Abstract
Purpose of Review
This review describes existing evidence addressing the potential modulation of pre-exposure prophylaxis (PrEP) products, specifically 1% tenofovir (TFV) gel and oral tenofovir-based PrEP, by vaginal dysbiosis and discusses future considerations for delivering novel, long-acting PrEP products to women at high risk for vaginal dysbiosis and HIV.
Recent Findings
We describe results from analyses investigating the modification of PrEP efficacy by vaginal dysbiosis and studies of biological mechanisms that could render PrEP ineffective in the presence of specific microbiota. A secondary analysis from the CAPRISA-004 cohort demonstrated that there is no effect of the 1% TFV gel in the presence of non-Lactobacillus dominant microbiota. Another recent analysis comparing oral tenofovir-based PrEP efficacy among women with and without bacterial vaginosis in the Partners PrEP Study found that oral PrEP efficacy is not modified by bacterial vaginosis. Gardnerella vaginalis, commonly present in women with vaginal dysbiosis, can rapidly metabolize TFV particularly when it is locally applied and thereby prevent TFV integration into cells. Given that vaginal dysbiosis appears to modulate efficacy for 1% TFV gel but not for oral tenofovir-based PrEP, vaginal dysbiosis is potentially less consequential to HIV protection from TFV in the context of systemic drug delivery and high product adherence.
Summary
Vaginal dysbiosis may undermine the efficacy of 1% TFV gel to protect women from HIV but not the efficacy of oral PrEP. Ongoing development of novel ring, injectable, and film-based PrEP products should investigate whether vaginal dysbiosis can reduce efficacy of these products, even in the presence of high adherence.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Adimora AA, Ramirez C, Auerbach JD, Aral SO, Hodder S, Wingood G, et al. Preventing HIV infection in women. J Acquir Immune Defic Syndr. 2013;63(0 2):S168–73. doi:10.1097/QAI.0b013e318298a166.
Ramjee G, Daniels B. Women and HIV in sub-Saharan Africa. AIDS Res Ther. 2013;10(1):30. doi:10.1186/1742-6405-10-30.
Underhill K, Operario D, Mimiaga MJ, Skeer MR, Mayer KH. Implementation science of pre-exposure prophylaxis: preparing for public use. Curr HIV/AIDS Rep. 2010;7(4):210–9. doi:10.1007/s11904-010-0062-4.
Celum CL, Delany-Moretlwe S, McConnell M, van Rooyen H, Bekker L-G, Kurth A, et al. Rethinking HIV prevention to prepare for oral PrEP implementation for young African women. J Int AIDS Soc. 2015;18(4 Suppl 3):20227. doi:10.7448/IAS.18.4.20227.
Marcus JL, Volk JE, Pinder J, Liu AY, Bacon O, Hare CB, et al. Successful implementation of HIV preexposure prophylaxis: lessons learned from three clinical settings. Curr HIV/AIDS Rep. 2016;13(2):116–24. doi:10.1007/s11904-016-0308-x.
Cáceres CF, O’Reilly KR, Mayer KH, Baggaley R. PrEP implementation: moving from trials to policy and practice. J Int AIDS Soc. 2015;18(4 Suppl 3):20222. doi:10.7448/IAS.18.4.20222.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi:10.1056/NEJMoa1108524.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. doi:10.1056/NEJMoa1110711.
• Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med. 2016;375:2121–32. doi:10.1056/NEJMoa1506110. This article presents the primary analysis from the ASPIRE phase 3, randomized, double-blind, placebo-controlled trial of the monthly dapivirine ring. The study demonstrated that the dapivirine ring can prevent HIV acquisition, particularly for women over 21 years of age.
• Nel A, van Niekerk N, Kapiga S, Bekker L-G, Gama C, Gill K, et al. Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med. 2016;375(22):2133–43. doi:10.1056/NEJMoa1602046. This article presents the primary analysis from the phase 3, randomized, double-blind, placebo-controlled trial of the monthly dapivirine ring in South Africa and Uganda. The study demonstrated that the dapivirine ring can prevent HIV acquisition and did not find a difference in efficacy by age group.
• Schlesinger E, Johengen D, Luecke E, Rothrock G, McGowan I, van der Straten A, et al. A tunable, biodegradable, thin-film polymer device as a long-acting implant delivering tenofovir alafenamide fumarate for HIV pre-exposure prophylaxis. Pharm Res. 2016;33(7):1649–56. doi:10.1007/s11095-016-1904-6. This article describes the use of a thin-film polymer device (TFPD) as a biodegradable implant for PrEP. The device demonstrated linear drug release for up to 60 or 90 days, depending on desired drug quantity.
