Abstract
SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis) is a rare autoimmune disease which, due to its clinical presentation and symptoms, is often misdiagnosed and unrecognized. Its main features are prominent inflammatory cutaneous and articular manifestations. Treatments with immunosuppressive drugs have been used for the management of SAPHO with variable results. To date, the use of anti-TNF-α agents has proved to be an effective alternative to conventional treatment for unresponsive or refractory SAPHO cases. TNF-α is a pro-inflammatory cytokine and pivotal regulator of other cytokines, including IL-1 β, IL-6, and IL-8, involved in inflammation, acute-phase response induction, and chemotaxis. IL-1 inhibition strategies with anakinra have shown efficacy as first and second lines of treatment. In this review, we will describe the main characteristics of biological drugs currently used for SAPHO syndrome. We also describe some of the promising therapeutic effects of ustekinumab, an antibody against the p40 subunit of IL-12 and IL-23, after failure of multiple drugs including anti-TNF-α and anakinra. We discuss the use and impact of the new anti-IL-1 antagonists involved in the IL-17 blockade, in particular for the most difficult-to-treat SAPHO cases.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nguyen MT, Borchers A, Selmi C, Naguwa SM, Cheema G, Gershwin ME. The SAPHO syndrome. Semin Arthritis Rheum. 2012;42(3):254–65. doi:10.1016/j.semarthrit.2012.05.006.
McGonagle D, McDermott MF. A proposed classification of the immunological diseases. PLoS Med. 2006;3(8), e297. doi:10.1371/journal.pmed.0030297.
Braun-Falco M, Ruzicka T. Skin manifestations in autoinflammatory syndromes. J Dtsch Dermatol Ges. 2011;9(3):232–46. doi:10.1111/j.1610-0387.2010.07580.x.
Stern SM, Ferguson PJ. Autoinflammatory bone diseases. Rheum Dis Clin North Am. 2013;39(4):735–49. doi:10.1016/j.rdc.2013.05.002.
Wipff J, Adamsbaum C, Kahan A, Job-Deslandre C. Chronic recurrent multifocal osteomyelitis. Joint Bone Spine. 2011;78(6):555–60. doi:10.1016/j.jbspin.2011.02.010.
Beretta-Piccoli BC, Sauvain MJ, Gal I, Schibler A, Saurenmann T, Kressebuch H, et al. Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome in childhood: a report of ten cases and review of the literature. Eur J Pediatr. 2000;159(8):594–601.
Rohekar G, Inman RD. Conundrums in nosology: synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome and spondylarthritis. Arthritis Rheum. 2006;55(4):665–9. doi:10.1002/art.22087.
Aljuhani F, Tournadre A, Tatar Z, Couderc M, Mathieu S, Malochet-Guinamand S, et al. The SAPHO syndrome: a single-center study of 41 adult patients. J Rheumatol. 2015;42(2):329–34. doi:10.3899/jrheum.140342. A recent case-series of patients with SAPHO syndrome providing clinical and therapeutic insights.
Hayem G, Bouchaud-Chabot A, Benali K, Roux S, Palazzo E, Silbermann-Hoffman O, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum. 1999;29(3):159–71.
Colina M, Govoni M, Orzincolo C, Trotta F. Clinical and radiologic evolution of synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: a single center study of a cohort of 71 subjects. Arthritis Rheum. 2009;61(6):813–21. doi:10.1002/art.24540.
Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol. 1988;6(2):109–12.
Chamot AM, Benhamou CL, Kahn MF, Beraneck L, Kaplan G, Prost A. Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic. 1987;54(3):187–96.
Ombrello MJ. Advances in the genetically complex autoinflammatory diseases. Semin Immunopathol. 2015;37(4):403–6. doi:10.1007/s00281-015-0498-0. Updated view on the current classification of autoinflammatory diseases, their genetic basis and relevant undisclosed issues.
Almeida de Jesus A, Goldbach-Mansky R. Monogenic autoinflammatory diseases: concept and clinical manifestations. Clin Immunol. 2013;147(3):155–74. doi:10.1016/j.clim.2013.03.016.
