Abstract
Attention deficit hyperactivity disorder (ADHD) affects approximately 5 % of children and adolescents, and sleep problems are common in these patients. There is growing evidence informing the significant importance of sleep problems in youth with ADHD. The sleep problems in children with ADHD include specific sleep disorders and sleep disturbances due to comorbid psychiatric disorders or ADHD medications. The specific sleep disorders of ADHD children include behaviorally based insomnia, sleep-disordered breathing, and restless legs syndrome/periodic limb movement disorder. Current practices on the management of sleep problems for ADHD children are based mostly on expert consensus, whereas more evidence-based literature can be found only recently. Assessment of the sleep conditions in ADHD children before initiation of pharmacotherapy is the currently recommended guideline, and good sleep hygiene can be considered as the first-line treatment option. In addition to modifying the dose regimens, formulation, or alternative stimulants when sleep problems are encountered in ADHD children, atomoxetine, once daily guanfacine extended release, and melatonin are potential choices for ADHD children with more severe sleep problems. In this review, we aimed to provide the most updated information, preferably based on meta-analyses, systemic review, and randomized controlled trials published in the latest 3 years, in order to be clinically useful for practitioners and clinicians.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance, •• Of major importance
Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. 2008;162:336–42.
Um YH, Jeong JH, Hong SC, Kim TW, Lim HK, Seo HJ, et al. Association between sleep parameters and cognitive function in drug-naïve children with attention-deficit hyperactivity disorder: a polysomnographic study. Sleep Med. doi:10.1016/j.sleep.2015.11.016. This study documented the relationship between sleep parameters and cognitive function in drug-naïve children with ADHD, while most subjects in previous studies were on medication, which is a potent confounding factor.
Mulraney M, Giallo R, Lycett K, Mensah F, Sciberras E. The bidirectional relationship between sleep problems and internalizing and externalizing problems in children with ADHD: a prospective cohort study. Sleep Med. 2016;17:45–51.
Katzman MA, Sternat T. A review of OROS methylphenidate (Concerta®) in the treatment of attention-deficit/hyperactivity disorder. CNS Drugs. 2014;28:1005–33.
Becker SP, Pfiffner LJ, Stein MA, Burns GL, McBurnett K. Sleep habits in children with attention-deficit/hyperactivity disorder predominantly inattentive type and associations with comorbid psychopathology symptoms. Sleep Med. 2015;11:S1389–9457.
Canals J, Morales-Hidalgo P, Jané MC, Domènech E. ADHD prevalence in Spanish preschoolers: comorbidity, socio-demographic factors, and functional consequences. J Atten Disord. 2016. doi:10.1177/1087054716638511.
Yallop L, Brownell M, Chateau D, Walker J, Warren M, Baillis D, et al. Lifetime prevalence of attention-deficit/hyperactivity disorder in young adults: examining variations in the socioeconomic gradient. Can J Psychiatry. 2015;60:432–40.
Wang KY. Updated findings on neurodevelopmental disorders in Taiwan: impact of the institutionalized national healthcare system on prevalence and health outcomes. Curr Opin Psychiatry. 2016;29:144–8.
Aquirre Castaneda RL, Kumar S, Voigt RG, Leibson CL, Barbaresi WJ, et al. Childhood attention-deficit/hyperactivity disorder, sex, and obesity: a longitudinal population-based study. Mayo Clin Proc. 2016;91:352–61.
van Lieshout M, Luman M, Twisk JW, van Ewijk H, Groenman AP, Thissen AJ, et al. A 6-year follow-up of a large European cohort of children with attention-deficity/hyperactivity disorder-combined subtype: outcomes in late adolescence and young adulthood. Eur Child Adolesc Psychiatry. 2016. doi:10.1007/s00787-016-0820-y.
Casas M, Rösler M, Sandra Kooij JJ, Ginsberg Y, Ramos-Quiroga JA, Heger S, et al. Efficacy and safety of prolonged-release OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a 13-week, randomized, double-blind, placebo-controlled, fixed-dose study. World J Biol Psychiatry. 2013;14:268–81.