Akil A, Agashe H, Dezzutti CS, Moncla BJ, Hillier SL, Devlin B, et al. Formulation and characterization of polymeric films containing combinations of antiretrovirals (ARVs) for HIV prevention. Pharm Res. 2015;32(2):458–68. doi:10.1007/s11095-014-1474-4.
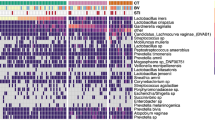
•• Klatt NR, Cheu R, Birse K, Zevin AS, Perner M, Noel-Romas L, et al. Vaginal bacteria modify HIV tenofovir microbicide efficacy in African women. Science. 2017;356:938–45. doi:10.1126/science.aai9383. This article presents findings on associations between vaginal microbiota and tenofovir gel microbicide efficacy in the CAPRISA-004 trial. Gel-based PrEP was not efficacious in women with non- Lactobacillus dominant microbiota, potentially because Gardnerella vaginalis present in these women could metabolize tenofovir.
Atashili J, Poole C, Ndumbe PM, Adimora AA, Smith JS. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS. 2008;22(12):1493–501. doi:10.1097/QAD.0b013e3283021a37.
Passmore J-AS, Jaspan HB, Masson L. Genital inflammation, immune activation and risk of sexual HIV acquisition. Curr Opin HIV AIDS. 2016;11(2):156–62. doi:10.1097/COH.0000000000000232.
• Masese L, Baeten JM, Richardson BA, Bukusi E, John-Stewart G, Graham SM, et al. Changes in the contribution of genital tract infections to HIV acquisition among Kenyan high-risk women from 1993 to 2012. AIDS. 2015;29(9):1077–85. doi:10.1097/QAD.0000000000000646. This article presents findings on associations between genital tract infections and HIV incidence among women in Kenya during a 20-year follow-up period. The estimated PAR% for bacterial vaginosis and intermediate microbiota was high during the follow-up period.
McClelland RA. Vaginal microbiome and susceptibility to HIV [Abstract #54]. Oral Presentation at: Conference on Retroviruses and Opportunistic Infections (CROI) 2017; March 4-7, 2017;Seattle, WA, USA.
• Gosmann C, Anahtar MN, Handley SA, Farcasanu M, Abu-Ali G, Bowman BA, et al. Lactobacillus-deficient cervicovaginal bacterial communities are associated with increased HIV acquisition in young South African women. Immunity. 2017;46(1):29–37. doi:10.1016/j.immuni.2016.12.013. This article presents findings from a prospective cohort study examining associations between genital inflammation and HIV acquisition among South African women. Having diverse vaginal microbiota (not Lactobacillus -dominant) was associated with elevated HIV risk and increased activated CD4+ T cells.
•• Passmore JS, Williams B. Role of vaginal microbiota in genital inflammation and enhancing HIV acquisition in women [Abstract #TUSS0605]. Oral Presentation at AIDS 2016; July 18-22, 2016; Durban, South Africa. In a case-control study with women from the CAPRISA-004 trial, HIV-infected cases were found to have an upregulation in inflammatory cytokines prior to HIV acquisition. Specifically, bacterial vaginosis with an abundance of Prevotella bivia was associated with inflammatory cytokine response and increased HIV risk.
Burgener A, McGowan I, Klatt NR. HIV and mucosal barrier interactions: consequences for transmission and pathogenesis. Curr Opin Immunol. 2015;36:22–30. doi:10.1016/j.coi.2015.06.004.
• Anahtar MN, Byrne EH, Doherty KE, Bowman BA, Yamamoto HS, Soumillon M, et al. Cervicovaginal bacteria are a major modulator of host inflammatory responses in the female genital tract. Immunity. 2015;1(5):965–76. doi:10.1016/j.immuni.2015.04.019. In a prospective cohort study with 146 HIV-negative South African women, high diversity of vaginal microbiota was correlated with genital pro-inflammatory cytokine response. In addition, there were significantly more CCR5+ CD4+ T cells found in the endocervical canal of women with higher cytokine responses (which tended to also be those with the most diverse vaginal flora).
• Dimitrov DT, Mâsse BR, Donnell D. PrEP adherence patterns strongly affect individual HIV risk and observed efficacy in randomized clinical trials. J Acquir Immune Defic Syndr. 2016;72(4):444–51. doi:10.1097/QAI.0000000000000993. This simulation study presents findings on expected PrEP efficacy associated with different levels of oral pill adherence. Pill-taking patterns were found to have a large effect on estimated PrEP efficacy, after comparing model findings with results from PrEP randomized controlled trials.
• Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509–18. doi:10.1056/NEJMoa1402269. This article presents the primary analysis from the VOICE randomized, placebo-controlled trial of oral tenofovir disoproxil fumarate, oral tenofovir-emtricitabine, or 1% tenofovir gel as HIV PrEP. The study did not find oral or gel-based regimens to be efficacious in preventing HIV; however, adherence to the daily regimens was low.
Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22. doi:10.1056/NEJMoa1202614.
Hanscom B, Janes HE, Guarino PD, Huang Y, Brown ER, Chen YQ, et al. Preventing HIV-1 infection in women using oral pre-exposure prophylaxis: a meta-analysis of current evidence. J Acquir Immune Defic Syndr. 2016;73(5):606–8. doi:10.1097/QAI.0000000000001160.
Celum C, Baeten JM. Tenofovir-based pre-exposure prophylaxis for HIV prevention: evolving evidence. Curr Opin Infect Dis. 2012;25(1):51–7. doi:10.1097/QCO.0b013e32834ef5ef.
Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74. doi:10.1126/science.1193748.
• Rees H, Delany-Moretlwe S, Lombard C, Baron D, Panchia R, Myer L, et al. FACTS 001 phase III trial of pericoital tenofovir 1% gel for HIV prevention in women [Abstract #26LB]. Oral Presentation at: Conference on Retroviruses and Opportunistic Infections (CROI) 2015; February 23-26, 2015. Seattle, WA, USA. In the FACTS 001, phase III, multi-center, double-blind, randomized, placebo-controlled trial, 1% tenofovir gel was not found to be efficacious for HIV prevention among South African women. While the gel effectiveness was highest in women who reported product use, overall adherence was low in this cohort.
Friend DR, Kiser PF. Assessment of topical microbicides to prevent HIV-1 transmission: concepts, testing, lessons learned. Antivir Res. 2013;99(3):391–400. doi:10.1016/j.antiviral.2013.06.021.
Montgomery ET, Mensch B, Musara P, Hartmann M, Woeber K, Etima J, et al. Misreporting of product adherence in the MTN-003/VOICE trial for HIV prevention in Africa: participants’ explanations for dishonesty. AIDS Behav. 2017;21(2):481–91. doi:10.1007/s10461-016-1609-1.
•• Heffron RA, McClelland RS, Balkus J, Celum CL, Cohen C, Mugo N, et al. Daily oral PrEP is effective among women with abnormal vaginal microbiota [Abstract #85]. Oral Presentation at: Conference on Retroviruses and Opportunistic Infections (CROI) 2017; March 4-7, 2017; Seattle, WA, USA. This work examines the associations between vaginal microbiota and oral PrEP efficacy in the Partners PrEP Study. Oral PrEP efficacy was not significantly different among women with bacterial vaginosis and intermediate microbiota, compared with women who had normal microbiota.
Hendrix CW, Chen BA, Guddera V, Hoesley C, Justman J, Nakabiito C, et al. MTN-001: randomized pharmacokinetic cross-over study comparing tenofovir vaginal gel and oral tablets in vaginal tissue and other compartments. PLoS One. 2013;8(1):e55013. doi:10.1371/journal.pone.0055013.
•• Hillier SL, Meyn L, Bunge K, Austin M, Moncla BJ, Dezzutti C, et al. Impact of vaginal microbiota on genital tissue and plasma concentrations of tenofovir [Abstract #86LB]. Oral Presentation at: Conference on Retroviruses and Opportunistic Infections (CROI) 2017; March 4-7, 2017; Seattle, WA, USA. In the FAME-04 study of tenofovir gel and film, women with higher concentrations of Gardnerella vaginalis were found to have lower tenofovir drug levels in cervicovaginal fluid and plasma after 7 days. This study highlights the potential for Gardnerella vaginalis to rapidly metabolize PrEP.
•• Zevin AS, Xie IY, Birse K, Arnold K, Romas L, Westmacott G, et al. Microbiome composition and function drives wound-healing impairment in the female genital tract. PLoS Pathog. 2016;12(9):e1005889. doi:10.1371/journal.ppat.1005889. This article presents findings on epithelial barrier integrity and immune activation among women with Gardnerella vaginalis dominant vaginal microbiota, compared with women with Lactobacillus dominant microbiota. Women with Gardnerella vaginalis dominant microbiota had increased abundance of membrane transport proteins which could influence drug metabolism.
Cottrell ML, Srinivas N, Kashuba ADM. Pharmacokinetics of antiretrovirals in mucosal tissue. Expert Opin Drug Metab Toxicol. 2015;11(6):893–905. doi:10.1517/17425255.2015.1027682.