Ferguson PJ, Bing X, Vasef MA, Ochoa LA, Mahgoub A, Waldschmidt TJ, et al. A missense mutation in pstpip2 is associated with the murine autoinflammatory disorder chronic multifocal osteomyelitis. Bone. 2006;38(1):41–7. doi:10.1016/j.bone.2005.07.009.
Cassel SL, Janczy JR, Bing X, Wilson SP, Olivier AK, Otero JE, et al. Inflammasome-independent IL-1beta mediates autoinflammatory disease in Pstpip2-deficient mice. Proc Natl Acad Sci U S A. 2014;111(3):1072–7. doi:10.1073/pnas.1318685111. This paper shows the role of cytokine IL-1β in the Pstpip2-deficient mice affected by chronic multifocal osteomyelitis.
Hurtado-Nedelec M, Chollet-Martin S, Chapeton D, Hugot JP, Hayem G, Gerard B. Genetic susceptibility factors in a cohort of 38 patients with SAPHO syndrome: a study of PSTPIP2, NOD2, and LPIN2 genes. J Rheumatol. 2010;37(2):401–9. doi:10.3899/jrheum.090456.
Colina M, Pippucci T, Moro MA, Marconi C, Magini P, Ciancio G, et al. Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome: is PTPN22 involved? Clin Exp Rheumatol. 2012;30(3):451.
Koenders MI, Devesa I, Marijnissen RJ, Abdollahi-Roodsaz S, Boots AM, Walgreen B, et al. Interleukin-1 drives pathogenic Th17 cells during spontaneous arthritis in interleukin-1 receptor antagonist-deficient mice. Arthritis Rheum. 2008;58(11):3461–70. doi:10.1002/art.23957.
Shepherd J, Little MC, Nicklin MJ. Psoriasis-like cutaneous inflammation in mice lacking interleukin-1 receptor antagonist. J Invest Dermatol. 2004;122(3):665–9. doi:10.1111/j.0022-202X.2004.22305.x.
Aksentijevich I, Masters SL, Ferguson PJ, Dancey P, Frenkel J, van Royen-Kerkhoff A, et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med. 2009;360(23):2426–37. doi:10.1056/NEJMoa0807865.
Firinu D, Barca MP, Lorrai MM, Perra S, Cabras S, Muggianu E, et al. TH17 cells are increased in the peripheral blood of patients with SAPHO syndrome. Autoimmunity. 2014;47(6):389–94. doi:10.3109/08916934.2014.906582.
Hofmann SR, Morbach H, Schwarz T, Rosen-Wolff A, Girschick HJ, Hedrich CM. Attenuated TLR4/MAPK signaling in monocytes from patients with CRMO results in impaired IL-10 expression. Clin Immunol. 2012;145(1):69–76. doi:10.1016/j.clim.2012.07.012.
Hurtado-Nedelec M, Chollet-Martin S, Nicaise-Roland P, Grootenboer-Mignot S, Ruimy R, Meyer O, et al. Characterization of the immune response in the synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome. Rheumatology (Oxford). 2008;47(8):1160–7. doi:10.1093/rheumatology/ken185.
Lasiglie D, Traggiai E, Federici S, Alessio M, Buoncompagni A, Accogli A, et al. Role of IL-1 beta in the development of human T(H)17 cells: lesson from NLPR3 mutated patients. PLoS One. 2011;6(5), e20014. doi:10.1371/journal.pone.0020014.
Ovadia A, Livneh A, Feld O, Ben-Zvi I, Kukuy E, Kivity S, et al. T helper 17 polarization in familial Mediterranean fever. Genes Immun. 2013;14(4):212–6. doi:10.1038/gene.2013.6.
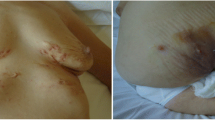
Zuo RC, Schwartz DM, Lee CC, Anadkat MJ, Cowen EW, Naik HB. Palmoplantar pustules and osteoarticular pain in a 42-year-old woman. J Am Acad Dermatol. 2015;72(3):550–3. doi:10.1016/j.jaad.2014.07.014.
