic fluid of two pregnant women whose foetuses had microcephaly. In the Paraiba state of Brazil, six ZIKV-infected children, who were born to ZIKV-infected mothers during pregnancy, were found to have neonatal head circumferences (HC) below the 10th percentile [25].
Diagnostic Methods
The clinical presentation of ZIKV infection is very similar to that of other arbovirus infections and makes the diagnosis more challenging [26]. In a geographic area where multiple species of flaviviruses circulate, accurate identification of an infecting agent depends upon the diagnostic assay as well as the infection history and immune status of the vertebrate host [27].
Serology Testing
A serological test (ELISA/immunofluorescent) has been used to test the specific anti-Zika immunoglobulin (IgM) in individuals four or more days after the onset of symptoms. However, this method is limited and unspecific, as cross-reactions could occur with other arboviruses within the Flavivirus genus [28]. Earlier studies using this technique did not find many differences of antigenic properties to differentiate ZIKV and other flaviviruses (e.g. DENV, Uganda S, Banzi and Potiskum). Recent studies showed that there are differences comparing the antigenic properties of ZIKV (Uganda and Banzi) with yellow fever (Potiskum and Wesselsbron [4]. This could be caused by a restricted immune response [29]. Hence, a false positive result could be obtained in this serological test.
Furthermore, the concentrations of IgM and IgG are very low during the early phase of infection [4, 29]. The virus-specific IgM antibodies normally can be detected within 3 days of the onset of infection [29, 30] but sometimes can only be detected after 8 days. Hence, it is vital to collect serum from both acute and convalescent phases to confirm the diagnosis of ZIKV infection [29]. Lanciotti et al. reported that a Plaque Reduction Neutralization Test (PRNT) helps to differentiate the cross-reacting antibodies in infection with the primary flavivirus and can improve specificity over immunoassays, although cross-reactive results are still found in secondary flavivirus infections [31]. Drawbacks to serological testing are that it is time-consuming, shows cross-reactivity and is non-specific. The “original antigenic sin” phenomenon is the biggest challenge with serologic cross-reactivity [32]. In a population that has earlier been exposed to a heterologous flavivirus by natural infection or vaccination, the antibody response to the preceding infecting flavivirus will be more vigorous than the current one [33]. Cao-lormeau et al. reported a boost in anamnestic antidengue IgG response in the patients with Guillain-Barré syndrome [23]. This may be due to a substantial antigenic overlap and the ability to undergo antibody-dependent enhancement mechanism. An anamnestic response to ZIKV infection from their yellow fever virus vaccination was also reported [24].
Reverse transcriptase polymerase chain reaction
One-step reverse transcriptase polymerase chain reaction (RT-PCR) allows qualitative detection of ZIKV RNA. RT-PCR is a molecular technology that targets envelope protein-coding region in the early stage of infection [21, 34]. During the first 7 days of the illness, where the acute phase begins with the onset of symptoms, viral RNA is frequently identified in serum; hence, RT-PCR is the favoured test at this stage to detect ZIKV [30].
Saliva and urine can also be used instead of serum as a sample for routine ZIKV RNA detection through RT-PCR [34]. Using saliva increased the ability of molecular detection in the early stages of disease [22], while urine can be used at later stages (>10 days after onset of disease) because there was a higher virus load with an extended period in urine samples relative to serum samples [26]. However, saliva and urine samples cannot replace blood samples and should be considered only when blood collection cannot be performed, especially in children or neonates [34]. Saliva and urine samples are best used together with serum sample to increase the sensitivity of the molecular detection of ZIKV through RT-PCR.
The detection limit to identify ZIKV is low, varying from 103 to 106 pfu/ml in natural human infection, demonstrating the high sensitivity of RT-PCR in detecting ZIKV [21]. This detection limit also rules out the need of modification of the PCR procedure to reduce non-specific binding due to the amplification of unexpected primer binding sites. In addition, the assay’s analytical specificity is assessed utilizing RNA ZIKV isolates and isolates from other related flavivirus. The amplicons of anticipated sequences and sizes are observed only in ZIKV sample, indicating no cross-sensitivity, hence verifying the high specificity of this assay. High sensitivity of RT-PCR makes it clinically helpful by allowing its use for differential diagnosis to distinguish ZIKV from additional clinically related arbovirus infections, including Chikungunya and dengue viruses in endemic areas and areas where they are co-circulating, since the clinical presentation of ZIKV is not very definite [4]. Furthermore, the assay has great repeatability (100 %) in human serum that also demonstrated the robustness of RT-PCR [21]. Due to the several advantages of RT-PCR, this assay is now widely used for ZIKV detection.
Cytokine Profiling: an Indicator of Immunological Response
Cytokine profiling is also another important tool to diagnose Zika fever. During the acute phase of Zika fever, a polyfunctional immune response is activated, as reflected by the increased cytokine levels associated with T helper subsets, Th1, Th2, Th9 and Th17 [10].
Table 1 shows the types of cytokines increase during acute and reconvalescent phases of Zika fever, as well as cytokines with no significant changes in both phases. The elevation of chemokines such as RANTES, MIP-1α and VEGF was more pronounced than the elevation of inflammatory cytokines in Zika fever patients [10]. Moreover, most cytokines (other than IL-1β, IL-8, IL-10, IP-10, MIP-1β and GM-CSF) will generally decrease in the reconvalescent phase compared to acute phase. The level of cytokines is important to distinguish dengue fever from Zika fever during the acute and reconvalescent phases. The differences between Zika fever, dengue fever and Chikungunya in terms of symptoms associated with level of certain kinds of cytokines are listed in Table 2 [10, 35–41].