Rönnlund H, Elovainio M, Virtanen I, Matomäki J, Lapinleimu H. Poor parental sleep and the reported sleep quality of their children. Pediatrics. 2016. doi:10.1542/peds.2015-3425.
Kronholm E, Puusniekka R, Jokela J, Villberg J, Urrila AS, Paunio T, et al. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res. 2015;24:3–10.
Hysing M, Pallesen S, Stormark KM, Lundervold AJ, Sivertsen B. Sleep patterns and insomnia among adolescents: a population-based study. J Sleep Res. 2013;22:549–56.
Efron D, Lycett K, Sciberras E. Use of sleep medication in children with ADHD. Sleep Med. 2014;15:472–5.
Corkum P, Davidson F, MacPherson M. A framework for the assessment and treatment of sleep problems in children with attention-deficit/hyperactivity disorder. Pediatr Clin N Am. 2011;58:667–83.
Cortese S, Lecendreux M, Mouren MC, Konofal E. ADHD and insomnia. J Am Acad Child Adolesc Psychiatry. 2006;45:384–5.
Mitchison GM, Njardvik U. Prevalence and gender differences of ODD, anxiety, and depression in a sample of children with ADHD. J Atten Disord. 2015. doi:10.1177/1087054715608442.
Lee MJ, Yang KC, Shyu YC, Yuan SS, Yang CJ, Lee SY, et al. Attention-deficit hyperactivity disorder, its treatment with medication and the probability of developing a depressive disorder: a nationwide population-based study in Taiwan. J Affect Disord. 2016;189:110–7.
Spruyt K, Gozal D. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Expert Rev Neurother. 2011;11:565–77.
Sciberras E, Lycett K, Efron D, Mensah F, Gerner B, Hiscock H. Anxiety in children with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133:801–8.
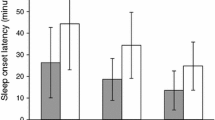
Kidwell KM, Van Dyk TR, Lundahl A, Nelson TD. Stimulant medications and sleep for youth with ADHD: a meta-analysis. Pediatrics. 2015;136:1144–53. This is a recent published meta-analysis of stimulant medication regarding its effects of longer sleep latency, worse sleep efficiency, and shorter sleep duration.
Santisteban JA, Stein MA, Bergmame L, Gruber R. Effect of extended-release dexmethylphenidate and mixed amphetamine salts on sleep: a double-blind, randomized, crossover study in youth with attention-deficit hyperactivity disorder. CNS Drugs. 2014;28:825–33.
LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–65.
Meltzer LJ, Brimeyer C, Russell K, Avis KT, Biggs S, Reynolds AC, et al. The children’s report of sleep patterns: validity and reliability of the sleep hygiene index and sleep disturbance scale in adolescents. Sleep Med. 2014;15:1500–7.
Weiss MD, Salpekar J. Sleep problems in the child with attention-deficit/hyperactivity disorder: defining etiology and appropriate treatments. CNS Drugs. 2010;24:811–28.
Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: a pilot randomized controlled trial. Sleep Med. 2011;12:932–5.
Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D, Khano S, et al. Impact of a behavioral sleep intervention on symptoms and sleep in children with attention-deficit/hyperactivity disorder, and parental mental health: randomized controlled trial. BMJ. 2015;350:h68. This study providing evidence-based information using RCT documenting the effect of behavior sleep intervention on ADHD children with sleep problems.
Vidal R, Castells J, Richarte V, Palomar G, Garcia M, Nicolau R, et al. Group therapy for adolescents with attention-deficit/hyperactivity disorder: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:275–82. This study is the latest and an important RCT documenting the effect of group therapy for adolescents with ADHD.
Santisteban JA, Stein MA, Bergmame L, Gruber R. Effect of extended-release dexmethylphenidate and mixed amphetamine salts on sleep: a double-blind, randomized, crossover study in youth with attention-deficit hyperactivity disorder. CNS Drugs. 2014;28:825–33. This study highlights that higher stimulant doses are associated with reduced sleep duration and later sleep start times, regardless of medication class.
