Abstract
Purpose of Review
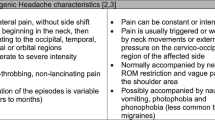
The International Classification of Headache Disorders provides an extensive framework to classify headaches. Physiotherapy is indicated if neuromusculoskeletal dysfunctions are involved in the pathophysiology. Maladaptive postures seem a dominant trigger in tension-type and cervicogenic headache. Yet, outcomes following physiotherapy vary. The absence of protocol studies to identify determinants concerning the role of spinal posture in headache might explain such variability. Hence, multi-dimensional profiling of patients with headache based on interactions between spinal posture, psychosocial and lifestyle factors might be essential. Therefore, the aim of this paper was to perform a comprehensive review to find support for the paradigm of spinal posture triggering episodic headache based on a multi-dimensional view on tension-type and cervicogenic headache including modern pain neuroscience.
Recent Findings
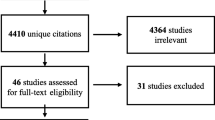
A review was conducted to support spinal posture-induced episodic headache. Pubmed, Web of Science, Pedro and the Cochrane database were explored based on the following ‘Mesh’ or ‘Topics’: ‘Headache’, ‘Posture’, ‘Spine’, ‘Psychosocial’, ‘Lifestyle’. The contemporary review of neuroanatomical, biomechanical and non-nociceptive pathways, with integration of modern pain neuroscience in tension-type and cervicogenic headache, supports spinal posture as a trigger for episodic headache. Maladaptive postures can activate C1-C3 nociceptors. Convergence with trigeminal afferents at the trigeminocervical nucleus could explain spinal headache. Interactions with psychosocial and lifestyle factors might contribute to peripheral and central sensitisation.
Summary
Neuroanatomical, biomechanical and non-nociceptive pathways seem to justify profiling patients based on a postural trigger. Further research is needed to determine the contribution of postural dysfunctions in headache and the effect of specific interventions.


Similar content being viewed by others
Abbreviations
- TTH:
-
Tension-type headache
- CeH:
-
Cervicogenic headache
- FHP:
-
Forward head posture
- RCPmi:
-
Rectus capitis posterior minor
- CS:
-
Central sensitisation
- DNIC:
-
Diffuse noxious inhibitory control
- HPA:
-
Hypothalamic-pituitary-adrenal
- ANS:
-
Autonomic nervous system
- PAG:
-
Periaqueductal grey matter
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
World Health Organization. Lifting The Burden. Atlas of headache disorders and resources in the world. 2011. http://www.who.int/mental_health/management/atlas_headache_disorders. Accessed 20 May 2018.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
Smitherman TA, Davis RE, Walters AB, Young J, Houle TT. Anxiety sensitivity and headache: diagnostic differences, impact, and relations with perceived headache triggers. Cephalalgia. 2015;35(8):710–21.
Martin P. Classification of headache disorders: extending to a multiaxial system. Headache. 2016;56:1649–52.
Suhr J, Spickard B. Pain is a highly subjective sensation with a complex and often non-linear relationship between nociceptive input and pain perception. Clin Neuropsychol. 2012;26(7):1128–41.
de Tommaso M, Fernández-de-Las-Penas C. Tension type headache. Curr Rheumatol Rev. 2016;12(2):127–39.
Olesen J. Problem areas in the international classification of headache disorders, 3rd edition (beta). Cephalalgia. 2014;34(14):1193–9.
Farmer PK, Snodgrass SJ, Buxton AJ, Rivett DA. An investigation of cervical spinal posture in cervicogenic headache. Phys Ther. 2015;95(2):212–22.
Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study. Cephalalgia. 2005;26:314–9.
Watson DH, Trott PH. Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13:272–84.
Bogduk N. The neck and headaches. Neurol Clin. 2014;32(2):471–87.
Moore CS, Sibbritt DW, Adams J. A critical review of manual therapy use for headache disorders: prevalence, profiles, motivations, communication and self-reported effectiveness. BMC Neurol. 2017;17(1):61.
