Opinion statement
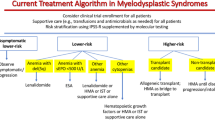
Chronic myelomonocytic leukemia (CMML) is an aggressive myeloid neoplasm in which treatment strategies with the capacity to improve survival are currently lacking. Clinical features are heterogeneous and although the overall prognosis is poor, survival can vary significantly between individuals. This reflects the need for an individualized treatment approach which incorporates accurate risk stratification. Though numerous prognostic scores exist, newer CMML-specific models incorporating molecular data should be favored. While asymptomatic, low-risk patients should be observed until their disease progresses, the majority of patients will require treatment. Due to a deficiency in treatments with disease-modifying capacity, any patient who requires treatment should be considered for enrollment in clinical trials evaluating novel therapeutic approaches. Allogeneic stem cell transplant (allo-SCT) remains the only current therapy with the potential to cure the disease and should be considered in most patients with intermediate- to high-risk disease. However, substantial risks are involved and, in part, because of advanced age at diagnosis, a minority of patients are candidates. Hypomethylating agents (HMAs) have become a preferred treatment approach, and should be used in those with cytopenias. Patients presenting with proliferative features can be treated with hydroxyurea to manage their symptoms and control leukocytosis, though HMAs can be incorporated as well, particularly in patients with higher risk disease. HMAs should also be considered in patients with a high burden of disease prior to proceeding with allo-SCT. Induction chemotherapy should be reserved for younger, healthy patients who have transformed to acute myeloid leukemia to induce remission prior to transplant. Supportive care utilizing transfusion support, erythropoiesis-stimulating agents, and infection prevention measures should be incorporated into the care of all patients.


Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544. This is the most recent update to the WHO classification of myeloid malignancies, published in 2016, and contains the current criteria required to establish a diagnosis of CMML.
Smith GS. Chronic monocytic leukaemia. Br Med J. 1937;2(3991):1–26.2.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985;103(4):620–5.
Rollison DE, Howlader N, Smith MT, Strom SS, Merritt WD, Ries LA, et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001–2004, using data from the NAACCR and SEER programs. Blood. 2008;112(1):45–52. https://doi.org/10.1182/blood-2008-01-134858.
Wassie EA, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA, et al. Molecular and prognostic correlates of cytogenetic abnormalities in chronic myelomonocytic leukemia: a Mayo Clinic-French Consortium study. Am J Hematol. 2014;89(12):1111–5. https://doi.org/10.1002/ajh.23846.
Such E, Cervera J, Costa D, Sole F, Vallespi T, Luno E, et al. Cytogenetic risk stratification in chronic myelomonocytic leukemia. Haematologica. 2011;96(3):375–83. https://doi.org/10.3324/haematol.2010.030957.
Patnaik MM, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014;28(11):2206–12. https://doi.org/10.1038/leu.2014.125.
Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol. 2013;31(19):2428–36. https://doi.org/10.1200/JCO.2012.47.3314.
• Padron E, Garcia-Manero G, Patnaik MM, Itzykson R, Lasho T, Nazha A, et al. An international data set for CMML validates prognostic scoring systems and demonstrates a need for novel prognostication strategies. Blood Cancer J. 2015;5:e333. https://doi.org/10.1038/bcj.2015.53. Our group evaluated seven different prognostic scoring systems in a large cohort of 1800 patients and found that all systems were valid and comparable, though none of these included somatic mutations. This paper also validated the negative prognostic impact of ASXL1 mutation and, for the first time, identified an inferior OS associated with mutation in CBL.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. https://doi.org/10.1182/blood-2012-03-420489.
Germing U, Strupp C, Aivado M, Gattermann N. New prognostic parameters for chronic myelomonocytic leukemia. Blood. 2002;100(2):731–2; author reply 2–3.
Kantarjian H, O'Brien S, Ravandi F, Cortes J, Shan J, Bennett JM, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original International Prognostic Scoring System. Cancer. 2008;113(6):1351–61. https://doi.org/10.1002/cncr.23697.
Onida F, Kantarjian HM, Smith TL, Ball G, Keating MJ, Estey EH, et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood. 2002;99(3):840–9.