Bock DE, Roach-Fox E, Seabrook JA, Rieder MJ, Matsui D. Sleep-promoting medications in children: physician prescribing habits in Southwestern Ontario. Canada Sleep Med. 2016;17:52–6.
Golmirzaei J, Mahboobi H, Yazdanparast M, Mushtag G, Kamal MA, Hamzei E. Psychopharmacology of attention-deficit hyperactivity disorder: effects and side effects. Curr Pharm Des. 2016;22:590–4.
Furster C, Hallerbäck MU. The use of melatonin in Swedish children and adolescents—a register-based study according to age, gender, and medication of ADHD. Eur J Clin Pharmacol. 2015;71:877–81.
Dalsgaard S, Nielsen HS, Simonsen M. Five-fold increase in national prevalence rates of attention-deficit/hyperactivity disorder medications for children and adolescents with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other psychiatric disorders: a Danish register-based study. J Child Adolesc Psychopharmacol. 2013;23:432–9.
van der Heijden KB, Smits MG, Van Someren EJ, Gunning WB. Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiol Int. 2005;22:559–70.
van Geijlswijk IM, Korzilius HP, Smits MG. The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep. 2010;33:1605–14.
Bendz LM, Scates AC. Melatonin treatment for insomnia in pediatric patients with attention-deficit/hyperactivity disorder. Ann Pharmacother. 2010;44:185–91.
Gringras P, Gamble C, Jones AP, Wiggs L, Williamson PR, Sutcliffe A, et al. Melatonin for sleep problems in children with neurodevelopmental disorders: randomized double masked placebo controlled trial. BMJ. 2012;345:e6664.
Hoebert M, van der Heijden KB, van Geijlswijk IM, Smits MG. Long-term follow-up of melatonin treatment in children with ADHD and chronic sleep onset insomnia. J Pineal Res. 2009;47:1–7.
Sallee F, Connor DF, Newcorn JH. A review of the rationale and clinical utilization of α2-adrenoceptor agonists for the treatment of attention-deficit/hyperactivity and related disorders. J Child Adolesc Psychopharmacol. 2013;23:308–19.
Prince JB, Wilens TE, Biederman J, Spencer TJ, Wozniak JR. Clonidine for sleep disturbances associated with attention-deficit hyperactivity disorder: a systemic chart review of 62 cases. J Am Acad Child Adolesc Psychiatry. 1996;35:599–605.
Wilens TE, Biederman J, Spencer T. Clonidine for sleep disturbances associated with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1994;33:424–6.
Jain R, Segal S, Kollins SH, Khayrallah M. Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:171–9.
Blumer JL, Findling RL, Shih WJ, Soubrane C, Reed MD. Controlled clinical trial of zolpidem for the treatment of insomnia associated with attention-deficit/hyperactivity disorder in children 6 to 17 years of age. Pediatrics. 2009;123:e770–6.
Sedky K, Carvalho K, Lippmann S. Attention deficit hyperactivity disorder and sleep disordered breathing in children. J Pediatr Biochem. 2013;3:61–7.
Gruber R, Xi T, Frenette S, Robert M, Vannashin P, Carrier J. Sleep disturbances in prepubertal children with attention deficit hyperactivity disorder: a home polysomnography study. Sleep. 2009;32:343–50.
Amiri S, AbdollahiFakhim S, Lotfi A, Bayazian G, Sohrabpour M, Hemmatjoo T. Effect of adenotonsillectomy on ADHD symptoms of children with adenotonsillar hypertrophy and sleep disordered breathing. Int J Pediatr Otorhinolaryngol. 2015;79:1213–7. This study documented the significant effect of adenotonsillectomy on ADHD children with sleep disordered breathing.
Mostofsky SH, Cooper KL, Kates WR, Denckla MB, Kaufmann WE. Smaller prefrontal and premotor volumes in boys with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2002;52:785–94.
