Abstract
Purpose of Review
High consumption of alcohol can lead to cirrhosis. The risk of a low to moderate consumption of alcohol in the setting of a concurrent liver disease is less clear. The aim of this review is to sum the evidence on the risk of adverse outcomes in patients with liver diseases other than alcoholic liver disease who consume alcohol.
Recent Findings
High alcohol consumption is strongly associated with adverse outcomes in most liver diseases. For hepatitis C, some evidence points to an increased risk for fibrosis progression also with low amounts. For non-alcoholic fatty liver disease, most studies indicate an inverse association between fibrosis and alcohol consumption, but methodological limitations reduce inference.
Summary
High alcohol consumption is associated with an increased risk of fibrosis progression and other adverse outcomes, while less is clear regarding low to moderate consumption. Obtaining high-level evidence on this topic ought to be the objective of future studies. Currently, an individual risk profile should be obtained in patients with liver disease who consume alcohol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol consumption is deeply embedded in most human societies, with some evidence suggesting that production of alcohol started as early as 10,000 BC [1, 2]. As an extremely available stimulant, the consumption of alcohol is vast, with 86% of US citizens reporting any lifetime alcohol consumption [3], and a mean consumption of 8.6 l of pure alcohol per year in the USA, compared to 6.2 l per year globally [4]. Alcohol has been reported to account for 85,000 deaths per year in the USA [5], and as much as 5.9% of all global deaths can be attributed to alcohol [4].
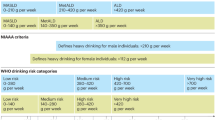
It has long been known that alcohol has detrimental effects on the liver by inducing alcoholic liver disease (ALD) [6], and alcohol accounts for up to 50% of all deaths in liver cirrhosis on a global scale [4]. However, although 90% of persons who consume more than 60 g of alcohol per day, roughly equivalent to six drinks, develop steatosis [7], significant fibrosis or cirrhosis only develops in up to 30% of this population [8,9,10]. In contrast, a low to moderate consumption of alcohol, below two drinks per day in women and three drinks per day in men, has not been associated with an increased risk for liver disease and is currently considered safe in most countries [11, 12], although a more restrictive approach is currently advocated in some countries, including the UK where the recommended maximum intake for men is now two drinks per day [12].
The role of low to moderate consumption in the setting of a concurrent liver disease is controversial, as an interactive effect could be present. This review briefly sums the epidemiological evidence for the risk of alcohol consumption in patients with liver diseases other than alcoholic liver disease.
NAFLD
Non-alcoholic fatty liver disease (NAFLD) is strongly associated with obesity, insulin resistance, and the metabolic syndrome [13,14,15]. Tracing the global obesity pandemic, NAFLD is now the most common liver disease, affecting up to 25% of the global population [16•] and is expected to become the leading indication for need of liver transplantation in the USA in the near future [17, 18]. Epidemiological studies have suggested an interactive effect between at least high-grade consumption of alcohol and obesity. In a study of almost 10,000 British men followed for 29 years, an increased risk for death in liver disease was found for consumption of more than 15 drinks of alcohol per week across all BMI categories. However, this risk was accentuated in obese men (RR 18.9, 95% CI 6.84–52.4) compared to normal weight men (RR 3.16, 95%CI 1.28–7.80) [19]. Similar findings have been found for women in the Million Women Study [20], where women who consumed more than 150 g of alcohol per week had a higher risk for development of liver cirrhosis if they also were obese than if they had a normal BMI.
In contrast, in patients with known NAFLD and compared to abstainers, a low to moderate consumption of alcohol has been associated with lower values of ALT [21], lower prevalence of hepatic steatosis [22, 23•, 24, 25], non-alcoholic steatohepatitis (NASH) [26], carotid plaques [27], and lower stages of fibrosis [26, 28•]. This is of importance since the most significant predicting factor for mortality in NAFLD is the stage of fibrosis [29, 30]. Contrasting this, a recent Mendelian randomization study found that NAFLD patients with a mutation in the aldehyde dehydrogenase gene, which leads to a slower metabolism of ethanol and therefore making persons with the mutation less likely to consume alcohol due to more side effects, did not have higher stages of fibrosis or prevalence of NASH [31••].
