Abstract
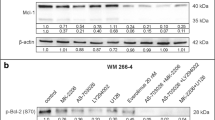
Itraconazole, an effective broad-spectrum antifungal drug, has been well established for its anticancer activity in cancers including melanoma. However, details concerning its underlying mechanism in melanoma are unclear. This work investigated the function of itraconazole-induced 5'-monophosphate (AMP)-activated protein kinase alpha (AMPKα) in melanoma progression through ERK signaling. The AMPKα level in melanoma tissues and cells was assessed by RT-qPCR and western blot. Survival analysis of patients with melanoma based on the AMPKα expression level was performed according to TCGA database. Melanoma cell proliferation, migration, and invasion were examined using CCK-8, colony formation, wound healing, and Transwell assays. A xenograft tumor model was established to examine the effect of itraconazole on tumor growth in vivo. The AMPKα mRNA and protein levels were reduced in melanoma tissues and cells. A low expression of AMPKα indicated a poor prognosis. Functionally, itraconazole restrained melanoma cell proliferation, migration, and invasion by upregulating AMPKα. Itraconazole activated AMPK signaling and inhibited ERK signaling in melanoma cells. Activation of ERK signaling reversed the effect of itraconazole on cellular process in melanoma. Moreover, itraconazole-induced AMPKα inhibited melanoma tumor growth in vivo by inhibiting ERK signaling. Itraconazole-induced AMPKα inhibits the progression of melanoma by inhibition of ERK signaling.





Similar content being viewed by others
Change history
10 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12013-023-01129-0
05 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12013-022-01103-2
References
Cui, S., Wang, J., Wu, Q., Qian, J., Yang, C., & Bo, P. (2017). Genistein inhibits the growth and regulates the migration and invasion abilities of melanoma cells via the FAK/paxillin and MAPK pathways. Oncotarget, 8(13), 21674–21691.
Sundstrøm, T., Espedal, H., Harter, P. N., Fasmer, K. E., Skaftnesmo, K. O., Horn, S., Hodneland, E., Mittelbronn, M., Weide, B., Beschorner, R., Bender, B., Rygh, C. B., Lund-Johansen, M., Bjerkvig, R., & Thorsen, F. (2015). Melanoma brain metastasis is independent of lactate dehydrogenase A expression. Neuro-oncology, 17(10), 1374–85.
Siegel, R. L., Miller, K. D., & Jemal, A. (2017). Cancer Statistics, 2017. CA: Cancer Journal for Clinicians, 67(1), 7–30.
Siegel, R. L., Miller, K. D., & Jemal, A. (2015). Cancer statistics, 2015. CA: Cancer Journal for Clinicians, 65(1), 5–29.
Bränström, R., Chang, Y. M., Kasparian, N., Affleck, P., Tibben, A., Aspinwall, L. G., Azizi, E., Baron-Epel, O., Battistuzzi, L., Bruno, W., Chan, M., Cuellar, F., Debniak, T., Pjanova, D., Ertmański, S., Figl, A., Gonzalez, M., Hayward, N. K., Hocevar, M., Kanetsky, P. A., Leaf, S. L., van Nieuwpoort, F. A., Heisele, O., Palmer, J., Peric, B., Puig, S., Ruffin, A. D., Schadendorf, D., Gruis, N. A., Brandberg, Y., & Newton-Bishop, J. (2010). Melanoma risk factors, perceived threat and intentional tanning: an international online survey. European Journal of Cancer Prevention, 19(3), 216–26.