Wallach D, Vignon-Pennamen MD. From acute febrile neutrophilic dermatosis to neutrophilic disease: forty years of clinical research. J Am Acad Dermatol. 2006;55(6):1066–71. doi:10.1016/j.jaad.2006.07.016.
Marzano AV, Ishak RS, Saibeni S, Crosti C, Meroni PL, Cugno M. Autoinflammatory skin disorders in inflammatory bowel diseases, pyoderma gangrenosum and Sweet’s syndrome: a comprehensive review and disease classification criteria. Clin Rev Allergy Immunol. 2013;45(2):202–10. doi:10.1007/s12016-012-8351-x.
Borella E, Palma L, Zen M, Bettio S, Nalotto L, Gatto M, et al. The body against self: autoinflammation and autoimmunity. Isr Med Assoc J. 2014;16(10):608–10.
Marzano AV, Cugno M, Trevisan V, Lazzari R, Fanoni D, Berti E, et al. Inflammatory cells, cytokines and matrix metalloproteinases in amicrobial pustulosis of the folds and other neutrophilic dermatoses. Int J Immunopathol Pharmacol. 2011;24(2):451–60.
Scarpa R, Lubrano E, Cozzi R, Ames PR, Oriente CB, Oriente P. Subcorneal pustular dermatosis (Sneddon-Wilkinson syndrome): another cutaneous manifestation of SAPHO syndrome? Br J Rheumatol. 1997;36(5):602–3.
Marzano AV, Cugno M, Trevisan V, Fanoni D, Venegoni L, Berti E, et al. Role of inflammatory cells, cytokines and matrix metalloproteinases in neutrophil-mediated skin diseases. Clin Exp Immunol. 2010;162(1):100–7. doi:10.1111/j.1365-2249.2010.04201.x.
Pene J, Chevalier S, Preisser L, Venereau E, Guilleux MH, Ghannam S, et al. Chronically inflamed human tissues are infiltrated by highly differentiated Th17 lymphocytes. J Immunol. 2008;180(11):7423–30.
Marzano AV, Tavecchio S, Berti E, Gelmetti C, Cugno M. Paradoxical autoinflammatory skin reaction to tumor necrosis factor alpha blockers manifesting as amicrobial pustulosis of the folds in patients with inflammatory bowel diseases. Medicine (Baltimore). 2015;94(45), e1818. doi:10.1097/MD.0000000000001818.
Ruddy MJ, Wong GC, Liu XK, Yamamoto H, Kasayama S, Kirkwood KL, et al. Functional cooperation between interleukin-17 and tumor necrosis factor-alpha is mediated by CCAAT/enhancer-binding protein family members. J Biol Chem. 2004;279(4):2559–67. doi:10.1074/jbc.M308809200.
Skov L, Beurskens FJ, Zachariae CO, Reitamo S, Teeling J, Satijn D, et al. IL-8 as antibody therapeutic target in inflammatory diseases: reduction of clinical activity in palmoplantar pustulosis. J Immunol. 2008;181(1):669–79.
Pelletier M, Maggi L, Micheletti A, Lazzeri E, Tamassia N, Costantini C, et al. Evidence for a cross-talk between human neutrophils and Th17 cells. Blood. 2010;115(2):335–43. doi:10.1182/blood-2009-04-216085.
Kalke S, Perera SD, Patel ND, Gordon TE, Dasgupta B. The sternoclavicular syndrome: experience from a district general hospital and results of a national postal survey. Rheumatology (Oxford). 2001;40(2):170–7.
Depasquale R, Kumar N, Lalam RK, Tins BJ, Tyrrell PN, Singh J, et al. SAPHO: what radiologists should know. Clin Radiol. 2012;67(3):195–206. doi:10.1016/j.crad.2011.08.014.
Fu Z, Liu M, Li Z, Fan Y, Zhang J, Zhang X, et al. Is the bullhead sign on bone scintigraphy really common in the patient with SAPHO syndrome? A single-center study of a 16-year experience. Nucl Med Commun. 2015. doi:10.1097/MNM.0000000000000451.