Heavy episodic drinking has been shown to increase the risk of fibrosis progression in biopsy-proven NAFLD [32], although this study did not evaluate lifetime consumption. There have been no randomized controlled trials of alcohol consumption in patients with NAFLD. However, a RCT of moderate red wine consumption in healthy students found that consumption of 33 g per day in men and 16 g per day in women for 3 months did not induce MRI-measured steatosis in single subject, indicating that to develop steatosis, either a higher dose or a longer duration of alcohol consumption is needed to induce steatosis [33••].
Notably, the main cause of death in NAFLD is cardiovascular disease [29]. Epidemiological studies indicate a J-shaped association between the amount of alcohol consumed and the risk of cardiovascular disease [34, 35], indicating that a low to moderate consumption of alcohol might actually be beneficial in NAFLD. A more extensive review on the effect of low to moderate alcohol consumption on NAFLD was recently published for the interested reader [36•].
Hepatitis C
Chronic viral hepatitis C (HCV) is highly prevalent, with data indicating that between 2.7 and 5.2 million persons are infected in the USA [37,38,39] and approximately 130 million cases globally [40]. HCV-related disease, including cirrhosis and hepatocellular carcinoma, accounts for around 700,000 deaths each year [41]. Alcohol consumption is high in many patients with HCV, especially those infected through intravenous drug use [42, 43]. A large sum of evidence points toward an interactive effect on the risk for fibrosis progression and development of cirrhosis in patients with HCV and a high consumption of alcohol of at least 30 g per day [44,45,46,47]. The role of low to moderate alcohol consumption in HCV is less clear. A French cross-sectional study of 260 HCV patients found no increased risk of fibrosis progression in subjects consuming below 30 g per day [48]. By contrast, in a group of 78 untreated patients with HCV that underwent paired liver biopsies with a median time of 6.3 years between biopsies, higher alcohol consumption and higher drinking frequency was independently associated with fibrosis progression. All these patients drank below 40 g of alcohol per day (median 4.8 g per day), suggesting that even a low consumption of alcohol is harmful in HCV [49].
Hepatitis B
As for HCV, a high consumption of alcohol corresponding to more than 30 g/day is associated with adverse outcomes, including an increased risk for mortality [50] and development of hepatocellular carcinoma [51, 52]. Regarding low to moderate alcohol consumption, less is clear. In a study of 1045 Chinese patients with hepatitis B investigated with transient elastography, patients who reported consumption of 1–20 g of alcohol per day did not have advanced fibrosis to a higher extent than patients who reported being abstainers [53]. As in many other studies, these are cross-sectional data which is prone to potential misclassification bias due to under-reporting of alcohol consumption in heavy drinkers or recall bias and should be interpreted cautiously.
Autoimmune Liver Diseases
This group of liver diseases includes autoimmune hepatitis (AIH), primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC). As these are rare conditions, not much evidence regarding alcohol consumption is available, and results from studies in this area should be interpreted cautiously. In AIH, an inverse association between alcohol consumption and the diagnosis of AIH was seen in a dose-response pattern in a smaller study of 72 AIH patients [54]. For PBC, a case-control study of more than 2,500 PBC patients in the UK found that alcohol use, defined as if a person had ever consumed alcohol regularly, was negatively associated with the presence of PBC [55]. An association between any alcohol consumption and HCC was found in a smaller case-control study of 52 Chinese PBC patients with HCC, where alcohol consumption was more common in HCC cases (31%) than in controls (8%, p = .01) [56]. In a larger European study, however, no association was found between alcohol consumption over 40 g per day and HCC in 716 PBC patients [57].
In PSC, alcohol consumption has been suggested to increase the risk of development of cholangiocarcinoma (CCA) [58]. However, this study included only four PSC patients with CCA and current alcohol consumption, why the dose-response effect is unclear. In a study of 96 Swedish PSC patients, lifetime alcohol consumption was low at 2.6 units of alcohol per week in mean. No association between alcohol consumption and higher values on transient elastography was found [59]. No cases of CCA were included in this cross-sectional study.