Patnaik MM, Padron E, LaBorde RR, Lasho TL, Finke CM, Hanson CA, et al. Mayo prognostic model for WHO-defined chronic myelomonocytic leukemia: ASXL1 and spliceosome component mutations and outcomes. Leukemia. 2013;27(7):1504–10. https://doi.org/10.1038/leu.2013.88.
Such E, Germing U, Malcovati L, Cervera J, Kuendgen A, Della Porta MG, et al. Development and validation of a prognostic scoring system for patients with chronic myelomonocytic leukemia. Blood. 2013;121(15):3005–15. https://doi.org/10.1182/blood-2012-08-452938.
• Elena C, Galli A, Such E, Meggendorfer M, Germing U, Rizzo E, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. 2016;128(10):1408–17. https://doi.org/10.1182/blood-2016-05-714030. The CPSS-Mol model is the most recently created prognostic model and the most comprehensive with regard to incorporation of genetic information. It utilizes a genetic score that includes cytogenetics as well as the mutation status of ASXL1, RUNX1, NRAS, and SETBP1.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–9. https://doi.org/10.1182/blood-2005-05-2004.
•• Symeonidis A, van Biezen A, de Wreede L, Piciocchi A, Finke J, Beelen D, et al. Achievement of complete remission predicts outcome of allogeneic haematopoietic stem cell transplantation in patients with chronic myelomonocytic leukaemia. A study of the Chronic Malignancies Working Party of the European Group for Blood and Marrow Transplantation. Br J Haematol. 2015;171(2):239–46. https://doi.org/10.1111/bjh.13576. Although there is no prospective data on allo-SCT in CMML, this is the largest retrospective series reported to date, with 513 patients included. Published by the European Group for Blood and Marrow Transplantation, 4-year OS and relapse-free survival of 33% and 27%, respectively, were observed.
Eissa H, Gooley TA, Sorror ML, Nguyen F, Scott BL, Doney K, et al. Allogeneic hematopoietic cell transplantation for chronic myelomonocytic leukemia: relapse-free survival is determined by karyotype and comorbidities. Biol Blood Marrow Transplant. 2011;17(6):908–15. https://doi.org/10.1016/j.bbmt.2010.09.018.
Koreth J, Pidala J, Perez WS, Deeg HJ, Garcia-Manero G, Malcovati L, et al. Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: an international collaborative decision analysis. J Clin Oncol. 2013;31(21):2662–70. https://doi.org/10.1200/JCO.2012.46.8652.
Taussig DC, Davies AJ, Cavenagh JD, Oakervee H, Syndercombe-Court D, Kelsey S, et al. Durable remissions of myelodysplastic syndrome and acute myeloid leukemia after reduced-intensity allografting. J Clin Oncol. 2003;21(16):3060–5. https://doi.org/10.1200/JCO.2003.02.057.
Martino R, Iacobelli S, Brand R, Jansen T, van Biezen A, Finke J, et al. Retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic hematopoietic stem cell transplantation using HLA-identical sibling donors in myelodysplastic syndromes. Blood. 2006;108(3):836–46. https://doi.org/10.1182/blood-2005-11-4503.
Parker JE, Shafi T, Pagliuca A, Mijovic A, Devereux S, Potter M, et al. Allogeneic stem cell transplantation in the myelodysplastic syndromes: interim results of outcome following reduced-intensity conditioning compared with standard preparative regimens. Br J Haematol. 2002;119(1):144–54.
Brierley CK, Steensma DP. Allogeneic stem cell transplantation in myelodysplastic syndromes: does pretransplant clonal burden matter? Curr Opin Hematol. 2016;23(2):167–74. https://doi.org/10.1097/MOH.0000000000000217.
Damaj G, Duhamel A, Robin M, Beguin Y, Michallet M, Mohty M, et al. Impact of azacitidine before allogeneic stem-cell transplantation for myelodysplastic syndromes: a study by the Societe Francaise de Greffe de Moelle et de Therapie-Cellulaire and the Groupe-Francophone des Myelodysplasies. J Clin Oncol. 2012;30(36):4533–40. https://doi.org/10.1200/JCO.2012.44.3499.