Jung J, Molinger M, Kohn D, Schreiber M, Pfreundschuh M, Assmann G. Intra-articular glucocorticosteroid injection into sternocostoclavicular joints in patients with SAPHO syndrome. Semin Arthritis Rheum. 2012;42(3):266–70. doi:10.1016/j.semarthrit.2012.03.012.
Assmann G, Kueck O, Kirchhoff T, Rosenthal H, Voswinkel J, Pfreundschuh M, et al. Efficacy of antibiotic therapy for SAPHO syndrome is lost after its discontinuation: an interventional study. Arthritis Res Ther. 2009;11(5):R140. doi:10.1186/ar2812.
Murakami M, Masuda K, Utsunomiya R, Oda F, Namba C, Sayama K. Cefcapene pivoxil hydrochloride is a potentially new treatment for palmoplantar pustulosis with pustulotic arthro-osteitis. Dermatology. 2015;231(4):304–11. doi:10.1159/000439401.
Yabe H, Ohshima H, Takano Y, Koyanagi T, Usui H, Nojiri K, et al. Mucosal lesions may be a minor complication of SAPHO syndrome: a study of 11 Japanese patients with SAPHO syndrome. Rheumatol Int. 2010;30(10):1277–83. doi:10.1007/s00296-009-1138-6.
Yamamoto T. Pustulotic arthro-osteitis associated with palmoplantar pustulosis. J Dermatol. 2013;40(11):857–63. doi:10.1111/1346-8138.12272.
Amital H, Applbaum YH, Aamar S, Daniel N, Rubinow A. SAPHO syndrome treated with pamidronate: an open-label study of 10 patients. Rheumatology (Oxford). 2004;43(5):658–61. doi:10.1093/rheumatology/keh149.
Solau-Gervais E, Soubrier M, Gerot I, Grange L, Puechal X, Sordet C, et al. The usefulness of bone remodelling markers in predicting the efficacy of pamidronate treatment in SAPHO syndrome. Rheumatology (Oxford). 2006;45(3):339–42. doi:10.1093/rheumatology/kei160.
Colina M, La Corte R, Trotta F. Sustained remission of SAPHO syndrome with pamidronate: a follow-up of fourteen cases and a review of the literature. Clin Exp Rheumatol. 2009;27(1):112–5.
Delattre E, Guillot X, Godfrin-Valnet M, Prati C, Wendling D. SAPHO syndrome treatment with intravenous pamidronate. Retrospective study of 22 patients. Joint Bone Spine. 2014. doi:10.1016/j.jbspin.2014.01.017.
Hayama K, Inadomi T, Fujisawa D, Terui T. A pilot study of medium-dose cyclosporine for the treatment of palmoplantar pustulosis complicated with pustulotic arthro-osteitis. Eur J Dermatol. 2010;20(6):758–62. doi:10.1684/ejd.2010.1109.
Kundu BK, Naik AK, Bhargava S, Srivastava D. Diagnosing the SAPHO syndrome: a report of three cases and review of literature. Clin Rheumatol. 2013;32(8):1237–43. doi:10.1007/s10067-013-2251-1.
Gorecki P, Stockmann P, Distler JHW, Wuest W, Schmidt D, Neukam FW, et al. Implication of bisphosphonate use in the treatment of SAPHO syndrome: case report and discussion of current literature. J Med Hypotheses Ideas. 2015;9(2):72–8. doi:10.1016/j.jmhi.2015.04.002.
Olivieri I, Padula A, Ciancio G, Salvarani C, Niccoli L, Cantini F. Successful treatment of SAPHO syndrome with infliximab: report of two cases. Ann Rheum Dis. 2002;61(4):375–6.
Wagner AD, Andresen J, Jendro MC, Hulsemann JL, Zeidler H. Sustained response to tumor necrosis factor alpha-blocking agents in two patients with SAPHO syndrome. Arthritis Rheum. 2002;46(7):1965–8. doi:10.1002/art.10539.
Burgemeister LT, Baeten DL, Tas SW. Biologics for rare inflammatory diseases: TNF blockade in the SAPHO syndrome. Neth J Med. 2012;70(10):444–9.