Misdiagnosis with Dengue/Chikungunya
Many ZIKV infection cases have been misdiagnosed or unreported because its non-specific clinical presentation is easily confused with that of other arboviruses, particularly Chikungunya and dengue infection [42, 43]. In addition, serologic cross-reactivity of ZIKV antibodies with dengue virus (DENV) also contributes to the misdiagnosis [24]. According to Lanciotti et al., IgM assay for DENVs showed a great extent of cross-reactivity in patients with ZIKV infections, which could lead to the wrong diagnosis of dengue being the cause of the infection [44]. A case report by Kwong et al. showed that a ZIKV-infected patient was provisionally given a diagnosis of dengue fever due to the dengue serologic analysis showing a positive result for IgM as well as IgG [43]. ZIKV-specific tests have not yet been developed, and non-availability of commercial tests for ZIKV infection making diagnosis of ZIKV infection a challenge [45]. Therefore, expansion of ZIKV emphasizes the need to develop a reliable, sensitive and specific tool to detect the virus accurately. Plans to provide treatment in affected patients can be accelerated with the rapid detection of the virus in specimens.
Modes of Transmission of ZIKV
ZIKV is mainly transmitted through bites from Aedes aegypti mosquito [46, 47]. Additionally, the transmission can be perinatal, as well as by close physical contact between the newborn babies and their mothers [48, 49].
Perinatal Transmission
Substantial evidence now indicates that ZIKV can be transmitted from the mother to the foetus during pregnancy. In mothers whose foetuses had cerebral abnormalities detected by ultrasonography, ZIKV RNA has been identified in their amniotic fluid [50–52], and viral antigen and RNA have been identified in the brain tissue and placentas of children who were born with microcephaly and died soon after birth as well as in tissues from miscarriages [52, 53]. The frequency of and risk factors for transmission are unknown. Perinatal transmission of ZIKV can occur, most probably transplacental or during the delivery of a viraemia mother [48, 54, 55]. A study by Besnard et al. reported two cases of ZIKV infection for infants most probably occurred by transplacental transmission or during delivery [48]. The Brazilian ministry of health reported the presence of ZIKV RNA in amniotic fluid samples of two pregnant women, whose foetuses showed microcephaly. On December 2015, the Brazilian ministry of health reported the presence of the ZIKV genome in the blood and tissue samples of a baby from the state of Parà with microcephaly. The newborn presented microcephaly and other congenital anomalies and died within 5 min of being born. Mlakar et al. further supported the association between ZIKV infection and microcephaly, demonstrating severe foetal brain injury in a case of vertically acquired ZIKV infection [56].
Vertical ZIKV Transmission
Although no replicative ZIKV particles were detected in breast milk, a high ZIKV RNA load detected in breast milk is an area of concern [48]. However, currently, there is no evidence that Zika can be transmitted to babies through breast milk [57]. Mothers in areas with Zika circulation should consider breastfeeding for the infant and mother, as no potential risk of ZIKV transmission through breast milk has been reported. If required, feeding support by skilled breastfeeding counsellors should be provided in line with WHO recommendations [58].
Sexual transmission of ZIKV infection from the infected male partner has been reported [24, 59, 60]. High copy numbers of replicative viral particles have been identified in sperm with viral RNA up to 62 days after the onset of symptoms [61–63]. Therefore, there is a possibility of infection with ZIKV through sexual transmission even after recovery, as suggested by the high RNA load of ZIKV and its replicable virus in both semen and urine of a man presenting with hematospermia [47]. However, transmission of ZIKV from an infected woman to her sexual partner has not been reported [47, 48, 64]. In particular, vertical transmission of ZIKV needs to be concretely demonstrated as well as any direct or indirect effects of infection of ZIKV.
Target Cells for ZIKV Tropism
Transmission of ZIKV is majorly by the infected vector, Aedes aegypti mosquito. The vector inoculates ZIKV into human by allowing the deposition of ZIKV in the epidermis and dermis layers of the skin [65, 66]. Epidermal keratinocytes and skin fibroblasts are highly susceptible to ZIKV [65]. The infected skin fibroblasts show rapid and active viral replication. ZIKV induces autophagy, an intracellular process by which cytoplasmic constituents are recruited in double-membrane vesicles and afterwards fuse with lysosomes for protein degradation in experimentally infected skin fibroblasts [65, 67]. This suggests that ZIKV could hijack the autophagy pathway and utilize the components of this biological pathway for replication; this is true for several flavivirus [65, 67, 68]. In addition, ZIKV-infected epidermal keratinocytes were observed to undergo apoptosis, which is also similarly found in dengue-infected human skin explants [65]. It is postulated that ZIKV deters anti-viral immune responses by triggering apoptotic cell death of infected cells, resembling DENV’s mechanism, thereby enhancing viral dissemination from dying cells. Another promising target of ZIKV is dendritic cells [65]. This may be due to flavivirus’ replication involving skin antigen-presenting cells, of which dendritic cells are an example [65, 69].
ZIKV was shown to be highly neurotropic in intraperitoneally inoculated mice [70]. Brains of infected mice showed neuronal degeneration, cellular infiltration and softening in certain areas. This suggested that ZIKV has the potential to cross the blood-brain barrier, albeit through unknown mechanism(s). Bell et al. reported that neural cells are involved in the infection of ZIKV [71]. Coinciding with the ZIKV outbreak, an increased number of newborns with microcephaly were observed in several regions of Brazil [72, 73]. This is also coupled with the fact that mothers and amniotic fluid samples from foetuses revealed positive results for ZIKV RNA. Thus, the virus could have the potential to trigger neurodevelopmental dysfunction, as well as microcephaly [46]. More studies are needed to provide a platform to determine whether the virus is involved (directly or indirectly) in microcephaly.
Microcephaly Causality by ZIKV
Among the 7150 cases of microcephaly and/or CNS malformation reported in Brazil, 246 child deaths occurred after birth or during pregnancy (including miscarriage or stillbirth) [46]. EI Salvador recorded 178 Guillain-Barre syndrome cases from 5 December 2015 to 22 March 2016, including five deaths, while the annual average number of Guillain-Barre syndrome cases is 169 [74].