Field T, Perkins J, Huang Y, Kharfan-Dabaja MA, Alsina M, Ayala E, et al. 5-Azacitidine for myelodysplasia before allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2010;45(2):255–60. https://doi.org/10.1038/bmt.2009.134.
Cogle CR, Imanirad I, Wiggins LE, Hsu J, Brown R, Scornik JC, et al. Hypomethylating agent induction therapy followed by hematopoietic cell transplantation is feasible in patients with myelodysplastic syndromes. Clin Adv Hematol Oncol. 2010;8(1):40–6.
• Kongtim P, Popat U, Jimenez A, Gaballa S, El Fakih R, Rondon G, et al. Treatment with hypomethylating agents before allogeneic stem cell transplant improves progression-free survival for patients with chronic myelomonocytic leukemia. Biol Blood Marrow Transplant. 2016;22(1):47–53. https://doi.org/10.1016/j.bbmt.2015.08.031. Although most evidence in this area is extrapolated from MDS patients, this study evaluated therapies preceding allo-SCT in 83 patients with CMML. Treatment with a HMA and achievement of bone marrow blasts < 5% prior to transplant were associated with improved PFS.
Hollenbach PW, Nguyen AN, Brady H, Williams M, Ning Y, Richard N, et al. A comparison of azacitidine and decitabine activities in acute myeloid leukemia cell lines. PLoS One. 2010;5(2):e9001. https://doi.org/10.1371/journal.pone.0009001.
Christman JK. 5-Azacytidine and 5-aza-2′-deoxycytidine as inhibitors of DNA methylation: mechanistic studies and their implications for cancer therapy. Oncogene. 2002;21(35):5483–95. https://doi.org/10.1038/sj.onc.1205699.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the Cancer and Leukemia Group B. J Clin Oncol. 2002;20(10):2429–40. https://doi.org/10.1200/JCO.2002.04.117.
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794–803. https://doi.org/10.1002/cncr.21792.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32. https://doi.org/10.1016/S1470-2045(09)70003-8.
Aribi A, Borthakur G, Ravandi F, Shan J, Davisson J, Cortes J, et al. Activity of decitabine, a hypomethylating agent, in chronic myelomonocytic leukemia. Cancer. 2007;109(4):713–7. https://doi.org/10.1002/cncr.22457.
Wijermans PW, Ruter B, Baer MR, Slack JL, Saba HI, Lubbert M. Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML). Leuk Res. 2008;32(4):587–91. https://doi.org/10.1016/j.leukres.2007.08.004.
Braun T, Itzykson R, Renneville A, de Renzis B, Dreyfus F, Laribi K, et al. Molecular predictors of response to decitabine in advanced chronic myelomonocytic leukemia: a phase 2 trial. Blood. 2011;118(14):3824–31. https://doi.org/10.1182/blood-2011-05-352039.
Costa R, Abdulhaq H, Haq B, Shadduck RK, Latsko J, Zenati M, et al. Activity of azacitidine in chronic myelomonocytic leukemia. Cancer. 2011;117(12):2690–6. https://doi.org/10.1002/cncr.25759.
Thorpe M, Montalvao A, Pierdomenico F, Moita F, Almeida A. Treatment of chronic myelomonocytic leukemia with 5-azacitidine: a case series and literature review. Leuk Res. 2012;36(8):1071–3. https://doi.org/10.1016/j.leukres.2012.04.024.
Fianchi L, Criscuolo M, Breccia M, Maurillo L, Salvi F, Musto P, et al. High rate of remissions in chronic myelomonocytic leukemia treated with 5-azacytidine: results of an Italian retrospective study. Leuk Lymphoma. 2013;54(3):658–61. https://doi.org/10.3109/10428194.2012.719617.
Ades L, Sekeres MA, Wolfromm A, Teichman ML, Tiu RV, Itzykson R, et al. Predictive factors of response and survival among chronic myelomonocytic leukemia patients treated with azacitidine. Leuk Res. 2013;37(6):609–13. https://doi.org/10.1016/j.leukres.2013.01.004.
Wong E, Seymour JF, Kenealy M, Westerman D, Herbert K, Dickinson M. Treatment of chronic myelomonocytic leukemia with azacitidine. Leuk Lymphoma. 2013;54(4):878–80. https://doi.org/10.3109/10428194.2012.730615.