Hayem G, M’Barek RB, Toussirot E, Compaore C, Pham T, Houvenagel E et al. Abstracts of the American College of Rheumatology & Association of Rheumatology Health Professionals, Annual Scientific Meeting. November 6–11, 2010. Atlanta, Georgia, USA. Arthritis Rheum. 2010;62 Suppl 10:1. doi:10.1002/art.30032.
Laveti D, Kumar M, Hemalatha R, Sistla R, Naidu VG, Talla V, et al. Anti-inflammatory treatments for chronic diseases: a review. Inflamm Allergy Drug Targets. 2013;12(5):349–61.
Robinson A, Van Voorhees AS, Hsu S, Korman NJ, Lebwohl MG, Bebo Jr BF, et al. Treatment of pustular psoriasis: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2012;67(2):279–88. doi:10.1016/j.jaad.2011.01.032.
Haslund P, Lee RA, Jemec GB. Treatment of hidradenitis suppurativa with tumour necrosis factor-alpha inhibitors. Acta Derm Venereol. 2009;89(6):595–600. doi:10.2340/00015555-0747.
Adisen E, Gurer MA. Therapeutic options for palmoplantar pustulosis. Clin Exp Dermatol. 2010;35(3):219–22. doi:10.1111/j.1365-2230.2009.03520.x.
Delage M, Samimi M, Atlan M, Machet L, Lorette G, Maruani A. Efficacy of infliximab for hidradenitis suppurativa: assessment of clinical and biological inflammatory markers. Acta Derm Venereol. 2011;91(2):169–71. doi:10.2340/00015555-1025.
Vilar-Alejo J, Dehesa L, de la Rosa-del Rey P, Novoa-Medina J, Valeron Almazan P, Santana Medina N, et al. SAPHO syndrome with unusual cutaneous manifestations treated successfully with etanercept. Acta Derm Venereol. 2010;90(5):531–2. doi:10.2340/00015555-0895.
Moll C, Hernandez MV, Canete JD, Gomez-Puerta JA, Soriano A, Collado A, et al. Ilium osteitis as the main manifestation of the SAPHO syndrome: response to infliximab therapy and review of the literature. Semin Arthritis Rheum. 2008;37(5):299–306. doi:10.1016/j.semarthrit.2007.08.004.
Massara A, Cavazzini PL, Trotta F. In SAPHO syndrome anti-TNF-alpha therapy may induce persistent amelioration of osteoarticular complaints, but may exacerbate cutaneous manifestations. Rheumatology (Oxford). 2006;45(6):730–3. doi:10.1093/rheumatology/kei221.
De Souza A, Solomon GE, Strober BE. SAPHO syndrome associated with hidradenitis suppurativa successfully treated with infliximab and methotrexate. Bull NYU Hosp Jt Dis. 2011;69(2):185–7.
Salles M, Olive A, Perez-Andres R, Holgado S, Mateo L, Riera E, et al. The SAPHO syndrome: a clinical and imaging study. Clin Rheumatol. 2011;30(2):245–9. doi:10.1007/s10067-010-1560-x.
Fruehauf J, Cierny-Modre B, Caelen Lel S, Schwarz T, Weinke R, Aberer E. Response to infliximab in SAPHO syndrome. BMJ Case Rep. 2009;2009. doi: 10.1136/bcr.10.2008.1145.
Ben Abdelghani K, Dran DG, Gottenberg JE, Morel J, Sibilia J, Combe B. Tumor necrosis factor-alpha blockers in SAPHO syndrome. J Rheumatol. 2010;37(8):1699–704. doi:10.3899/jrheum.091086.
Firinu D, Murgia G, Lorrai MM, Barca MP, Peralta MM, Manconi PE, et al. Biological treatments for SAPHO syndrome: an update. Inflamm Allergy Drug Targets. 2014;13(3):199–205.
Zhang LL, Zhao JX, Liu XY. Successful treatment of SAPHO syndrome with severe spinal disorder using entercept: a case study. Rheumatol Int. 2012;32(7):1963–5. doi:10.1007/s00296-011-1916-9.