Song SA, Tolisano AM, Cable BB, Camacho M. Neurocognitive outcomes after pediatric adenotonsillectomy for obstructive sleep apnea: a systemic review and meta-analysis. Int J Pediatr Otorhinolaryngol. 2016;83:205–10. This study documented the significant effect of adenotonsillectomy on obstructive sleep apnea, which leads to improved neurocognitive outcomes.
Huang YS, Guilleminault C, Li HY, Yang CM, Wu YY, Chen NH. Attention-deficit/hyperactivity disorder with obstructive sleep apnea: a treatment outcome study. Sleep Med. 2007;8:18–30.
Sedky K, Bennett DS, Carvalho KS. Attention deficit hyperactivity disorder and sleep disordered breathing in pediatric populations: a meta-analysis. Sleep Med Rev. 2014;18:349–56.
Picchietti MA, Picchietti DL. Advances in pediatric restless legs syndrome: iron, genetics, diagnosis and treatment. Sleep Med. 2010;11:643–51.
de Weerd A, Arico I, Silvestri R. Presenting symptoms in pediatric restless legs syndrome patients. J Clin Sleep Med. 2013;9:1077–80.
Oner P, Dirik EB, Taner Y, Caykoylu A, Anlar O. Association between low serum ferritin and restless legs syndrome in patients with attention deficit hyperactivity disorder. Tohoku J Exp Med. 2007;213:269–76.
Paulo Daubian-Nose P, Frank MK, Esteves AM. Sleep disorders: review of the interface between restless legs syndrome and iron metabolism. Sleep Sci. 2014;7:234–7.
Sharon D. Nonpharmacologic management of restless legs syndrome (Willis-Ekbom Disease): myths or science. Sleep Med Clin. 2015;10:263–78.
Silber MH, Becker PM, Earley C, Garcia-Borreguero D, Ondo WG, Medical Advisory Board of the Willis-Ekbom Disease Foundation. Willis-Ekbom Disease Foundation revised consensus statement on the management of restless legs syndrome. Mayo Clin Proc. 2013;88:977–86.
Rinaldi F, Galbiati A, Marelli S, Ferini Strambi L, Zucconi M. Treatment options in intractable restless legs syndrome/Willis-Ekbom Disease (RLS/WED). Curr Treat Options Neurol. 2016;18:7.
Weinstock LB, Walters AS. Restless legs syndrome is associated with irritable bowel syndrome and small intestinal bacterial overgrowth. Sleep Med. 2011;12:610–3.
Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology. 2016;86:1336–43. This article provides the latest updated information regarding restless legs syndrome being as a continuous spectrum with a major genetic contribution and a major comorbid disease of other entities.
Allen RP, Adler CH, Du W, Butcher A, Bregman DB, Earley CJ. Clinical efficacy and safety of IV ferric carboxymaltose (FCM) treatment of RLS: a multi-centred, placebo-controlled preliminary clinical trial. Sleep Med. 2011;12:906–13.
Schneider J, Krafft A, Manconi M, Hübner A, Baumann C, Werth E, et al. Open-label study of the efficacy and safety of intravenous ferric carboxymaltose in pregnant women with restless legs syndrome. Sleep Med. 2015;16:1342–7.
Grim K, Lee B, Sung AY, Kotagal S. Treatment of childhood-onset restless legs syndrome and periodic limb movement disorder using intravenous iron sucrose. Sleep Med. 2013;14:1100–4.
Tilma J, Tilma K, Norregaard O, Ostergaard JR. Early childhood-onset restless legs syndrome: symptoms and effect of oral iron treatment. Acta Paediatr. 2013;105:e221–6.
Konofal E, Lecendreux M, Arnulf I, Mouren MC. Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2004;158:1113–5.
Konofal E, Lecendreux M, Deron J, Marchand M, Cortese S, Zaim M, et al. Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatr Neurol. 2008;38:20–6.
England SJ, Picchietti DL, Couvadelli BV, Fisher BC, Siddigui F, Wagner ML, et al. L-Dopa improves restless legs syndrome and periodic limb movements in sleep but not attention-deficit/hyperactivity disorder in a double-blind trial in children. Sleep Med. 2011;12:471–7.