•• Santini V, Allione B, Zini G, Gioia D, Lunghi M, Poloni A, et al. A phase II, multicentre trial of decitabine in higher-risk chronic myelomonocytic leukemia. Leukemia. 2018;32(2):413–8. https://doi.org/10.1038/leu.2017.186. This is the most recently published phase 2 study evaluating HMA use in a CMML-specific population. Forty-three predominantly high-risk patients were treated with decitabine with an overall response rate of 47% and median OS of 17 months, with a significant improvement in OS observed in responders (31 months in those with CR). No somatic mutation was predictive of response.
Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011;25(7):1147–52. https://doi.org/10.1038/leu.2011.71.
Traina F, Visconte V, Elson P, Tabarroki A, Jankowska AM, Hasrouni E, et al. Impact of molecular mutations on treatment response to DNMT inhibitors in myelodysplasia and related neoplasms. Leukemia. 2014;28(1):78–87. https://doi.org/10.1038/leu.2013.269.
Bejar R, Lord A, Stevenson K, Bar-Natan M, Perez-Ladaga A, Zaneveld J, et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood. 2014;124(17):2705–12. https://doi.org/10.1182/blood-2014-06-582809.
• Alfonso A, Montalban-Bravo G, Takahashi K, Jabbour EJ, Kadia T, Ravandi F, et al. Natural history of chronic myelomonocytic leukemia treated with hypomethylating agents. Am J Hematol. 2017;92(7):599–606. https://doi.org/10.1002/ajh.24735. This is a large retrospective analysis of 151 CMML patients treated with HMA at a single institution. Several predictors of improved OS were observed, as was a higher rate of CR in those treated with decitabine compared to azacitidine (58.3% vs. 20.6%, p < 0.001). A dismal prognosis after HMA failure was identified, with median OS of 7 months after relapse.
Garcia-Manero G, Griffiths EA, Roboz GJ, Busque L, Wells RA, Odenike O, et al. A phase 2 dose-confirmation study of oral ASTX727, a combination of oral decitabine with a cytidine deaminase inhibitor (CDAi) cedazuridine (E7727), in subjects with myelodysplastic syndromes (MDS). Blood. 2017;130(Suppl 1):4274.
Savona MR, Kolibaba K, Conkling P, Kingsley EC, Becerra C, Morris JC, et al. Extended dosing with CC-486 (oral azacitidine) in patients with myeloid malignancies. Am J Hematol. 2018. https://doi.org/10.1002/ajh.25216.
Beran M, Estey E, O'Brien S, Cortes J, Koller CA, Giles FJ, et al. Topotecan and cytarabine is an active combination regimen in myelodysplastic syndromes and chronic myelomonocytic leukemia. J Clin Oncol. 1999;17(9):2819–30. https://doi.org/10.1200/JCO.1999.17.9.2819.
Wattel E, Guerci A, Hecquet B, Economopoulos T, Copplestone A, Mahe B, et al. A randomized trial of hydroxyurea versus VP16 in adult chronic myelomonocytic leukemia. Groupe Francais des Myelodysplasies and European CMML group. Blood. 1996;88(7):2480–7.
Tricot G, Boogaerts MA. The role of aggressive chemotherapy in the treatment of the myelodysplastic syndromes. Br J Haematol. 1986;63(3):477–83.
Kantarjian HM, O'Brien S, Huang X, Garcia-Manero G, Ravandi F, Cortes J, et al. Survival advantage with decitabine versus intensive chemotherapy in patients with higher risk myelodysplastic syndrome: comparison with historical experience. Cancer. 2007;109(6):1133–7. https://doi.org/10.1002/cncr.22508.
de Witte T, Suciu S, Verhoef G, Labar B, Archimbaud E, Aul C, et al. Intensive chemotherapy followed by allogeneic or autologous stem cell transplantation for patients with myelodysplastic syndromes (MDSs) and acute myeloid leukemia following MDS. Blood. 2001;98(8):2326–31.