Potential Targets for Therapeutic Antiviral Strategies
In order to enter the host cell, ZIKV’s viral envelope protein needs to interact with various receptors on the cell surface and attachment factors, of all which will determine the viral cellular tropism. Several receptors, including dendritic cell-specific ICAM-3-grabbing non-integrin (DC-SIGN) encoded by CD209, AXL, Tyro3 and transmembrane immunoglobulin and mucin domain (TIM)-1 (encoded by HAVCR1), have been suggested as ZIKV receptors. These different entry receptors provide an evolutionary advantage for ZIKV to infect a wide range of target cells and invade the human host [65]. Among the abundant surface receptors available, C-type lectin receptors (CLR), TIM proteins and TAM proteins (standing for Tyro3, AXL and Mer) are important to facilitate the entry.
DC-SIGN, categorized under CLRs, offers a significant link between viral replication and host infection. DC-SIGN is constitutively expressed in dendritic cells that may reside in the skin, the site of initial infection [66]. Being an essential host factor, it could be exploited by ZIKV to penetrate and infect the immature dendritic cells [65, 66].
Hamel et al. reported that TAM proteins (namely AXL and Tyro3) mediate ZIKV entry into the host cell [65]. As cutaneous fibroblasts and epidermal keratinocytes express AXL, this further supports the susceptibility of these cells to ZIKV infection. Astrocytes and microglial cells are known to have AXL and Tyro3 expression [75]. Therefore, astrocytes and microglial cell could be targets for ZIKV infection. These cells can be found within the spinal cord and most importantly, the brain. With the possible capability of ZIKV crossing the blood–brain barrier, it could target astrocytes and microglia within the brain and trigger the infection there. Hence, this could be a possible pathway necessary for microcephaly.
TIM-1 (a TIM protein) contributes the least to ZIKV infection when compared to DC-SIGN and TAM proteins [65]. Its expression, nonetheless, increases the efficacy of AXL-mediated viral entry. With the potential function as an attachment factor, TIM-1 could bind to viral particles and concentrate ZIKV on the cell surface [65]. TIM-1 could then transfer the viral particles to AXL, facilitating ZIKV interaction with AXL. Since ZIKV’s entry into target cells is the main key factor of viral pathogenesis and cellular tropism, it becomes the potential target in preventive measures and therapeutic antiviral therapy.
Management and Prevention
The mainstays of management include supportive care and bed rest, along with advice to prevent dehydration [45]. Treatments providing symptomatic relief include combining paracetamol and antihistamines for pruritic rash [7, 18]. ZIKV infection shares similar clinical features with DENV infection. Before dengue infection is ruled out, non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided, as they are contraindicated in dengue fever, where they may produce an increased risk of haemorrhagic syndrome [7]. In addition, specific viral diagnosis is essential in managing and preventing complications, especially when there is co-circulating of multiple arboviruses [45].
Vaccines Availability
To date, there are no vaccines or antiviral therapy available for ZIKV [45, 76]. There are successful vaccines for some of the flavivirus infections (dengue, Japanese encephalitis and yellow fever). The earlier success in developing vaccines for flaviviruses infections is a positive sign of a possible vaccine candidate for ZIKV. GloPID-R members coordinate research on Zika through working groups on vaccines [77]. There is much ongoing research on preclinical vaccine development, and the first phase I clinical trials in humans are expected at the end of 2016. A plasmid DNA vaccine is undergoing preclinical evaluation now and is planned to enter phase I clinical trial in Q4 of 2016 [77]. A DNA Zika vaccine candidate has been tested for its potency in a mouse model, and its efficacy is yet to be tested [78]. An inactivated and a recombinant Zika vaccine candidate is currently undergoing testing in an animal model, and clinical phase I studies are planned to start before the end of 2016 [79].
A recent computational approach has identified Zika viral envelope glycoproteins as a good candidate for vaccine development, as these are the most immunogenic [80]. Nonetheless, it is predicted that Zika vaccines, if available, would face problems similar to Chikungunya vaccines. For instance, the vaccine would be prohibitively expensive, and deployment of vaccines following any rapid outbreak may be too slow to counter the explosive epidemic. This is mostly because epidemics usually appear unexpectedly and sporadically [45].
Destruction of Mosquito-Bite Breeding Sites
Air-conditioning, house screens and minimizing mosquitoes-breeding sites are considered as the best available preventive measures against ZIKV [45, 81]. Aquatic environments, for instance open water storage containers and small puddles, are known as their common breeding sites [5]. In order to destroy the breeding sites, larvicides can be used on natural and peridomestic breeding sites. If larvicides fail, the density of adult mosquitoes can be reduced through space spraying with pyrethroids [82]. Deltamethrin is currently the only satisfactorily effective pyrethroids insecticides [18, 21].
Reduction of Urban Mosquito-Human Transmission
In order to reduce disease burden, reductions in urban mosquito-human transmission seem to be the only option [83]. Since 80 % of infected individuals are asymptomatic, mosquito bites avoidance such as personal protection helps to disrupt human-to-mosquito-to-human transmission cycles [76]. Avoidance of mosquito bites in daytime is crucial as Aedes mosquitoes, being the most active near dawn and dusk, are adapted for daytime biting in urban areas [5, 81]. Using insect repellent, mosquito bed nets and wearing light-coloured clothes with long sleeves [18, 45, 81], and insecticide such as permethrin spray on clothing [84] are some useful methods to avoid mosquito bites. There are also alternative strategies available such as reduction of human-to-vector contact with insect repellents, biologic control (e.g., bio-insecticides use) and genetic control [82, 85]. For genetic control, the genetically modified mosquitoes are either sterile or have lost the ability to transmit diseases to humans [82, 86]. However, the control methods mentioned have their weaknesses such as funding and difficulties their application over a sufficiently wide area [86]. Community-level vector surveillance and disease surveillance enhanced earlier case detection, and thus appropriate control measures can be implemented [76].