Mesa-Jiménez JA, Lozano-López C, Angulo-Díaz-Parreño S, Rodríguez-Fernández ÁL, De-la-Hoz-Aizpurua JL, Fernández-de-Las-Peñas C. Multimodal manual therapy vs. pharmacological care for management of tension type headache: a meta-analysis of randomized trials. Cephalalgia. 2015;35(14):1323–32.
Liebert A, Rebbeck T, Elias S, Hawkins D, Adams R. Musculoskeletal physiotherapists' perceptions of non-responsiveness to treatment for cervicogenic headache. Physiother Theory Pract. 2013;29(8):616–29.
• Luedtke K, Boissonnault W, Caspersen N, Castien R, Chaibi A, Falla D, et al. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: a Delphi study. Man Ther. 2016;23:17–24 A very good critical view on current physical therapy techniques applied in headache and their limitations.
Jones GT. Psychosocial vulnerability and early life adversity as risk factors for central sensitivity syndromes. Curr Rheumatol Rev. 2016;12(2):140–53.
• Adams LM, Turk DC. Psychosocial factors and central sensitivity syndromes. Curr Rheumatol Rev. 2015;11(2):96–108 An important contribution that stimulates including psychosocial variables during patient examination.
Villanueva L. Diffuse noxious inhibitory control (DNIC) as a tool for exploring dysfunction of endogenous pain modulatory systems. Pain. 2009;3:161–2.
Drummond PD, Knudsen L. Central pain modulation and scalp tenderness in frequent episodic tension-type headache. Headache. 2011;51(3):375–83.
Bezov D, Ashina S, Jensen R, Bendtsen L. Pain perception studies in tension-type headache. Headache. 2011;51(2):262–71.
Mongini F, Rota E, Evangelista A, Ciccone G, Milani C, Ugolini A, et al. Personality profiles and subjective perception of pain in head pain patients. Pain. 2009;44:125–9.
Loyen A, van der Ploeg HP, Bauman A, Brug J, Lakerveld J. European sitting championship: prevalence and correlates of self-reported sitting time in the 28 European Union member states. PLoS One. 2016;11(3):e0149320.
Malinska M, Bugajska J. The influence of occupational and non-occupational factors on the prevalence of musculoskeletal complaints in users of portable computers. Int J Occup Saf Ergon. 2010;16:337–43.
Westgaard RH, Winkel J. Guidelines for occupational musculoskeletal load as a basis for intervention: a critical review. Appl Ergon. 1996;27(2):79–88.
Pooriput W, Bala R, Prawit J. Internal oblique and transversus abdominis muscle fatigue induced by slumped sitting posture after 1 hour of sitting in office workers. Saf Health Work. 2016;7(1):49–54.
Black KM, McClure P, Polansky M. The influence of different sitting positions on cervical and lumbar posture. Spine (Phila Pa 1976). 1996;21(1):65–70.
Fernández-de-Las-Peñas C, Cuadrado ML. Physical therapy for headaches. Cephalalgia. 2016;36(12):1134–42.
McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clin Biomech. 1992;7(1):43–6.
Fernandez-de-las-Penas C, Cuadrado ML, Pareja JA. Myofascial trigger points, neck mobility, and forward head posture in episodic tension-type headache. Headache. 2007;47:662–72.
Caneiro JP, O’Sullivan P, Burnett A, Barach A, O’Neil D, Tveit O, et al. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. 2010;15:54–60.
Van Houdenhove JB, Oostendorp RA. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Man Ther. 2010;15(2):135–41.
Smart KM, Blake C, Staines A, Doody C. Clinical indicators of 'nociceptive', 'peripheral neuropathic' and 'central' mechanisms of musculoskeletal pain. A Delphi survey of expert clinicians. Man Ther. 2010;15(1):80–7.
Sluka KA. Pain mechanisms involved in musculoskeletal disorders. J Orthop Sports Phys Ther. 1996;4(4):240–54.
Hack GD, Hallgren RC. Chronic headache relief after section of suboccipital muscle dural connections: a case report. Headache. 2004;44(1):84–9.