Ross SD, Allen IE, Probst CA, Sercus B, Crean SM, Ranganathan G. Efficacy and safety of erythropoiesis-stimulating proteins in myelodysplastic syndrome: a systematic review and meta-analysis. Oncologist. 2007;12(10):1264–73. https://doi.org/10.1634/theoncologist.12-10-1264.
List AF, Baer MR, Steensma DP, Raza A, Esposito J, Martinez-Lopez N, et al. Deferasirox reduces serum ferritin and labile plasma iron in RBC transfusion-dependent patients with myelodysplastic syndrome. J Clin Oncol. 2012;30(17):2134–9. https://doi.org/10.1200/JCO.2010.34.1222.
Stone RM. How I treat patients with myelodysplastic syndromes. Blood. 2009;113(25):6296–303. https://doi.org/10.1182/blood-2008-09-038935.
Gattermann N. Overview of guidelines on iron chelation therapy in patients with myelodysplastic syndromes and transfusional iron overload. Int J Hematol. 2008;88(1):24–9. https://doi.org/10.1007/s12185-008-0118-z.
Garcia-Manero G, Gore SD, Kambhampati S, Scott B, Tefferi A, Cogle CR, et al. Efficacy and safety of extended dosing schedules of CC-486 (oral azacitidine) in patients with lower-risk myelodysplastic syndromes. Leukemia. 2016;30(4):889–96. https://doi.org/10.1038/leu.2015.265.
Garcia-Manero G, Savona MR, Gore SD, Scott BL, Cogle CR, Boyd T, et al. CC-486 (oral azacitidine) in patients with hematological malignancies who had received prior treatment with injectable hypomethylating agents (HMAs): results from phase 1/2 CC-486 studies. Blood. 2016;128(22):905.
Issa JJ, Roboz G, Rizzieri D, Jabbour E, Stock W, O'Connell C, et al. Safety and tolerability of guadecitabine (SGI-110) in patients with myelodysplastic syndrome and acute myeloid leukaemia: a multicentre, randomised, dose-escalation phase 1 study. Lancet Oncol. 2015;16(9):1099–110. https://doi.org/10.1016/S1470-2045(15)00038-8.
Montalban-Bravo G, Bose P, Alvarado Y, Daver NG, Ravandi F, Borthakur G, et al. Updated results from phase II study of guadecitabine for patients with higher risk myelodysplastic syndromes or chronic myelomonocytic leukemia. J Clin Oncol. 2017;35(15_suppl):7020. https://doi.org/10.1200/JCO.2017.35.15_suppl.7020.
Padron E, Painter JS, Kunigal S, Mailloux AW, McGraw K, McDaniel JM, et al. GM-CSF-dependent pSTAT5 sensitivity is a feature with therapeutic potential in chronic myelomonocytic leukemia. Blood. 2013;121(25):5068–77. https://doi.org/10.1182/blood-2012-10-460170.
• Padron E, Dezern A, Andrade-Campos M, Vaddi K, Scherle P, Zhang Q, et al. A multi-institution phase I trial of ruxolitinib in patients with chronic myelomonocytic leukemia (CMML). Clin Cancer Res. 2016;22(15):3746–54. https://doi.org/10.1158/1078-0432.CCR-15-2781. The results of a phase 1 study of ruxolitinib in CMML, which demonstrated safety and efficacy. Ruxolitinib was particularly successful at controlling splenomegaly and constitutional symptoms, suggesting an additional therapeutic option in patients presenting with such symptoms. Final combined phase 1/2 data will be reported soon.
Padron E, DeZern AE, Niyongere S, Ball MC, Balasis M, Ramadan H, et al. Promising results of a phase 1/2 clinical trial of ruxolitinib in patients with chronic myelomonocytic leukemia. Blood. 2017;130(Suppl 1):162.
Ma Y, Rix LR, Zhang Q, Balasis ME, Komrokji RS, Rix U, et al. Pacritinib (PAC) synergistically potentiates azacitidine (5AZA) cytotoxicity in chronic myelomonocytic leukemia (CMML). Blood. 2015;126(23):1658.
Buonamici S, Yoshimi A, Thomas M, Seiler M, Chan B, Caleb B, et al. H3B-8800, an orally bioavailable modulator of the SF3b complex, shows efficacy in spliceosome-mutant myeloid malignancies. Blood. 2016;128(22):966.