Alexandrov, L. B., Nik-Zainal, S., Wedge, D. C., Aparicio, S. A., Behjati, S., Biankin, A. V., Bignell, G. R., Bolli, N., Borg, A., Børresen-Dale, A. L., Boyault, S., Burkhardt, B., Butler, A. P., Caldas, C., Davies, H. R., Desmedt, C., Eils, R., Eyfjörd, J. E., Foekens, J. A., Greaves, M., Hosoda, F., Hutter, B., Ilicic, T., Imbeaud, S., Imielinski, M., Jäger, N., Jones, D. T., Jones, D., Knappskog, S., Kool, M., Lakhani, S. R., López-Otín, C., Martin, S., Munshi, N. C., Nakamura, H., Northcott, P. A., Pajic, M., Papaemmanuil, E., Paradiso, A., Pearson, J. V., Puente, X. S., Raine, K., Ramakrishna, M., Richardson, A. L., Richter, J., Rosenstiel, P., Schlesner, M., Schumacher, T. N., Span, P. N., Teague, J. W., Totoki, Y., Tutt, A. N., Valdés-Mas, R., van Buuren, M. M., van ‘t Veer, L., Vincent-Salomon, A., Waddell, N., Yates, L. R., Zucman-Rossi, J., Futreal, P. A., McDermott, U., Lichter, P., Meyerson, M., Grimmond, S. M., Siebert, R., Campo, E., Shibata, T., Pfister, S. M., Campbell, P. J., & Stratton, M. R. (2013). Signatures of mutational processes in human cancer. Nature, 500(7463), 415–21.
Thompson, J. F., Scolyer, R. A., & Kefford, R. F. (2005). Cutaneous melanoma. Lancet, 365(9460), 687–701.
Hepner, A., Salgues, A., Anjos, C. A. D., Sahade, M., Camargo, V. P., Garicochea, B., Shoushtari, A. N., Postow, M. A., Fernandes, G. S., & Munhoz, R. R. (2017). Treatment of advanced melanoma—A changing landscape. Revista Associacao Medica Brasileira, 63(9), 814–823.
Shtivelman, E., Davies, M. Q., Hwu, P., Yang, J., Lotem, M., Oren, M., Flaherty, K. T., & Fisher, D. E. (2014). Pathways and therapeutic targets in melanoma. Oncotarget, 5(7), 1701–52.
Chien, A. J., Moore, E. C., Lonsdorf, A. S., Kulikauskas, R. M., Rothberg, B. G., Berger, A. J., Major, M. B., Hwang, S. T., Rimm, D. L., & Moon, R. T. (2009). Activated Wnt/beta-catenin signaling in melanoma is associated with decreased proliferation in patient tumors and a murine melanoma model. Proceedings of the National Academy of Sciences of the United States of America, 106(4), 1193–8.
Berghoff, A. S., & Preusser, M. (2018). New developments in brain metastases. Therapeutic Advances in Neurological Disorders, 11, 1756286418785502.
Hernandez, J. J., Pryszlak, M., Smith, L., Yanchus, C., Kurji, N., Shahani, V. M., & Molinski, S. V. (2017). Giving drugs a second chance: overcoming regulatory and financial hurdles in repurposing approved drugs as cancer therapeutics. Frontiers in Oncology, 7, 273.
Pandya, N. A., Atra, A. A., Riley, U., & Pinkerton, C. R. (2003). Role of itraconazole in haematology/oncology. Archives of Disease in Childhood, 88(3), 258–60.
Chong, C. R., Xu, J., Lu, J., Bhat, S., Sullivan, Jr, D. J., & Liu, J. O. (2007). Inhibition of angiogenesis by the antifungal drug itraconazole. ACS Chemical Biology, 2(4), 263–70.
Kim, J., Tang, J. Y., Gong, R., Kim, J., Lee, J. J., Clemons, K. V., Chong, C. R., Chang, K. S., Fereshteh, M., Gardner, D., Reya, T., Liu, J. O., Epstein, E. H., Stevens, D. A., & Beachy, P. A. (2010). Itraconazole, a commonly used antifungal that inhibits Hedgehog pathway activity and cancer growth. Cancer Cell, 17(4), 388–99.