Kahkeshani K, Ward PJ. Connection between the spinal dura mater and suboccipital musculature: evidence for the myodural bridge and a route for its dissection—a review. Clin Anat. 2010;25:415–22.
Choi JC, Chung M, Lee YD. Modulation of pain sensation by stress-related testosterone and cortisol. Anaesthesia. 2012;67(10):1146–51.
Peck D, Buxton DF, Nitz A. A comparison of spindle concentrations in large and small muscles acting in parallel combinations. J Morphol. 1984;180:243–52.
Hallgren RC, Rowan JR, Bai P, Pierce SJ, Shafer-Crane GA, Prokop LL. Activation of rectus capitis posterior major muscles during voluntary retraction of the head in asymptomatic subjects. J Manip Physiol Ther. 2014;37(6):433–40.
Richmond F, Singh K, Corneil B. Marked non-uniformity of fiber-type composition in the primate suboccipital muscle obliquus capitis inferior. Exp Brain Res. 1999;125(1):14–8.
Liu J, Thornell L, Pedrosa-Domellöfet F. Muscle spindles in the deep muscles of the human neck: a morphological and immunocytochemical study. J Histochem Cytochem. 2003;51(2):175–86.
Corneil BD, Olivier E, Munoz DP. Neck muscle responses to stimulation of monkey superior colliculus. I. Topography and manipulation of stimulation parameters. J Neurophysiol. 2002;88(4):1980–99.
Hirai T, Hongo S, Sasaki S, Yamashita M, Yoshida K. Neck muscle afferent input to spinocerebellar tract cells of the central cervical nucleus in the cat. Exp Brain Res. 1984;55(2):286–300.
Peterson BW. Current approaches and future directions to understanding control of head movement. Prog Brain Res. 2004;143:369–81.
Field S, Treleaven J, Jull G. Standing balance: a comparison between idiopathic and whiplash induced neck pain. Man Ther. 2008;(3, 3):183–91.
Leistad RB, Stovner LJ, White LR, Nilsen KB, Westgaard RH, Sand T. Noradrenaline and cortisol changes in response to low-grade cognitive stress differ in migraine and tension-type headache. J Headache Pain. 2007;8(3):157–66.
Hallgren RC, Greenman PE, Rechtien JJ. Atrophy of suboccipital muscles in patients with chronic pain: a pilot study. J Am Osteopath Assoc. 1994;12:1032–8.
Khayatzadeh S, Kalmanson OA, Schuit D, Havey RM, Voronov LI, Ghanayem AJ, et al. Cervical spine muscle-tendon unit length differences between neutral and forward head postures: biomechanical study using human cadaveric specimens. Phys Ther. 2017;97(7):756–66.
Luedtke K. Does the rectus capitis posterior minor muscle contribute to the pathogenesis of chronic headache? Cephalalgia. 2017;37(11):1025–6.
•• Palomeque-del-Cerro L, Arraez-Aybar LA, Rodrıguez-Blanco C, Guzman-Garcıa R, Menendez-Aparicio M, Oliva-Pascual-Vaca A. A systematic review of the soft-tissue connections between neck muscles and dura mater. Spine. 2016;2(1):49–54 A very good view of possible pathophysiological mechanisms for cervicogenic headache.
Meyer RA, Campbell JN, Raja SN. Peripheral neural mechanisms of nociception. Textbook of pain. 3rd ed. London: Curchill Livingstone; 1995.
Nijs J, Torres-Cueco R, van Wilgen CP, Girbes EL, Struyf F, Roussel N, et al. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician. 2014;17:447–57.
Nijs J, Apeldoorn A, Hallegraeff H, Clark J, Smeets R, Malfleit A, et al. Low back pain: guidelines for the clinical classification of predominant neuropathic, nociceptive, or central sensitization pain. Pain Physician. 2015;18(3):333–46.
Chua NHL, van Suijlekom HA, Vissers KC, Arendt-Nielsen L, Wilder-Smith OH. Differences in sensory processing between chronic cervical zygapophysial joint pain patients with and without cervicogenic headache. Cephalalgia. 2011;31(8):953–63.