Travel Precautions
People who have travelled to or reside in endemic areas of ZIKV infection are under possible exposure to ZIKV. Therefore, it is important to provide health education to the people at risk. Travellers are advised to take extra precautions when travelling to the areas with active ZIKV transmission. The precautions suggested include using insect repellent and sleeping under a mosquito net. The most recommended insect repellents are those containing N,N-diethyl meta toluamide (DEET) as it is safe to be used, even in pregnant and breastfeeding women [84]. As described earlier, there is an association between ZIKV and microcephaly, and some countries such as the UK and the USA have issued travel advice to their citizens that pregnant women should avoid travelling to zones where active ZIKV transmission is enduring [76, 84]. If they must travel to the endemic area, they should be assessed and monitored appropriately during antenatal visits [9]. Travellers returning from an area with ZIKV-infected area should be kept under surveillance at least for a month for any symptoms of ZIKV infection [87]. After coming back from the endemic areas, women, who are willing to conceive, should avoid getting pregnant for a further 28 days, which allows a maximum 2 weeks of the ZIKV incubation period and a possible 2-week viraemia. It is ideal to wait 2–3 months for women after their return from endemic areas of ZIKV infection [88, 89].
ZIKV can be transmitted sexually from men to women. A man who lives in or has recently travelled to the endemic areas of ZIKV infection can spread ZIKV infection to his sex partners as the virus persists in semen 2 weeks of post-symptomatic periods, when viremia is not present in the patient blood [34]. From the cases reported earlier, it is very clear that the ZIKV can be spread during the infected period and pre- or post-symptomatic period. Thus, if a man has recently travelled to the endemic areas, effective contraception should be used for at least 28 days [84]. They should consider the use of condoms during sex with their pregnant or non-pregnant partners.
Prevention of Blood Donor Transmission of ZIKV
The theme of blood donation “Blood connects us all” explains how much it is a critical need for health care. At the same time, blood safety should be considered as the donated blood carries the risk of transmitting infectious diseases from the donor to recipient. Viral inactivation and removal methods which are effectively clearing lipid-enveloped viruses in plasma-derived products can be used in plasma and plasma products. However, it is not applicable for the blood and blood products. A newly approved device (amotosalen + UV illumination) to reduce pathogen in plasma and platelets has reduced panel of viruses, including ZIKV and other flaviviruses [90, 91]. The pathogen-reduction technology also has been reported to reduce ZIKV in plasma [86]. However, these methods are capable of adequate reduction of levels of flavivirus in plasma and platelets but are not applicable for red blood cells.
ZIKV is a high-risk agent that threatens the safety of blood recipients. In the past, the transfusion-transmissions of dengue virus, West Nile virus and yellow fever virus which belong to the flavivirus genome have been reported [26, 92, 93]. In French Polynesia, 3 % of samples from asymptomatic blood donors contained detectable ZIKV RNA [94, 95]. Blood donor transmission of ZIKV is very much possible because of the variation in the pre-symptomatic period from 3 to 12 days [18, 96]. Moreover, 80 % of ZIKV infections remain asymptomatic [52, 94]. Therefore, donors may not be aware of their ZIKV infection.
Recent travel to or residence in areas with local ZIKV will make any individual susceptible to infection with ZIKV. Therefore, a potential donor’s travel history is very important to find out the possibility of ZIKV infection. Special educational material on ZIKV with a questionnaire asking about travel history and health history before donating blood will help to get more information from the potential donors. If potential donors have recently been infected by ZIKV or have any symptoms of ZIKV infection such as fever or rash with pinkeye, along with muscle aches, headache or malaise, they should be excluded from blood donation. They should wait at least 28 days, (twice the assumed maximum incubation period [18]) following the full resolution of symptoms to donate their blood.
Prevention of transfusion-transmitted ZIKV includes nucleic acid testing (NAT) of blood donors (albeit not routinely available) and pathogen inactivation, of which the latter abolishes pathogen infectivity in blood products [57]. NAT reduces risk of transfusion-transmitted infections by providing an additional layer of blood safety through screening blood donations. It detects the viral nucleic acids earlier and specifically by amplifying the targeted region of viral ribonucleic acid or deoxynucleic acid (DNA) [97].
Need for ZIKV Research
ZIKV infection and its association with neurological damage in neonates and Guillain-Barre syndrome have made this infectious disease more dangerous [98]. Ultimately, more research is urgently needed on ZIKV including vaccination to control arbovirus spread. A worldwide collaborative research should be conducted to address identified research gaps [99]. A comprehensive understanding of the occurrence of foetal ZIKV infection and knowing the full spectrum of its clinical outcomes is very important. Areas such as environmental factors that influence ZIKV emergence, development of discriminating diagnostic tools, animal models, new vector control products and strategies, effective therapeutics and vaccines to protect humans against the disease should be the focus [100]. In managing this arbovirus pandemic, it is suggested that broad-spectrum antiviral drug which is effective in covering a whole class of virus is also required with respect to treatment [48].
Future interventions will enhance health security and improve international public health capacity. The global health community of researchers should develop a framework of principles by themselves to improve international public health capacity for sharing data and biologic samples during any such public health emergency [101]. Key interventions such as appropriate clinical care and prevention of ZIKV transmission through sexual contact or blood transfusion need to be strengthened [102]. Some asymptomatic individuals and mild cases may hinder control measures and spread the disease to others without being identified [97]. Therefore, all people, irrespective of their region of living, must be informed of the potential current and future risks of ZIKV transmission and its associated neurologic disorders [103].