• Kashuba ADM, Gengiah TN, Werner L, Yang K-H, White NR, Karim QA, et al. Genital tenofovir concentrations correlate with protection against HIV infection in the CAPRISA 004 trial: importance of adherence for microbicide effectiveness. J Acquir Immune Defic Syndr. 2015;69(3):264–9. doi:10.1097/QAI.0000000000000607. This article presents findings from a case-control study with the CAPRISA-004 trial cohort. Significantly fewer HIV-infected cases were found to have cervicovaginal fluid tenofovir concentrations >100 ng/mL compared with uninfected controls. Plasma concentrations were <1 ng/mL in all women receiving the 1% tenofovir gel.
Mayer KH, Maslankowski LA, Gai F, El-Sadr WM, Justman J, Kwiecien A, et al. Safety and tolerability of tenofovir vaginal gel in abstinent and sexually active HIV-infected and uninfected women. AIDS. 2006;20(4):543–51. doi:10.1097/01.aids.0000210608.70762.c3.
Patterson KB, Prince HA, Kraft E, Jenkins AJ, Shaheen NJ, Rooney JF, et al. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci Transl Med. 2011;3(112):112re4. doi:10.1126/scitranslmed.3003174.
• Cottrell ML, Yang KH, HMA P, Sykes C, White N, Malone S, et al. A translational pharmacology approach to predicting outcomes of preexposure prophylaxis against HIV in men and women using tenofovir disoproxil fumarate with or without emtricitabine. J Infect Dis. 2016;214(1):55–64. doi:10.1093/infdis/jiw077. This study found that tenofovir diphosphate concentrations were approximately ten-fold higher in colorectal tissue than in the lower female genital tract. Results indicate that a minimum adherence level of approximately 6–7 oral PrEP doses per week are required to protected female genital tissue from HIV.
• Chen BA, Panther L, Marzinke MA, Hendrix CW, Hoesley CJ, van der Straten A, et al. Phase 1 safety, pharmacokinetics, and pharmacodynamics of dapivirine and maraviroc vaginal rings: a double-blind randomized trial. J Acquir Immune Defic Syndr. 2015;70(3):242–9. doi:10.1097/QAI.0000000000000702. This article presents findings from a multisite, double-blind, randomized, placebo-controlled trial of dapivirine and maraviroc containing vaginal rings for HIV prevention. Dapivirine concentrations in cervicovaginal fluid and tissue dropped rapidly after ring removal.
Wang L, Koppolu S, Chappell C, Moncla BJ, Hillier SL, Mahal LK. Studying the effects of reproductive hormones and bacterial vaginosis on the glycome of lavage samples from the cervicovaginal cavity. PLoS One. 2015;10(5):e0127021. doi:10.1371/journal.pone.0127021.
Ravel J, Gajer P, Fu L, Mauck CK, Koenig SSK, Sakamoto J, et al. Twice-daily application of HIV microbicides alter the vaginal microbiota. MBio. 2012;3(6):e00370–12. doi:10.1128/mBio.00370-12.
Spence P, Bhatia Garg A, Woodsong C, Devin B, Rosenberg Z. Recent work on vaginal rings containing antiviral agents for HIV prevention. Curr Opin HIV AIDS. 2015;10(4):264–70. doi:10.1097/COH.0000000000000157.
Boffito M, Jackson A, Owen A, Becker S. New approaches to antiretroviral drug delivery: challenges and opportunities associated with the use of long-acting injectable agents. Drugs. 2014;74(1):7–13. doi:10.1007/s40265-013-0163-7.
Geary CW, Bukusi EA. Women and ARV-based HIV prevention—challenges and opportunities. J Int AIDS Soc. 2014;17(3 Suppl 2):19356. doi:10.7448/IAS.17.3.19356.
Acknowledgments
We are grateful for the dedication of the thousands of women who have participated in PrEP clinical trials and open-label demonstration projects around the world.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Key Points
• 1% TFV gel with an on-demand dosing schedule is not efficacious in women with non-Lactobacillus dominant vaginal microbiomes but has efficacy estimated at 61% (95% CI 11–84%) in women with Lactobacillius dominant microbiota.
• Efficacy of oral PrEP is not modulated by bacterial vaginosis.
• The modulation of PrEP efficacy by vaginal dysbiosis may be specific to PrEP drug formulation and delivery mechanism.
• In settings with high rates of bacterial vaginosis/vaginal dysbiosis and high HIV burden, efficacy trials of novel PrEP products are well positioned to consider the interaction of vaginal dysbiosis with product efficacy.
This article is part of the Topical Collection on The Science of Prevention
Rights and permissions
About this article
Cite this article
Velloza, J., Heffron, R. The Vaginal Microbiome and its Potential to Impact Efficacy of HIV Pre-exposure Prophylaxis for Women. Curr HIV/AIDS Rep 14, 153–160 (2017). https://doi.org/10.1007/s11904-017-0362-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-017-0362-z