Yunus MB. Role of central sensitization in symptoms beyond muscle pain, and the evaluation of a patient with widespread pain. Best Pract Res Clin Rheumatol. 2007;1(3):481–9.
Cady RK. The convergence hypothesis. Headache. 2007;47:S44–51.
Richards KV, Beales DJ, Smith AJ, O'Sullivan PB, Straker LM. Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Phys Ther. 2016;96(10):1576–87.
Lundy-Ekman L. Neuroscience fundamentals for rehabilitation. 5th ed. St. Louis: Elsevier; 2018.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624.
Gallagher L, McAuley J, Moseley GL. A randomized controlled trial of using a book of metaphors to reconceptualise pain and decrease catastrophizing in people with chronic pain. Clin J Pain. 2013;29:20–5.
Rahim-Williams B, Riley JL, Williams AK, Fillingim RB. A quantitative review of ethnic group differences in experimental pain response: do biology, psychology, and culture matter? Pain Med. 2012;13(4):522–40.
Paananen M, O'Sullivan P, Straker L, Beales D, Coenen P, Karppinen J, et al. A low cortisol response to stress is associated with musculoskeletal pain combined with increased pain sensitivity in young adults: a longitudinal cohort study. Arthritis Res Ther. 2015;10(17):355.
Glass JJ, Glaros AG. Autonomic dysregulation in headache patients. Appl Psychophysiol Biofeedback. 2013;38:257–63.
Mosek A, Novak V, Opfer-Gehrking TL, Swanson JW, Low PA. Autonomic dysfunction in migraineurs. Headache. 1999;39:108–17.
Benarroch EE. Pain-autonomic interactions. Neurol Sci. 2006;7:S130–3.
Nair S, Sagar M, Sollers J, Consedine N, Broadbent E. Do slumped and upright postures affect stress responses? A randomized trial. Health Psychol. 2015;34(6):632–41.
Wilson VE, Peper E. The effects of upright and slumped postures on the recall of positive and negative thoughts. Appl Psychophysiol Biofeedback. 2004;29:189–95.
Wijma AJ, van Wilgen CP, Meeus M, Nijs J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: the first step in pain neuroscience education. Physiother Theory Pract. 2016;32(5):368–84.
Hall T, Robinson K. The flexion-rotation test and active cervical mobility–a comparative measurement study in cervicogenic headache. Man Ther. 2004;9(4):197–202.
Sjaastad O, Bakketeig L. Tension-type headache: comparison with migraine without aura and cervicogenic headache. The Vaga study of headache epidemiology. Funct Neurol. 2008;23(2):71–6.
Castien RF, van der Windt DA, Blankenstein AH, Heymans MW, Dekker J. Clinical variables associated with recovery in patients with chronic tension-type headache after treatment with manual therapy. Pain. 2012;3(4):893–9.
Askew R, Kibelstis C, Overbaugh S, Walker S, Nixon-Cave K, Shepard KF. Physical therapists’ perception of patients’ pain and its effect on management. Physiother Res Int. 1998;3(1):37–57.
Overmeer T, Linton SJ, Boersma K. Do physical therapists recognise established risk factors? Swedish physical therapists’ evaluation in comparison to guidelines. Physiother. 2004;90(1):35–41.
Lee CH, Lee S, Shin G. Reliability of forward head posture evaluation while sitting, standing, walking and running. Hum Mov Sci. 2017;55:81–6.
McDonnell MK, Sahrmann SA, Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2005;35(1):3–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sarah Mingels, Wim Dankaerts, and Marita Granitzer declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hot Topics in Pain and Headache
Rights and permissions
About this article
Cite this article
Mingels, S., Dankaerts, W. & Granitzer, M. Is There Support for the Paradigm ‘Spinal Posture as a Trigger for Episodic Headache’? A Comprehensive Review. Curr Pain Headache Rep 23, 17 (2019). https://doi.org/10.1007/s11916-019-0756-2
Published:
DOI: https://doi.org/10.1007/s11916-019-0756-2