Roles of Healthcare Professionals
The current ZIKV pandemic is affecting more and more countries and spreading as much as possible [97, 104]. Healthcare professionals (especially clinicians) have a significant role in the early diagnosis of ZIKV infection, and they are encouraged in notifying the suspected cases to public health authorities [28]. If done in a timely fashion, this will facilitate the mitigation of local transmission in regions where Aedes mosquitoes are found [105]. Rapid dissemination of key information is crucial in terms of raising awareness to the public on ZIKV prevention. In light of this, healthcare professionals should get involved in public education, emphasizing the importance of preventing mosquito bites in at-risk individuals, especially pregnant women [28]. It is of utmost importance for healthcare professionals to be alert about the evolution of ZIKV outbreaks, especially those in popular tourist destinations so that clinicians would include ZIKV in their differential diagnosis [9, 28]. They should counsel women with possible ZIKV virus exposure who are interested in conceiving. The male partner also needs to be counselled and to be enquired about his travel history and any symptoms of ZIKV infection. Moreover, healthcare professionals would be able to consult travellers who are planning to visit endemic countries on effective preventive measures [18, 58].
During diagnosis, differential clinical diagnostic test must be applied as it is important to rule out other mosquito-borne infectious diseases such as dengue and Chikungunya. In addition, clinicians should be aware of the neurological complications of this infection, including inflammatory-autoimmune neurological syndromes (e.g., Guillain-Barré syndrome and its variants, encephalitis, transverse myelitis and foetal abnormalities in pregnant women). In Venezuela, 76 % Guillain-Barré syndrome cases indicated a clinical history of ZIKV infection. In three patients, ZIKV was detected using polymerase chain reaction [106]. A recent report on ocular abnormalities in ZIKV-infected infants (34.5 %) should also be considered by the clinicians [107]. It is essential for the clinician to understand that congenital infection presumed to be linked to ZIKV (ZIKV congenital syndrome) may be associated with microcephaly and other malformations [108].
Conclusion
The peer-reviewed literature demonstrates that the growing importance of developing a reliable, specific and rapid diagnostic device to detect ZIKV, as it is often recognized as a mild disease without being identified. In the absence of ZIKV vaccine, other control measures are especially important to be implemented, predominantly by combating vector mosquito and preventing mosquito bites. For a vector control program to be effective, it must be based on the extensively analysed entomological and ecologic surveillance data to understand the time and viral emergence location. ZIKV danger seems confined to pregnant women, as it shows a close association with the startling rise in microcephaly, a severe birth defect. This critical fact of ZIKV infection as a public health emergency emphasizes the urgent need of global attention and concern. Lessons learned from the Ebola epidemic concerning the importance of rapid key information dissemination serve as a reminder to stress the need for an urgent global effort to galvanize resources in understanding more about the disease.
References
Zanluca C, de Melo VC, Mosimann AL, Dos Santos GI, Dos Santos CN, Luz K (2015) First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz 110:569–572
Kuno G, Chang GJ (2007) Full-length sequencing and genomic characterization of Bagaza, Kedougou, and Zika viruses. Arch Virol 152:687–696
Campos GS, Bandeira AC, Sardi SI (2015) Zika Virus Outbreak, Bahia, Brazil. Emerg Infect Dis 21:1885–1886
Shapshak P, Sinnott JT, Somboonwit C, Kuhn J (2015) Global virology I -Identifying and Investigating Viral Disease. Springer, New York
Rodriguez-Morales AJ (2015) Zika: the new arbovirus threat for Latin America. J Infect Dev Ctries 9:684–685
Hayer EB (2009) Zika virus outside Africa 15:1347–1350
Musso D, Nhan TX (2015) Emergence of Zika Virus. Clin Microbiol 4:222. doi:10.4172/2327-5073.1000222
Tognarelli J, Ulloa S, Villagra E, Lagos J, Aguayo C, Fasce R et al (2014) A report on the outbreak of Zika virus on Easter Island, South Pacific. Arch Virol 161:665–668
European Centre for Disease Prevention and Control (2016) Rapid Risk Assessment. Zika virus disease epidemic: potential association with microcephaly and Guillain–Barré syndrome. Second update. Stockholm http://ecdc.europa.eu/en/publications/ Publications/zika-virus-americas-association-with-microcephaly-rapid-risk-assessment.pdf
Tappe D, Perez-Giron JV, Zammarchi L, Rissland J, Ferreira DF, Jaenisch T et al (2015) Cytokine kinetics of Zika virus-infected patients from acute to reconvalescent phase. Med Microbiol Immunol. doi:10.1007/s00430-015-0445-7
Centers for Disease Control and Prevention. CDC Newsroom. First case of Zika virus reported in Puerto Rico. http://www.cdc.gov/media/releases/2015/s1231-zika.html
Centers for Disease Control and Prevention. Zika Travel Information. Zika Virus in the Caribbean. http://wwwnc.cdc.gov/travel/notices/alert/zika-virus-caribbean
Thomas DL, Sharp TM, Torres J, Armstrong PA, Munoz-Jordan J, Ryff KR et al (2016) Local Transmission of Zika Virus - Puerto Rico. MMWR Morb Mortal Wkly Rep 65:154–158
Meaney-Delman D, Hills SL, Williams C, Galang RR, Iyengar P, Hennenfent AK et al (2016) Zika Virus Infection Among U.S. Pregnant Travelers - August 2015-February 2016. MMWR Morb Mortal Wkly Rep 65:211–214
Centers for Disease Control and Prevention. Zika virus disease in the United States, 2015–2016. http://www.cdc.gov/zika/geo/united-states.html
Armstrong P, Hennessey M, Adams M, Cherry C, Chiu S, Harrist A, et al. (2016). Travel-associated Zika virus disease cases among U.S. Residents - United States, January 2015-February 2016. MMWR Morb Mortal Wkly Rep 65:286.