Kim, J., Aftab, B. T., Tang, J. Y., Kim, D., Lee, A. H., Rezaee, M., Kim, J., Chen, B., King, E. M., Borodovsky, A., Riggins, G. J., Epstein, Jr, E. H., Beachy, P. A., & Rudin, C. M. (2013). Itraconazole and arsenic trioxide inhibit Hedgehog pathway activation and tumor growth associated with acquired resistance to smoothened antagonists. Cancer Cell, 23(1), 23–34.
Kim, D. J., Kim, J., Spaunhurst, K., Montoya, J., Khodosh, R., Chandra, K., Fu, T., Gilliam, A., Molgo, M., Beachy, P. A., & Tang, J. Y. (2014). Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. Journal of Clinical Oncology, 32(8), 745–51.
Rudin, C. M., Brahmer, J. R., Juergens, R. A., Hann, C. L., Ettinger, D. S., Sebree, R., Smith, R., Aftab, B. T., Huang, P., & Liu, J. O. (2013). Phase 2 study of pemetrexed and itraconazole as second-line therapy for metastatic nonsquamous non-small-cell lung cancer. Journal of Thoracic Oncology, 8(5), 619–23.
Tsubamoto, H., Sonoda, T., & Inoue, K. (2014). Impact of itraconazole on the survival of heavily pre-treated patients with triple-negative breast cancer. Anticancer Research, 34(7), 3839–44.
Inoue, K., Tsubamoto, H., Isono-Nakata, R., Sakata, K., & Nakagomi, N. (2018). Itraconazole treatment of primary malignant melanoma of the vagina evaluated using positron emission tomography and tissue cDNA microarray: a case report. BMC Cancer, 18(1), 630.
Shackelford, D. B., & Shaw, R. J. (2009). The LKB1-AMPK pathway: metabolism and growth control in tumour suppression. Nature Reviews Cancer, 9(8), 563–75.
Mihaylova, M. M., & Shaw, R. J. (2011). The AMPK signalling pathway coordinates cell growth, autophagy and metabolism. Nature Cell Biology, 13(9), 1016–23.
Faubert, B., Vincent, E. E., Poffenberger, M. C., & Jones, R. G. (2015). The AMP-activated protein kinase (AMPK) and cancer: many faces of a metabolic regulator. Cancer Letters, 356(2 Pt A), 165–70.
Guo, L., Bai, Y., Ji, S., & Ma, H. (2019). MicroRNA‑98 suppresses cell growth and invasion of retinoblastoma via targeting the IGF1R/k‑Ras/Raf/MEK/ERK signaling pathway. International Journal of Oncology, 54(3), 807–820.
Yu, Z., Ye, S., Hu, G., Lv, M., Tu, Z., Zhou, K., & Li, Q. (2015). The RAF-MEK-ERK pathway: targeting ERK to overcome obstacles to effective cancer therapy. Future Medicinal Chemistry, 7(3), 269–89.
Zhang, H., Jiang, H., Zhang, H., Liu, J., Hu, X., & Chen, L. (2019). Ribophorin II potentiates P-glycoprotein- and ABCG2-mediated multidrug resistance via activating ERK pathway in gastric cancer. International Journal of Biological Macromolecules, 128, 574–582.
Tandon, M., Chen, Z., Othman, A. H., & Pratap, J. (2016). Role of Runx2 in IGF-1Rβ/Akt- and AMPK/Erk-dependent growth, survival and sensitivity towards metformin in breast cancer bone metastasis. Oncogene, 35(36), 4730–40.
Head, S. A., Shi, W., Zhao, L., Gorshkov, K., Pasunooti, K., Chen, Y., Deng, Z., Li, R. J., Shim, J. S., Tan, W., Hartung, T., Zhang, J., Zhao, Y., Colombini, M., & Liu, J. O. (2015). Antifungal drug itraconazole targets VDAC1 to modulate the AMPK/mTOR signaling axis in endothelial cells. Proceedings of the National Academy of Sciences of the United States of America, 112(52), E7276–85.