Ferri R, Bruni O, Novelli L, Picchietti MA, Picchietti DL. Time structure of leg movement activity during sleep in attention-deficit/hyperactivity disorder and effects of levodopa. Sleep Med. 2013;14:359–66.
Walters AS, Mandelbaum DE, Lewin DS, Kugler S, England SJ, Miller M. Dopaminergic therapy in children with restless legs/periodic limb movements in sleep and ADHD. Dopaminergic Therapy Study Group. Pediatr Neurol. 2000;22:182–6.
Konofal E, Arnulf I, Lecendreux M, Mouren MC. Ropiniole in a child with attention-deficit hyperactivity disorder and restless legs syndrome. Pediatr Neurol. 2005;32:350–1.
Gagliano A, Arico I, Calarese T, et al. Restless leg syndrome in ADHD children: levetiracetam as a reasonable therapeutic option. Brain Dev. 2011;33:480–6.
Garcia-Borreguero D, Kohnen R, Silber MH, Winkelman JW, Earley CJ, Högl B, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the international restless legs syndrome study group. Sleep Med. 2013;14:675–84.
Cuffe SP, Visser SN, Holbrook JR, Danielson ML, Geryk LL, Wolraich ML, et al. ADHD and psychiatric comorbidity: functional outcomes in a school-based sample of children. J Atten Disord. 2015. doi:10.1177/1087054715613437.
Becker SP, Langberg JM, Evans SW. Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2015;24:897–907. This article highlights the importance of sleep problems as the important predictor of externalizing behavior and depression in ADHD adolescents.
Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014;53:550–8. This is the first study documenting sleep problems can predict and be predicted by generalized anxiety/depression and oppositional defiant disorder.
Cortese S, Brown TE, Corkum P, Gruber R, O’Brien LM, Stein M, et al. Assessment and management of sleep problems in youths with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2013;52:784–96. This is the expert consensus and meta-analysis regarding the latest assessment and management of sleep problems in youths with ADHD.
Papadopoulos N, Sciberras E, Hiscock H, Mulraney M, McGillivray J, Rinehart N. The efficacy of a brief behavioral sleep intervention in school-aged children with ADHD and comorbid autism spectrum disorder. J Atten Disord. 2015. doi:10.1177/1087054714568565.
Sciberras E, Mulraney M, AndersonV, Rapee RM, Nicholson JM, Efron D, et al. Managing anxiety in children with ADHD using cognitive-behavioral therapy: a pilot randomized controlled trial. J Atten Disord. 2015. doi:10.1177/1087054715584054.
Storebø OJ, Ramstad E, Krogh HB, Nilausen TD, Skoog M, Holmskov M, et al. Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). Cochrane Database Syst Rev. 2015;11:CD009885. This is the latest systemic review and meta-analysis regarding the stimulant effects on children with ADHD.
Storebø OJ, Krogh HB, Ramstad E, Moreira-Maia CR, Holmskov M, Skoog M, et al. Methylphenidate for attention-deficit/hyperactivity disorder in children and adolescents: Cochrane systemic review with meta-analyses and trial sequential analyses of randomized clinical trials. BMJ. 2015;351:h5203. This study focusing on whether methylphenidate beneficial or harmful for treatment of ADHD children concludes caution regarding the use of methylphenidate, since it is associated with an increased risk of non-serious adverse events.
Huang YS, Tsai MH. Long-term outcomes with medications for attention-deficit hyperactivity disorder: current status of knowledge. CNS Drugs. 2011;25:539–54.
Becker SP, Froehlich TE, Epstein JN. Effects of methylphenidate on sleep functioning in children with attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2016;37(5):395–404.
Wang LJ, Chen CK, Huang YS. Gender differences in the behavioral symptoms and neuropsychological performance of patients with attention-deficit/hyperactivity disorder treated with methylphenidate: a two-year follow-up study. J Child Adolesc Psychopharmacol. 2015;25:501–8.
Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep Med. 2010;11:652–8.
Wang LJ, Chen CK, Huang YS. Neurocognitive performance and behavioral symptoms in patients with attention-deficit/hyperactivity disorder during twenty-four months of treatment with methylphenidate. J Child Adolesc Psychopharmacol. 2015;25:246–53.
Lecendreux M, Lavault S, Lopez R, Inocente CO, Konofal E, Cortese S, et al. Attention-deficit/hyperactivity disorder (ADHD) symptoms in pediatric narcolepsy: a cross-sectional study. Sleep. 2015;38:1285–95.
Coghill DR, Banaschewski T, Lecendreux M, Soutullo C, Zuddas A, Adeyi B, et al. Post hoc analyses of the impact of previous medication on the efficacy of lisdexamfetamine dimesylate in the treatment of attention-deficit/hyperactivity disorder in a randomized, controlled trial. Neuropsychiatr Dis Treat. 2014;10:2039–47.
Simonoff E, Taylor E, Baird G, Bernard S, Chadwick O, Liang H, et al. Randomized controlled double-blind trial of optimal dose methylphenidate in children and adolescents with severe attention deficit hyperactivity disorder and intellectual disability. J Child Psychol Psychiatry. 2013;54:527–35.
Gruner JA, Marcy VR, Lin YG, Bozyczko-Coyne D, Marino MJ, Gasior M. The roles of dopamine transport inhibition and dopamine release facilitation in wake enhancement and rebound hypersomnolence induced by dopaminergic agents. Sleep. 2009;32:1425–38.
Roskell NS, Setyawan J, Zimovetz EA, Hodgkins P. Systemic evidence synthesis of treatments for ADHD in children and adolescents: indirect treatment comparisons of lisdexamfetamine with methylphenidate and atomoxetine. Curr Med Res Opin. 2014;30:1673–85.
Coghill DR, Caballero B, Sorooshian S, Civil R. A systemic review of the safety of lisdexamfetamine dimesylate. CNS Drugs. 2014;28:497–511.
Dittmann RW, Cardo E, Nagy P, Anderson CS, Adeyi B, Caballero B, et al. Treatment response and remission in a double-blind, randomized, head-to-head study of lisdexamfetamine dimesylate and atomoxetine in children and adolescents with attention-deficit hyperactivity disorder. CNS Drugs. 2014;28:1059–69. This study compared the efficacy and side effects of lisdexamfetamine dimesylate and atomoxetine in children with ADHD.
Warrer P, Thomsen PH, Dalsgaard S, Hansen EH, Aagaard L, Wallach Kildemoes H, et al. Switch in therapy from methylphenidate to atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: an analysis of patient records. J Child Adolesc Psychopharmacol. 2016;26(4):354–61.
Prasad S, Steer C. Switching from neurostimulant therapy to atomoxetine in children and adolescents with attention-deficit hyperactivity disorder: clinical approaches and review of current available evidence. Pediatr Drugs. 2008;10:39–47.
Schwartz S, Correll CU. Efficacy and safety of atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: results from a comprehensive meta-analysis and metaregression. J Am Acad Child Adolesc Psychiatry. 2014;53:174–87. This study using meta-analysis documented the efficacy and safety of atomoxetine, and concluded it as the alternative choice for children and adolescents with ADHD.
Hervas A, Huss M, Johnson M, McNicholas F, van Stralen J, Sreckovic S, et al. Efficacy and safety of extended-release guanfacine hydrochloride in children and adolescents with attention-deficit/hyperactivity disorder: a randomized, controlled, phase III trial. Eur Neuropsychopharmacol. 2014;24:1861–72.
Stein MA, Sikirica V, Weiss MD, Robertson B, Lyne A, Newcorn JH. Does guanfacine extended release impact functional impairment in children with attention-deficit/hyperactivity disorder? Results from a randomized controlled trial. CNS Drugs. 2015;29:953–62. This updated RCT documented guanfacine extended release treatment is associated with reductions in ADHD symptoms, and has tolerable adverse events.