Zika Virus Microcephaly And Guillain-Barré Syndrome Situation Report 21 APRIL 2016. http://apps.who.int/iris/bitstream/10665/205505/1/zikasitrep_21Apr2016_eng.pdf?-ua=1
Ioos S, Mallet HP, Leparc Goffart I, Gauthier V, Cardoso T, Herida M (2014) Current Zika virus epidemiology and recent epidemics. Med Mal Infect 44:302–307
The Lancet (2016) Zika virus: a new global threat for 2016. Lancet 387:96. doi:10.1016/S0140-6736(16)00014-3
Kindhauser MK, Allen T, Frank V, Santhana RS, Dye C (2016) Zika: the origin and spread of a mosquito-borne virus. Bull World Health Organ. http://www.who.int/bulletin/online_first/16-171082.pdf
Faye O, Faye O, Dupressoir A, Weidmann M, Ndiaye M, Alpha Sall A (2008) One-step RT-PCR for detection of Zika virus. J Clin Virol 43:96–101
Kutsuna S, Kato Y, Takasaki T, Moi M, Kotaki A, Uemura H et al (2014) Two cases of Zika fever imported from French Polynesia to Japan, December 2013 to January 2014. Euro Surveill 19:20683
Cao-Lormeau VM, Blake A, Mons S, Lastère S, Roche C, Vanhomwegen J et al (2016) Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case–control study. Lancet 387:1531–1539
Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da Rosa A, Haddow AD et al (2011) Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis 17:880–882
Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de Filippis AM (2016) Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol 47:6–7
Gourinat AC, O’Connor O, Calvez E, Goarant C, Dupont-Rouzeyrol M (2015) Detection of Zika Virus in Urine. Emerg Infect Dis 21:84–86
Ledermann JP, Lorono-Pino MA, Ellis C, Saxton-Shaw KD, Blitvich BJ, Beaty BJ et al (2011) Evaluation of Widely Used Diagnostic Tests To Detect West Nile Virus Infections in Horses Previously Infected with St. Louis Encephalitis Virus or Dengue Virus Type 2. Clin Vaccine Immunol 18:580–587
Zammarchi L, Stella G, Mantella A, Bartolozzi D, Tappe D, Gunther S et al (2015) Zika virus infections imported to Italy: clinical, immunological and virological findings, and public health implications. J Clin Virol 63:32–35
Hayes EB (2009) Zika virus outside Africa. Emerg Infect Dis 15:1347–1350
Revised diagnostic testing for Zika, Chikungunya, and dengue viruses in US Public Health Laboratories (2016) http://www.cdc.gov/zika/pdfs/denvchikvzikv-testing-algorithm.pdf
Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ et al (2008) Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis 14:1232–1239
Morens DM, Burke DS, Halstead SB (2010) The wages of original antigenic sin. Emerg Infect Dis 16:1023–1024
Johnson BW, Kosoy O, Martin DA, Noga AJ, Russell BJ, Johnson AA et al (2005) West Nile virus infection and serologic response among persons previously vaccinated against yellow fever and Japanese encephalitis viruses. Vector Borne Zoonotic Dis 5:137–145
Musso D, Roche C, Nhan TX, Robin E, Teissier A, Cao-Lormeau VM (2015) Detection of Zika virus in saliva. J Clin Virol 68:53–55
Guabiraba R, Ryffel B (2014) Dengue virus infection: current concepts in immune mechanisms and lessons from murine models. Immunology 141:143–156
Mathew A, Rothman AL (2008) Understanding the contribution of cellular immunity to dengue disease pathogenesis. Immunol Rev 225:300–313
Rathakrishnan A, Wang SM, Hu Y, Khan AM, Ponnampalavanar S, Lum LC et al (2012) Cytokine expression profile of dengue patients at different phases of illness. PLoS ONE 7:e52215
Wauquier N, Becquart P, Nkoghe D, Padilla C, Ndjoyi-Mbiguino A, Leroy EM (2011) The Acute Phase of Chikungunya Virus Infection in Humans Is Associated With Strong Innate Immunity and T CD8 Cell Activation. J Infect Dis 204:115–123
Ng LF, Chow A, Sun YJ, Kwek DJ, Lim PL, Dimatatac F et al (2009) IL-1beta, IL-6, and RANTES as biomarkers of Chikungunya severity. PLoS ONE 4:e4261
Fried JR, Gibbons RV, Kalayanarooj S, Thomas SJ, Srikiatkhachorn A, Yoon IK et al (2010) Serotype-specific differences in the risk of dengue hemorrhagic fever: an analysis of data collected in Bangkok, Thailand from 1994 to 2006. PLoS Negl Trop Dis 4:e617
Balmaseda A, Hammond SN, Perez L, Tellez Y, Saborio SI et al (2006) Serotype-specific differences in clinical manifestations of dengue. Am J Trop Med Hyg 74:449–456
Faye O, Faye O, Diallo D, Diallo M, Weidmann M, Sall AA (2013) Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol J 10:311
Kwong JC, Druce JD, Leder K (2013) Zika virus infection acquired during brief travel to Indonesia. Am J Trop Med Hyg 89:516–517
Johnson AJ, Noga AJ, Kosoy O, Lanciotti RS, Johnson AA, Biggerstaff BJ (2005) Duplex microsphere-based immunoassay for detection of anti-West Nile virus and anti-St. Louis encephalitis virus immunoglobulin m antibodies. Clin Diagn Lab Immunol 12:566–574