Hemochromatosis
Hereditary hemochromatosis (HH) is a genetic disorder of iron metabolism leading to inappropriate iron absorption and iron loading in various organs, especially the liver, and can lead to fibrosis progression and cirrhosis. In a study of 224 HH patients, 61% of subjects who consumed more than 60 g of alcohol per day had severe fibrosis or cirrhosis, compared to 7% of subjects who consumed less than 60 g per day [60]. Similar findings have been found in other studies [61,62,63]. The role of low to moderate alcohol consumption as a risk factor for fibrosis progression in HH remains to be studied.
Liver Transplantation
ALD is one of the leading indications for liver transplantation (LTX), and cases listed for LTX due to ALD have increased by 45% between 2004 and 2013 in the USA [17]. Although no formal recommendation on alcohol consumption exist for non-ALD cases either from AASLD or EASL after LTX, [64, 65] a careful approach is often advocated. Indeed, around 60% of non-ALD cases continue to consume alcohol after LTX, although often in small amounts [66]. Excessive drinking after LTX, independent of the primary indication, is associated with increased mortality [67] and graft loss [68].
Methodological Considerations
Several difficulties exist when trying to investigate the risk of alcohol consumption on disease progression or severity in concomitant liver disease. First, most studies investigating alcohol consumption have done so by using methodological designs including patients with manifest liver disease, including cirrhosis or HCC. This could induce misclassification bias of persons who has had a high lifetime consumption of alcohol but are currently abstaining due to symptoms, so-called “sick quitters” [69].
Also, patients under evaluation for any liver disease might be reluctant to disclose their true alcohol habits, or might unknowingly under-report these, leading to misclassification or recall bias. Indeed, in a recent study of 120 NAFLD patients who all reported drinking less than 14 units of alcohol per week, 11% of the sample had high levels of phosphatidyl ethanol (PEth) [28•], a validated marker for recent alcohol consumption [70,71,72], suggesting a higher than reported consumption of alcohol. This indicates that some patients with NAFLD could actually be classified as ALD patients. The use of validated biomarkers such as PEth could be one way to differentiate between NAFLD and ALD.
Second, different confounding factors could possibly explain the association between both detrimental and beneficial effects of alcohol and severity of liver disease. These include among others physical activity, smoking, dietary factors such as coffee and antioxidants, drinking patterns, and type of alcohol consumed, why such factors should ideally be accounted for in future studies.
Finally, genetic differences including mutations in the PNPLA3 [73, 74] and TM6SF2 genes [75, 76] are associated with increased risk of adverse outcomes in ALD and could influence the risk of disease progression that alcohol consumption might assert on any concurrent liver disease.
Conclusions
In summary, alcohol consumption of more than 30 g per day in men and 20 g per day in women is associated with fibrosis progression, development of cirrhosis and hepatocellular carcinoma, and mortality in most liver diseases. Large, well-designed studies on the risk, or benefit, of low to moderate alcohol consumption in the setting of concurrent liver disease are missing but are eagerly awaited. An individual approach should be made by clinicians advising patients with known or suspected liver diseases.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
McGovern PE. Uncorking the past: the quest for wine, beer, and other alcoholic beverages. Berkeley. 2009.
Patrick CH. Alcohol, culture and society. AMS Press. 1952.
Center for Behavioral Health Statistics and Quality. Behavioral Health Trends in the United States: results from the 2014 National Survey on Drug Use and Health. 2015.
World Health Organization. Global status report on alcohol and health – 2014 ed. 2014 [Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–45.
Lieber CS, Jones DP, Decarli LM. Effects of prolonged ethanol intake: production of fatty liver despite adequate diets. J Clin Invest. 1965;44:1009–21.
O'Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Am J Gastroenterol. 2010;105(1):14–32. quiz 3
Sorensen TI, Orholm M, Bentsen KD, Hoybye G, Eghoje K, Christoffersen P. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet. 1984;2(8397):241–4.
Leevy CM. Fatty liver: a study of 270 patients with biopsy proven fatty liver and review of the literature. Medicine. 1962;41:249–76.
Teli MR, Day CP, Burt AD, Bennett MK, James OF. Determinants of progression to cirrhosis or fibrosis in pure alcoholic fatty liver. Lancet. 1995;346(8981):987–90.
Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. Gut. 1997;41(6):845–50.
Drinking guidelines for the general population [Available from: http://www.iard.org/policy-tables/drinking-guidelines-general-population/.
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313(22):2263–73.
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10(11):686–90.
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917–23.
• Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. Important study on the global prevalence of NAFLD.
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547–55.
Goldberg D, Ditah IC, Saeian K, Lalehzari M, Aronsohn A, Gorospe EC, et al. Changes in the prevalence of hepatitis C virus infection, non-alcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017.
Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ. 2010;340:c1240.
Liu B, Balkwill A, Reeves G, Beral V, Million Women Study C. Body mass index and risk of liver cirrhosis in middle aged UK women: prospective study. Br Med J. 2010;340:7.
Dunn W, Xu R, Schwimmer JB. Modest wine drinking and decreased prevalence of suspected nonalcoholic fatty liver disease. Hepatology. 2008;47(6):1947–54.
Moriya A, Iwasaki Y, Ohguchi S, Kayashima E, Mitsumune T, Taniguchi H, et al. Alcohol consumption appears to protect against non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2011;33(3):378–88.
• Sookoian S, Castano GO, Pirola CJ. Modest alcohol consumption decreases the risk of non-alcoholic fatty liver disease: a meta-analysis of 43 175 individuals. Gut. 2014;63(3):530–2. Large meta-analysis of the impact of alcohol on presence of NAFLD.
Hashimoto Y, Hamaguchi M, Kojima T, Ohshima Y, Ohbora A, Kato T, et al. Modest alcohol consumption reduces the incidence of fatty liver in men: a population-based large-scale cohort study. J Gastroenterol Hepatol. 2015;30(3):546–52.
Moriya A, Iwasaki Y, Ohguchi S, Kayashima E, Mitsumune T, Ikeda F, et al. Roles of alcohol drinking pattern in fatty liver in Japanese women. Hepatol Int. 2013;7(3):859–68.
Dunn W, Sanyal AJ, Brunt EM, Unalp-Arida A, Donohue M, McCullough AJ, et al. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). J Hepatol. 2012;57(2):384–91.
Sinn DH, Gwak GY, Cho J, Son HJ, Paik YH, Choi MS, et al. Modest alcohol consumption and carotid plaques or carotid artery stenosis in men with non-alcoholic fatty liver disease. Atherosclerosis. 2014;234(2):270–5.
• Hagstrom H, Nasr P, Ekstedt M, Kechagias S, Onnerhag K, Nilsson E, et al. Low to moderate lifetime alcohol consumption is associated with less advanced stages of fibrosis in non-alcoholic fatty liver disease. Scand J Gastroenterol. 2016:1–7. First study to show that a biomarker might differ between NAFLD and ALD cases.
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61(5):1547–54.
Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, associates with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015.
•• Sookoian S, Flichman D, Castano GO, Pirola CJ. Mendelian randomisation suggests no beneficial effect of moderate alcohol consumption on the severity of nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2016;44(11–12):1224–34. Important study indicating that lifetime alcohol consumption might not be protective in NAFLD.
Ekstedt M, Franzen LE, Holmqvist M, Bendtsen P, Mathiesen UL, Bodemar G, et al. Alcohol consumption is associated with progression of hepatic fibrosis in non-alcoholic fatty liver disease. Scand J Gastroenterol. 2009;44(3):366–74.
•• Kechagias S, Zanjani S, Gjellan S, Leinhard OD, Kihlberg J, Smedby O, et al. Effects of moderate red wine consumption on liver fat and blood lipids: a prospective randomized study. Ann Med. 2011;43(7):545–54. Only RCT so far on the impact of low to moderate alcohol consumption on the risk of development of liver steatosis.
Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. N Engl J Med. 1997;337(24):1705–14.
Fuchs CS, Stampfer MJ, Colditz GA, Giovannucci EL, Manson JE, Kawachi I, et al. Alcohol consumption and mortality among women. N Engl J Med. 1995;332(19):1245–50.
• Ajmera VH, Terrault NA, Harrison SA. Is moderate alcohol use in non-alcoholic fatty liver disease good or bad? a critical review. Hepatology. 2017. More extensive review on alcohol consumption in NAFLD.
Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62(5):1353–63.
Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160(5):293–300.
Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C virus infection in USA: an estimate of true prevalence. Liver international : official journal of the International Association for the Study of the Liver. 2011;31(8):1090–101.