Seiler M, Yoshimi A, Darman R, Chan B, Keaney G, Thomas M, et al. H3B-8800, an orally available small-molecule splicing modulator, induces lethality in spliceosome-mutant cancers. Nat Med. 2018;24:497–504. https://doi.org/10.1038/nm.4493 https://www.nature.com/articles/nm.4493#supplementary-information,.
Borthakur G, Popplewell L, Boyiadzis M, Foran J, Platzbecker U, Vey N, et al. Activity of the oral mitogen-activated protein kinase kinase inhibitor trametinib in RAS-mutant relapsed or refractory myeloid malignancies. Cancer. 2016;122(12):1871–9. https://doi.org/10.1002/cncr.29986.
Patnaik MM, Sallman DA, Sekeres MA, Luger S, Bejar R, Hobbs GS, et al. Preliminary results from an open-label, phase 2 study of tipifarnib in chronic myelomonocytic leukemia (CMML). Blood. 2017;130(Suppl 1):2963.
Fenaux P, Raza A, Mufti GJ, Aul C, Germing U, Kantarjian H, et al. A multicenter phase 2 study of the farnesyltransferase inhibitor tipifarnib in intermediate- to high-risk myelodysplastic syndrome. Blood. 2007;109(10):4158–63. https://doi.org/10.1182/blood-2006-07-035725.
Patnaik MM, Gupta V, Gotlib JR, Carraway HE, Wadleigh M, Schiller GJ, et al. Results from ongoing phase 2 trial of SL-401 in patients with advanced, high-risk myeloproliferative neoplasms including chronic myelomonocytic leukemia. Blood. 2016;128(22):4245.
23rd Congress of the European Hematology Association Stockholm, Sweden, June 14–17, 2018. HemaSphere 2018;2(S1):1–1113. https://doi.org/10.1097/hs9.0000000000000060.
Yang H, Bueso-Ramos C, DiNardo C, Estecio MR, Davanlou M, Geng QR, et al. Expression of PD-L1, PD-L2, PD-1 and CTLA4 in myelodysplastic syndromes is enhanced by treatment with hypomethylating agents. Leukemia. 2014;28(6):1280–8. https://doi.org/10.1038/leu.2013.355.
Tang X, Yang L, Li Z, Nalin AP, Dai H, Xu T, et al. First-in-man clinical trial of CAR NK-92 cells: safety test of CD33-CAR NK-92 cells in patients with relapsed and refractory acute myeloid leukemia. Am J Cancer Res. 2018;8(6):1083–9.
Giagounidis A, Platzbecker U, Germing U, Götze K, Kiewe P, Mayer KT, et al. Luspatercept treatment leads to long term increases in hemoglobin and reductions in transfusion burden in patients with low or intermediate-1 risk myelodysplastic syndromes (MDS): preliminary results from the phase 2 PACE-MDS extension study. Blood. 2015;126(23):92.
Komrokji R, Garcia-Manero G, Ades L, Prebet T, Steensma DP, Jurcic JG, et al. Sotatercept with long-term extension for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes: a phase 2, dose-ranging trial. Lancet Haematol. 2018;5(2):e63–72. https://doi.org/10.1016/S2352-3026(18)30002-4.
Ramadan H, Duong VH, Al Ali N, Padron E, Zhang L, Lancet JE, et al. Eltrombopag use in patients with chronic myelomonocytic leukemia (CMML): a cautionary tale. Clin Lymphoma Myeloma Leuk. 2016;16(16 Suppl):S64–6. https://doi.org/10.1016/j.clml.2016.02.009.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Anthony M. Hunter declares that he has no conflict of interest.
Ling Zhang declares that she has no conflict of interest.
Eric Padron has received research funding from Kura Oncology, Incyte Corporation, and KaloBios Pharmaceuticals.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Hunter, A.M., Zhang, L. & Padron, E. Current Management and Recent Advances in the Treatment of Chronic Myelomonocytic Leukemia. Curr. Treat. Options in Oncol. 19, 67 (2018). https://doi.org/10.1007/s11864-018-0581-6
Published:
DOI: https://doi.org/10.1007/s11864-018-0581-6