Fauci AS, Morens DM (2016) Zika Virus in the Americas--Yet Another Arbovirus Threat. N Engl J Med 374:601–604
Tetro JA (2016) Zika and microcephaly: causation, correlation, or coincidence? Microbes Infect 18:167–168
Oster AM, Brooks JT, Stryker JE, Kachur RE, Mead P, Pesik NT et al (2016) Interim Guidelines for Prevention of Sexual Transmission of Zika Virus-United States 2016. MMWR Morb Mortal Wkly Rep 65:120–121
Besnard M, Lastere S, Teissier A, Cao-Lormeau V, Musso D (2014) Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill 19:20751
Triunfol M (2016) A new mosquito-borne threat to pregnant women in Brazil. Lancet Infect Dis 16:156–157
Hennessey M, Fischer M, Staples JE. Zika virus spreads to newareas-region of the Americas, May 2015–January 2016. www.cdc.gov/mmwr/volumes/65/wr/mm6503e1er.htm
Calvet G, Aguiar RS, Melo AS, Sampaio SA, de Filippis I, Fabri A et al (2016) Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. doi:10.1016/S1473-3099(16)00095-5
Meaney-Delman D, Hills SL, Williams C, Galang RR, Iyengar P, Hennenfent AK (2016) Zika virus infection among U.S. pregnant travellers-August 2015–February 2016. MMWR Morb Mortal Wkly Rep 65:211–214
Martines RB, Bhatnagar J, Keating MK, Silva-Flannery L, Muehlenbachs A, Gary J (2016) Notes from the field: evidence of Zika virus infection in brain and placental tissues from two congenitally infected newborns and two fetal losses — Brazil, 2015. MMWR Morb Mortal Wkly Rep 65:159–160
Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS et al (2009) Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med 360:2536–2543
Simpson DI (1964) Zika Virus Infection in Man. Trans R Soc Trop Med Hyg 58:335–338
Mlakar J, Korva M, Tul N, Popović M, Poljšak-Prijatelj M, Mraz J et al (2016) Zika Virus Associated with Microcephaly. N Engl J Med 374:951–958
PAHO Statement on Zika Virus Transmission and Prevention Updated: 2 February 2016, http://www.paho.org/hq/index.php?option=com_content&view=article&id=11605&Itemid=41716&lang=en
World Health Organization; UNICEF (1993) Breastfeeding counselling: a training course. World Health Organization, Geneva
Hills SL, Russell K, Hennessey M, Williams C, Oster AM, Fischer M et al (2016) Transmission of Zika virus through sexual contact with travelers to areas of ongoing transmission-continental United States, 2016. MMWR Morb Mortal Wkly Rep 65:215–216
Venturi G, Zammarchi L, Fortuna C, Remoli ME, Benedetti E, Fiorentini C et al (2016) An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill 21:30148. doi:10.2807/1560-7917.ES.2016.21.8.30148
Musso D, Roche C, Robin E, Nhan T, Teissier A, Cao-Lormeau VM (2015) Potential sexual transmission of Zika virus. Emerg Infect Dis 21:359–361
Atkinson B, Hearn P, Afrough B, Lumley S, Carter D, Aarons EJ et al. (2016) Detection of Zika virus in semen [letter]. Emerg Infect Dis. doi:http://dx.doi.org/10.3201/eid2205.160107
Mansuy JM, Dutertre M, Mengelle C, Fourcade C, Marchou B, Delobel P et al (2016) Zika virus: high infectious viral load in semen, a new sexually transmitted pathogen? Lancet Infect Dis 16:405
Goorhuis A, von Eije KJ, Douma RA, Rijnberg N, van Vugt M, Stijnis C et al (2016) Zika virus and the risk of imported infection in returned travelers: implications for clinical care. Travel Med Infect Dis 14:13–15
Hamel R, Dejarnac O, Wichit S, Ekchariyawat P, Neyret A, Luplertlop N et al (2015) Biology of Zika Virus Infection in Human Skin Cells. J Virol 89:8880–8896
Fernandez-Garcia MD, Mazzon M, Jacobs M, Amara A (2009) Pathogenesis of flavivirus infections: using and abusing the host cell. Cell Host Microbe 5:318–328
Blazquez AB, Escribano-Romero E, Merino-Ramos T, Saiz JC, Martin-Acebes MA (2014) Stress responses in flavivirus-infected cells: activation of unfolded protein response and autophagy. Front Microbiol 5:266
McLean JE, Wudzinska A, Datan E, Quaglino D, Zakeri Z (2011) Flavivirus NS4A-induced autophagy protects cells against death and enhances virus replication. J Biol Chem 286:22147–22159
Schmid MA, Diamond MS, Harris E (2014) Dendritic cells in dengue virus infection: targets of virus replication and mediators of immunity. Front Immunol 5:647
Dick GW (1952) Zika virus. II. Pathogenicity and physical properties. Trans R Soc Trop Med Hyg 46:521–534
Bell TM, Field EJ, Narang HK (1971) Zika virus infection of the central nervous system of mice. Arch Gesamte Virusforsch 35:183–193
Fact sheet, Zika Virus (2016) http://www.who.int/mediacentre/factsheets/zika/en/.