Arias-Santiago S, Sanchez-Cano D, Callejas-Rubio JL, Fernandez-Pugnaire MA, Ortego-Centeno N. Adalimumab treatment for SAPHO syndrome. Acta Derm Venereol. 2010;90(3):301–2. doi:10.2340/00015555-0822.
Garcovich S, Amelia R, Magarelli N, Valenza V, Amerio P. Long-term treatment of severe SAPHO syndrome with adalimumab: case report and a review of the literature. Am J Clin Dermatol. 2012;13(1):55–9. doi:10.2165/11593250-000000000-00000.
Henriques CC, Sousa M, Panarra A, Riso N. The dark side of SAPHO syndrome. BMJ Case Rep. 2011. doi:10.1136/bcr.11.2011.5197.
Brunasso AM, Laimer M, Massone C. Paradoxical reactions to targeted biological treatments: a way to treat and trigger? Acta Derm Venereol. 2010;90(2):183–5. doi:10.2340/00015555-0777.
Kamata Y, Minota S. Successful treatment of a patient with SAPHO syndrome with certolizumab pegol. Rheumatol Int. 2015;35(9):1607–8. doi:10.1007/s00296-015-3263-8.
Chimenti MS, Teoli M, Saraceno R, Dattola A, Ventura A, Chiricozzi A, et al. Golimumab in patients affected by moderate to severe psoriatic arthritis: an open-label study in thirty-two patients previously treated with other biologics. Dermatology. 2013;227(4):305–10. doi:10.1159/000354263.
Firinu D, Lorrai MM, Barca MP, Peralta MM, Mura MN, Perra S, et al. Increased peripheral T(H)17 Cells in SAPHO syndrome: a novel target for treatment? Allergy. 2013;68:198–9.
Colina M, Pizzirani C, Khodeir M, Falzoni S, Bruschi M, Trotta F, et al. Dysregulation of P2X7 receptor-inflammasome axis in SAPHO syndrome: successful treatment with anakinra. Rheumatology (Oxford). 2010;49(7):1416–8. doi:10.1093/rheumatology/keq074.
Wendling D, Prati C, Aubin F. Anakinra treatment of SAPHO syndrome: short-term results of an open study. Ann Rheum Dis. 2012;71(6):1098–100. doi:10.1136/annrheumdis-2011-200743. The largest published series of SAPHO patients treated with Anakinra.
Fujita S, Kosaka N, Mito T, Hayashi H, Morita Y. Development of aseptic subcutaneous abscess after tocilizumab therapy in a patient with SAPHO syndrome complicated by amyloid A amyloidosis. Int J Rheum Dis. 2015;18(4):476–9. doi:10.1111/1756-185X.12525.
Gerdes S, Franke J, Domm S, Mrowietz U. Ustekinumab in the treatment of palmoplantar pustulosis. Br J Dermatol. 2010;163(5):1116–8. doi:10.1111/j.1365-2133.2010.09897.x.
Edlund E, Johnsson U, Lidgren L, Pettersson H, Sturfelt G, Svensson B, et al. Palmoplantar pustulosis and sternocostoclavicular arthro-osteitis. Ann Rheum Dis. 1988;47(10):809–15.
Jappe U, Boit R, Farrar MD, Ingham E, Sandoe J, Holland KT. Evidence for diversity within Propionibacterium acnes: a comparison of the T-cell stimulatory activity of isolates from inflammatory acne, endocarditis and the laboratory. J Eur Acad Dermatol Venereol. 2004;18(4):450–4. doi:10.1111/j.1468-3083.2004.00950.x.
Hayem G, Hurtado-Nedelec M, Chollet-Martin S. The immune response in SAPHO syndrome: deficiency, hyper- responsiveness, or both? Curr Rheumatol Rev. 2013;9(1):11–4.
Benucci M, Saviola G, Baiardi P, Manfredi M, Sarzi-Puttini P, Atzeni F. Efficacy and safety of leflunomide or methotrexate plus subcutaneous tumour necrosis factor-alpha blocking agents in rheumatoid arthritis. Int J Immunopathol Pharmacol. 2011;24(1):269–74.