Alter MJ. Epidemiology of hepatitis C virus infection. World journal of gastroenterology : WJG. 2007;13(17):2436–41.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Rosman AS, Waraich A, Galvin K, Casiano J, Paronetto F, Lieber CS. Alcoholism is associated with hepatitis C but not hepatitis B in an urban population. Am J Gastroenterol. 1996;91(3):498–505.
Dalgard O, Jeansson S, Skaug K, Raknerud N, Bell H. Hepatitis C in the general adult population of Oslo: prevalence and clinical spectrum. Scand J Gastroenterol. 2003;38(8):864–70.
Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349(9055):825–32.
Innes HA, Hutchinson SJ, Barclay S, Cadzow E, Dillon JF, Fraser A, et al. Quantifying the fraction of cirrhosis attributable to alcohol among chronic hepatitis C virus patients: implications for treatment cost-effectiveness. Hepatology. 2013;57(2):451–60.
Delarocque-Astagneau E, Roudot-Thoraval F, Campese C, Desenclos JC. Past excessive alcohol consumption: a major determinant of severe liver disease among newly referred hepatitis C virus infected patients in hepatology reference centers, France, 2001. Ann Epidemiol. 2005;15(8):551–7.
Hutchinson SJ, Bird SM, Goldberg DJ. Influence of alcohol on the progression of hepatitis C virus infection: a meta-analysis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2005;3(11):1150–9.
Hezode C, Lonjon I, Roudot-Thoraval F, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of moderate alcohol consumption on histological activity and fibrosis in patients with chronic hepatitis C, and specific influence of steatosis: a prospective study. Aliment Pharmacol Ther. 2003;17(8):1031–7.
Westin J, Lagging LM, Spak F, Aires N, Svensson E, Lindh M, et al. Moderate alcohol intake increases fibrosis progression in untreated patients with hepatitis C virus infection. J Viral Hepat. 2002;9(3):235–41.
Marcellin P, Pequignot F, Delarocque-Astagneau E, Zarski JP, Ganne N, Hillon P, et al. Mortality related to chronic hepatitis B and chronic hepatitis C in France: evidence for the role of HIV coinfection and alcohol consumption. J Hepatol. 2008;48(2):200–7.
Jee SH, Ohrr H, Sull JW, Samet JM. Cigarette smoking, alcohol drinking, hepatitis B, and risk for hepatocellular carcinoma in Korea. J Natl Cancer Inst. 2004;96(24):1851–6.
Lin CW, Lin CC, Mo LR, Chang CY, Perng DS, Hsu CC, et al. Heavy alcohol consumption increases the incidence of hepatocellular carcinoma in hepatitis B virus-related cirrhosis. J Hepatol. 2013;58(4):730–5.
Ong A, Wong VW, Wong GL, Chan HL. The effect of caffeine and alcohol consumption on liver fibrosis—a study of 1045 Asian hepatitis B patients using transient elastography. Liver international : official journal of the International Association for the Study of the Liver. 2011;31(7):1047–53.
Ngu JH, Gearry RB, Frampton CM, Stedman CA. Autoimmune hepatitis: the role of environmental risk factors: a population-based study. Hepatol Int. 2013;7(3):869–75.
Prince MI, Ducker SJ, James OF. Case-control studies of risk factors for primary biliary cirrhosis in two United Kingdom populations. Gut. 2010;59(4):508–12.
Zhang XX, Wang LF, Jin L, Li YY, Hao SL, Shi YC, et al. Primary biliary cirrhosis-associated hepatocellular carcinoma in Chinese patients: incidence and risk factors. World journal of gastroenterology : WJG. 2015;21(12):3554–63.
Cavazza A, Caballeria L, Floreani A, Farinati F, Bruguera M, Caroli D, et al. Incidence, risk factors, and survival of hepatocellular carcinoma in primary biliary cirrhosis: comparative analysis from two centers. Hepatology. 2009;50(4):1162–8.
Chalasani N, Baluyut A, Ismail A, Zaman A, Sood G, Ghalib R, et al. Cholangiocarcinoma in patients with primary sclerosing cholangitis: a multicenter case-control study. Hepatology. 2000;31(1):7–11.
Hagstrom H, Stal P, Stokkeland K, Bergquist A. Alcohol consumption in patients with primary sclerosing cholangitis. World journal of gastroenterology : WJG. 2012;18(24):3105–11.