Martines R, Bhatnagar J, Keating M, Silva-Flannery L (2016) Notes from the field: evidence of zika virus infection in brain and placental tissues from two congenitally infected newborns and two fetal losses—Brazil, 2015. MMWR Morb Mortal Wkly Rep 65:159–160
Zika Virus Microcephaly and Guillain - Barré Syndrome Situation Report 21 APRIL 2016. http://apps.who.int/iris/bitstream/10665/205505/1/zikasitrep_21Apr2016_eng.pdf?ua=1
Ji R, Tian S, Lu HJ, Lu Q, Zheng Y, Wang X et al (2013) TAM receptors affect adult brain neurogenesis by negative regulation of microglial cell activation. J Immunol 191:6165–6177
Bogoch II, Brady OJ, Kraemer MU, German M, Creatore MI, Kulkarni MA et al (2016) Anticipating the international spread of Zika virus from Brazil. Lancet 387:335–336
http://www.bharatbiotech.com/media/press-release/?prsyear=2016
Shawan MMAK, Hossain MM, Hasan MA, Hasan MM et al (2015) Design and prediction of potential RNAi (siRNA) molecules for 3' UTR PTGS of different strains of zika virus: a computational approach. Nat Sci 13:37–50
Kelser EAC (2015) Meet dengue's cousin, Zika. Microbes Infect 18:163–166
Ngoagouni C, Kamgang B, Nakoune E, Paupy C, Kazanji M (2015) Invasion of Aedes albopictus (Diptera: Culicidae) into central Africa: what consequences for emerging diseases? Parasit Vectors 8:191
Weaver SC (2013) Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends Microbiol 21:360–363
Zika Virus Infection and Pregnancy Information for Healthcare Professionals. Interim RCOG/RCM/PHE/HPS clinical guidelines. 2016; Available at: https://www.rcog.org.uk/globalassets/documents/news/zika-virus-interim-guidelines.pdf
Paupy C, Delatte H, Bagny L, Corbel V, Fontenille D (2009) Aedes albopictus, an arbovirus vector: from the darkness to the light. Microbes Infect 11:1177–1185
Aubry M, Richard V, Green J, Broult J, Musso D (2016) Inactivation of Zika virus in plasma with amotosalen and ultraviolet A illumination. Transfusion 56:33–40
CDC Health Alert Network (2016) Emergency Preparedness and Response Recognizing, Managing, and Reporting Zika Virus Infections in Travelers Returning from Central America, South America, the Caribbean, and Mexico. http://emergency.cdc.gov/han/han00385.asp
Committee to Advise on Tropical Medicine and Travel. Canadian Recommendations on the Prevention and Treatment of Zika Virus. Public Health Agency of Canada 2016 http://www.healthycanadians.gc.ca/publications/diseases-conditionsmaladies-affections/committee-statement-treatment-prevention-zika-declaration-comitetraitement-prevention/index-eng.php
Petersen EE, Polen KN, Meaney-Delman D, Ellington SR, Oduyebo T, Cohn A et al (2016) Update: interim guidance for health care providers caring for women of reproductive age with possible Zika virus exposure—United States, 2016. MMWR Morb Mortal Wkly Rep 65:315–22
FDA News Release: FDA approves pathogen reduction system to treat platelets, (2014) http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm427500.htm
Jacobs MR, Lazarus HM, Maitta RW (2015) The Safety of the Blood Supply-Time to Raise the Bar. N Engl J Med 372:1882–1885
Chuang V, Wong TY, Leung YH, Ma E, Law YL, Tsang O et al (2008) Review of dengue fever cases in Hong Kong during 1998 to 2005. Hong Kong Med J 14:170–177
Centers for Disease Control and Prevention (CDC) (2010) Transfusion-related transmission of yellow fever vaccine virus-California, 2009. MMWR Morb Mortal Wkly Rep Yellow Fever 59:34–37
Musso D, Nhan T, Robin E, Roche C, Bierlaire D, Zisou K et al (2014) Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill 19:20761
Aubry M, Finke J, Teissier A, Roche C, Broult J, Paulous S et al (2015) Seroprevalence of arboviruses among blood donors in French Polynesia, 2011–2013. Int J Infect Dis 41:11–12
European Centre for Disease Prevention and Control (ECDC) Rapid risk assessment: Zika virus infection outbreak, Brazil and the Pacific region – 25 May 2015. Stockholm: ECDC; 2015 http://ecdc.europa.eu/en/publications/Publications/rapid-risk-assessmentZika%20virus-south-america-Brazil-2015.pdf
Hans R, Marwaha N (2014) Nucleic acid testing-benefits and constraints. Asian J Transfus Sci 8:2–3
Chang C, Ortiz K, Ansari A, Gershwin ME (2016) The Zika outbreak of the 21st century. J Autoimmun 68:1–13
Heymann DL, Liu J, Lillywhite L (2016) Partnerships, Not Parachutists, for Zika Research. N Engl J Med 374:1504–1505
Petersen LR, Jamieson DJ, Powers AM, Honein MA (2016) Zika virus. N Engl J Med 374:1552–1563
Yozwiak NL, Schaffner SF, Sabeti PC (2015) Data sharing: make outbreak research open access. Nature 518:477–479
Zika virus and potential complications. Geneva: World Health Organization, 2016 http://www.who.int/emergencies/zika-virus/en
Broutet N, Krauer F, Riesen M, Khalakdina A, Almiron M, Aldighieri S et al (2016) Zika virus as a cause of neurologic disorders. N Engl J Med 374:1506–1509
Malone RW, Homan J, Callahan MV, Glasspool-Malone J, Damodaran L et al (2016) Zika virus: medical countermeasure development challenges. PLoS Negl Trop Dis 10:e0004530
Derraik JG, Slaney D (2015) Notes on Zika virus—an emerging pathogen now present in the South Pacific. Aust N Z J Public Health 39:5–7
World Health Organization. Zika situation report 19 February 2016. http://apps.who.int/iris/bitstream/10665/204454/1/zikasitrep_19Feb2016_eng.pdf?ua=1.
McCarthy M (2016) Severe eye damage in infants with microcephaly is presumed to be due to Zika virus. BMJ 352:i855
de Fatima Vasco Aragao M, van der Linden V, Brainer-Lima AM, Coeli RR, Rocha MA, da Silva PS et al (2016) Clinical features and neuroimaging (CT and MRI) findings in presumed Zika virus related congenital infection and microcephaly: retrospective case series study. BMJ. doi:10.1136/bmj.i1901
Acknowledgments
We acknowledge Professor Brian Furman, University of Strathclyde, for his comments that greatly improved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maharajan, M., Ranjan, A., Chu, J. et al. Zika Virus Infection: Current Concerns and Perspectives. Clinic Rev Allerg Immunol 51, 383–394 (2016). https://doi.org/10.1007/s12016-016-8554-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-016-8554-7