Garces S, Demengeot J, Benito-Garcia E. The immunogenicity of anti-TNF therapy in immune-mediated inflammatory diseases: a systematic review of the literature with a meta-analysis. Ann Rheum Dis. 2013;72(12):1947–55. doi:10.1136/annrheumdis-2012-202220.
Meyer MW, Zachariae C, Bendtzen K, Skov L. Lack of anti-drug antibodies in patients with psoriasis well-controlled on long-term treatment with tumour necrosis factor inhibitors. Acta Derm Venereol. 2012;92(4):362–4. doi:10.2340/00015555-1376.
Dinarello CA, Simon A, van der Meer JW. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov. 2012;11(8):633–52. doi:10.1038/nrd3800.
Sanna M, Firinu D, Manconi PE, Pisanu M, Murgia G, Piras V, et al. The salivary proteome profile in patients affected by SAPHO syndrome characterized by a top-down RP-HPLC-ESI-MS platform. Mol Biosyst. 2015. doi:10.1039/c4mb00719k.
Colina M, Trotta F. Clinical and radiological characteristics of SAPHO syndrome. Curr Rheumatol Rev. 2013;9(1):22–7. A paper describing the key aspects of the disease.
Marotte H, Cimaz R. Etanercept—TNF receptor and IgG1 Fc fusion protein: is it different from other TNF blockers? Expert Opin Biol Ther. 2014. doi:10.1517/14712598.2014.896334.
Eleftheriou D, Gerschman T, Sebire N, Woo P, Pilkington CA, Brogan PA. Biologic therapy in refractory chronic non-bacterial osteomyelitis of childhood. Rheumatology (Oxford). 2010;49(8):1505–12. doi:10.1093/rheumatology/keq122.
Lukens JR, Gross JM, Calabrese C, Iwakura Y, Lamkanfi M, Vogel P, et al. Critical role for inflammasome-independent IL-1beta production in osteomyelitis. Proc Natl Acad Sci U S A. 2014;111(3):1066–71. doi:10.1073/pnas.1318688111. This paper shows the role of IL-1β dysregulation and identifies PSTPIP2 as a negative regulator of caspase-1–autonomous IL-1β production in chronic multifocal osteomyelitis of mice.
Pham TN, Rahman P, Richardson VJ. Divergent effects of infliximab and anakinra therapies on macrophage phenotype from patients with refractory rheumatoid arthritis. Int J Immunopathol Pharmacol. 2010;23(2):491–501.
Castrichini M, Lazzerini PE, Gamberucci A, Capecchi PL, Franceschini R, Natale M, et al. The purinergic P2x7 receptor is expressed on monocytes in Behcet’s disease and is modulated by TNF-alpha. Eur J Immunol. 2013. doi:10.1002/eji.201343353.
Scholtysek C, Kronke G, Schett G. Inflammation-associated changes in bone homeostasis. Inflamm Allergy Drug Targets. 2012;11(3):188–95.
Abu-Amer Y, Darwech I, Otero J. Role of the NF-kappaB axis in immune modulation of osteoclasts and bone loss. Autoimmunity. 2008;41(3):204–11. doi:10.1080/08916930701694543.
Sharon VR, Garcia MS, Bagheri S, Goodarzi H, Yang C, Ono Y, et al. Management of recalcitrant hidradenitis suppurativa with ustekinumab. Acta Derm Venereol. 2012;92(3):320–1. doi:10.2340/00015555-1229.
Hermanns-Le T, Berardesca E, Pierard GE, Lesuisse M, Pierard-Franchimont C. Challenging regional psoriasis and ustekinumab biotherapy: impact of the patterns of disease. J Biomed Biotechnol. 2012;2012:413767. doi:10.1155/2012/413767.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with the Helsinki declaration and its amendments and institutional research committee standards.
Additional information
Topical Collection on Orphan Diseases
Rights and permissions
About this article
Cite this article
Firinu, D., Garcia-Larsen, V., Manconi, P.E. et al. SAPHO Syndrome: Current Developments and Approaches to Clinical Treatment. Curr Rheumatol Rep 18, 35 (2016). https://doi.org/10.1007/s11926-016-0583-y
Published:
DOI: https://doi.org/10.1007/s11926-016-0583-y