Chen, M. B., Liu, Y. Y., Xing, Z. Y., Zhang, Z. Q., Jiang, Q., Lu, P. H., & Cao, C. (2018). Itraconazole-induced inhibition on human esophageal cancer cell growth requires AMPK activation. Molecular Cancer Therapeutics, 17(6), 1229–1239.
Liang, G., Liu, M., Wang, Q., Shen, Y., Mei, H., Li, D., & Liu, W. (2017). Itraconazole exerts its anti-melanoma effect by suppressing Hedgehog, Wnt, and PI3K/mTOR signaling pathways. Oncotarget, 8(17), 28510–28525.
Li, L., Zhao, D., Cheng, G., Li, Q., Chu, Y., Chu, H., Ding, Y., & Li, C. β-elemene suppresses Warburg effect in NCI-H1650 non-small-cell lung cancer cells by regulating the miR-301a-3p/AMPKà axis. Bioscience Reports, 40(6), BSR20194389.
Peng, Y. G., & Zhang, L. (2019). Wedelolactone suppresses cell proliferation and migration through AKT and AMPK signaling in melanoma. The Journal of Dermatological Treatment, 30(4), 389–395.
Chen, L., Chen, Q., Deng, G., Kuang, S., Lian, J., Wang, M., & Zhu, H. (2016). AMPK activation by GSK621 inhibits human melanoma cells in vitro and in vivo. Biochemical and Biophysical Research Communications, 480(4), 515–521.
Kfoury, A., Armaro, M., Collodet, C., Sordet-Dessimoz, J., Giner, M. P., Christen, S., Moco, S., Leleu, M., de Leval, L., Koch, U., Trumpp, A., Sakamoto, K., Beermann, F., & Radtke, F. (2018). AMPK promotes survival of c-Myc-positive melanoma cells by suppressing oxidative stress. Embo j, 37, 5.
Maehara, O., Suda, G., Natsuizaka, M., Ohnishi, S., Komatsu, Y., Sato, F., Nakai, M., Sho, T., Morikawa, K., Ogawa, K., Shimazaki, T., Kimura, M., Asano, A., Fujimoto, Y., Ohashi, S., Kagawa, S., Kinugasa, H., Naganuma, S., Whelan, K. A., Nakagawa, H., Nakagawa, K., Takeda, H., & Sakamoto, N. (2017). Fibroblast growth factor-2-mediated FGFR/Erk signaling supports maintenance of cancer stem-like cells in esophageal squamous cell carcinoma. Carcinogenesis., 38(11), 1073–1083.
Li, X., Dong, M., Zhou, J., Zhu, D., Zhao, J., & Sheng, W. (2019). C6orf106 accelerates pancreatic cancer cell invasion and proliferation via activating ERK signaling pathway. Molecular and Cellular Biochemistry, 454(1-2), 87–95.
Riverso, M., Montagnani, V., & Stecca, B. (2017). KLF4 is regulated by RAS/RAF/MEK/ERK signaling through E2F1 and promotes melanoma cell growth. Oncogene., 36(23), 3322–3333.
Ko, G. A., & Cho, S. K. (2018). Phytol suppresses melanogenesis through proteasomal degradation of MITF via the ROS-ERK signaling pathway. Chemico-Biological Interactions, 286, 132–140.
Acknowledgements
We thank all participators for their help.
Funding
The work was supported by Youth Science and technology project of Zhangjiagang (ZJGQNKJ202001) and Clinical medical science and technology development fund project of Jiangsu University (JLY20180173).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, N., Sun, Y., Yan, L. et al. Itraconazole-Induced the Activation of Adenosine 5'-Monophosphate (Amp)-Activated Protein Kinase Inhibits Tumor Growth of Melanoma via Inhibiting ERK Signaling. Cell Biochem Biophys 80, 331–340 (2022). https://doi.org/10.1007/s12013-021-01048-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-021-01048-y