Fletcher LM, Dixon JL, Purdie DM, Powell LW, Crawford DH. Excess alcohol greatly increases the prevalence of cirrhosis in hereditary hemochromatosis. Gastroenterology. 2002;122(2):281–9.
Loreal O, Deugnier Y, Moirand R, Lauvin L, Guyader D, Jouanolle H, et al. Liver fibrosis in genetic hemochromatosis. Respective roles of iron and non-iron-related factors in 127 homozygous patients. J Hepatol. 1992;16(1–2):122–7.
Poynard T, Mathurin P, Lai CL, Guyader D, Poupon R, Tainturier MH, et al. A comparison of fibrosis progression in chronic liver diseases. J Hepatol. 2003;38(3):257–65.
Scotet V, Merour MC, Mercier AY, Chanu B, Le Faou T, Raguenes O, et al. Hereditary hemochromatosis: effect of excessive alcohol consumption on disease expression in patients homozygous for the C282Y mutation. Am J Epidemiol. 2003;158(2):129–34.
EASL Clinical Practice Guidelines. Liver transplantation. J Hepatol. 2016;64(2):433–85.
Lucey MR, Terrault N, Ojo L, Hay JE, Neuberger J, Blumberg E, et al. Long-term management of the successful adult liver transplant: 2012 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2013;19(1):3–26.
Tang H, Boulton R, Gunson B, Hubscher S, Neuberger J. Patterns of alcohol consumption after liver transplantation. Gut. 1998;43(1):140–5.
Faure S, Herrero A, Jung B, Duny Y, Daures JP, Mura T, et al. Excessive alcohol consumption after liver transplantation impacts on long-term survival, whatever the primary indication. J Hepatol. 2012;57(2):306–12.
Rice JP, Eickhoff J, Agni R, Ghufran A, Brahmbhatt R, Lucey MR. Abusive drinking after liver transplantation is associated with allograft loss and advanced allograft fibrosis. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2013;19(12):1377–86.
Hayashi PH, Harrison SA, Torgerson S, Perez TA, Nochajski T, Russell M. Cognitive lifetime drinking history in nonalcoholic fatty liver disease: some cases may be alcohol related. Am J Gastroenterol. 2004;99(1):76–81.
Aradottir S, Asanovska G, Gjerss S, Hansson P, Alling C. PHosphatidylethanol (PEth) concentrations in blood are correlated to reported alcohol intake in alcohol-dependent patients. Alcohol and alcoholism (Oxford, Oxfordshire). 2006;41(4):431–7.
Kechagias S, Dernroth DN, Blomgren A, Hansson T, Isaksson A, Walther L, et al. Phosphatidylethanol compared with other blood tests as a biomarker of moderate alcohol consumption in healthy volunteers: a prospective randomized study. Alcohol and alcoholism (Oxford, Oxfordshire). 2015;50(4):399–406.
Helander A, Peter O, Zheng YF. Monitoring of the alcohol biomarkers PEth, CDT and EtG/EtS in an outpatient treatment setting. Alcohol Alcohol. 2012;47(5):552–7.
Stickel F, Buch S, Lau K, Schwabedissen HMZ, Berg T, Ridinger M, et al. Genetic variation in the PNPLA3 gene is associated with alcoholic liver injury in Caucasians. Hepatology. 2011;53(1):86–95.
Tian C, Stokowski RP, Kershenobich D, Ballinger DG, Hinds DA. Variant in PNPLA3 is associated with alcoholic liver disease. Nat Genet. 2010;42(1):21–3.
Falleti E, Cussigh A, Cmet S, Fabris C, Toniutto P. PNPLA3 rs738409 and TM6SF2 rs58542926 variants increase the risk of hepatocellular carcinoma in alcoholic cirrhosis. Dig Liver Dis. 2016;48(1):69–75.
Buch S, Stickel F, Trepo E, Way M, Herrmann A, Nischalke HD, et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat Genet. 2015;47(12):1443–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hannes Hagström declares no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Management of the Cirrhotic Patient
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hagström, H. Alcohol Consumption in Concomitant Liver Disease: How Much is Too Much?. Curr Hepatology Rep 16, 152–157 (2017). https://doi.org/10.1007/s11901-017-0343-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-017-0343-0