Dittmann RW, Cardo E, Nagy P, Anderson CS, Bloomfield R, Caballero B, et al. Efficacy and safety of lisdexamfetamine dimesylate and atomoxetine in the treatment of attention-deficit/hyperactivity disorder: a head-to-head, randomized, double-blind, phase IIIb study. CNS Drugs. 2013;27:1081–92.
Daviss WB, Patel NC, Robb AS, McDermott MP, Bukstein OG, Pelham Jr WE, et al. Clonidine for attention-deficit/hyperactivity disorder: II. ECG changes and adverse events analysis. J Am Acad Child Adolesc Psychiatry. 2008;47:189–98.
Ming X, Mulvey M, Mohanty S, Patel V. Safety and efficacy of clonidine and clonidine extended-release in the treatment of children and adolescents with attention deficit and hyperactivity disorders. Adolesc Health Med Ther. 2011;2:105–12.
Graham J, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, et al. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20:17–37.
Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51.
Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. J Am Acad Child Adolesc Psychiatry. 2006;45:512–9.
Cortese S, Holtmann M, Banaschewski T, Buitelaar J, Coghill D, Dittmann RW, et al. Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry. 2013;54:227–46.
Hvolby A. Associations of sleep disturbance with ADHD: implications for treatment. Atten Defic Hyperact Disord. 2015;7:1–18.
Kim HW, Yoon IY, Cho SC, Kim BN, Chung S, Lee H, et al. The effect of OROS methylphenidate on the sleep of children with attention-deficit/hyperactivity disorder. Int Clin Psychopharmacol. 2010;25:107–15.
Wilens TE, Bukstein O, Brams M, Cutler AJ, Childress A, Rugino T, et al. A controlled trial of extended-release guanfacine and psychostimulants for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51:74–85.
Newcorn JH, Stein MA, Childress AC, Youcha S, White C, Enright G, et al. Randomized, double-blind trial of guanfacine extended release in children with attention-deficit/hyperactivity disorder: morning or evening administration. J Am Acad Child Adolesc Psychiatry. 2013;52:921–30.
Sallee FR, McGough J, Wigal T, Donahue J, Lyne A, Biederman J, et al. Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48:155–65.
Block SL, Kelsey D, Coury D, Lewis D, Quintana H, Sutton V, et al. Once-daily atomoxetine for treating pediatric attention-deficit/hyperactivity disorder: comparison of morning and evening dosing. Clin Pediatr. 2009;48:723–33.
Cortese S, Panei P, Arcieri R, Germinario EA, Capuano A, Margari L, et al. Safety of methylphenidate and atomoxetine in children with attention-deficit/hyperactivity disorder (ADHD): data from the Italian National ADHD Registry. CNS Drugs. 2015;29:865–77.
Shang CY, Pan YL, Lin HY, Huang LW, Gau SS. An open-label, randomized trial of methylphenidate and atomoxetine treatment in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2015;25:566–73.
Mohammadi MR, Mostafavi SA, Keshavarz SA, Eshraghian MR, Hosseinzadeh P, Hosseinzadeh-Attar MJ, et al. Melatonin effects in methylphenidate treated children with attention deficit hyperactivity disorder: a randomized double blind clinical trial. Iran J Psychiatry. 2012;7:87–92.
Kratochvil CJ, Lake M, Pliszka SR, Walkup JT. Pharmacological management of treatment-induced insomnia in ADHD. J Am Acad Child Adolesc Psychiatry. 2004;44:499–501.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Yunlin Chang Gung Memorial Hospital, Yunlin, Taiwan, Republic of China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ming-Horng Tsai, Jen-Fu Hsu, and Yu-Shu Huang declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Tsai, MH., Hsu, JF. & Huang, YS. Sleep Problems in Children with Attention Deficit/Hyperactivity Disorder: Current Status of Knowledge and Appropriate Management. Curr Psychiatry Rep 18, 76 (2016). https://doi.org/10.1007/s11920-016-0711-4
Published:
DOI: https://doi.org/10.1007/s11920-016-0711-4