Abstract
Background
Although continuous positive airway pressure (CPAP) therapy curtails most of the negative impacts of obstructive sleep apnea (OSA), its efficacy is limited by its low long-term adherence. Nasal obstruction contributes to OSA pathophysiology and necessitates high CPAP titration pressures which reduce CPAP compliance.
Aim
This study aims at elucidating the outcomes of surgical correction of nasal obstruction in patients intolerant to CPAP therapy.
Methods
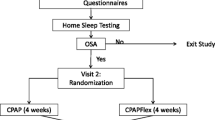
Forty-nine patients with severe OSA intolerant to CPAP secondary to surgically correctable nasal obstruction were operated upon. Patients were evaluated preoperatively and at least 3 months after the surgical intervention. Subjective assessment entailed the Nasal Obstruction Symptom Evaluation score (NOSE) and the Epworth Sleepiness Scale (ESS). Objectively the patients were assessed by acoustic rhinometry and standard polysomnography.
Results
Nasal surgical intervention resulted in an a statistically significant decrease in the mean NOSE score, ESS and optimal CPAP titration pressure. In addition, the minimal cross-sectional area (MCA1&2) increased significantly postoperatively. There was a positive correlation between the improvement in NOSE score as well as the MCA1& 2 and the postoperative decrease in CPAP titration pressure. Surgical correction of nasal obstruction improved CPAP outcomes and compliance in all patients.
Conclusions
Nasal surgery in OSA objectively assessed by acoustic rhinometry improved nasal obstruction with a resultant decrease in the CPAP pressure requirements. Given that lower CPAP pressures improve adherence to CPAP therapy, surgical alleviation of nasal obstruction should be considered a crucial intervention in the management armamentarium of OSA.
Similar content being viewed by others
References
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5(2):136–143. https://doi.org/10.1513/pats.200709-155MG
Léger D, Stepnowsky C (2020) The economic and societal burden of excessive daytime sleepiness in patients with obstructive sleep apnea. Sleep Med Rev 51:101275. https://doi.org/10.1016/j.smrv.2020.101275
Golbin JM, Somers VK, Caples SM (2008) Obstructive sleep apnea, cardiovascular disease, and pulmonary hypertension. https://doi.org/10.1513/pats.200708-143MG
Andrade RGS et al (2018) Nasal vs oronasal CPAP for OSA treatment: a meta-analysis. Chest 153(3):665–674. https://doi.org/10.1016/j.chest.2017.10.044
Grote L, Hedner J, Grunstein R, Kraiczi H (2000) Therapy with nCPAP: incomplete elimination of sleep related breathing disorder. Eur Respir J 16(5):921–927. https://doi.org/10.1183/09031936.00.16592100
Nakata S et al (2008) Effects of nasal surgery on sleep quality in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol 22(1):59–63. https://doi.org/10.2500/ajr.2008.22.3120
Inoue A, Chiba S, Matsuura K et al (2019) Nasal function and CPAP compliance. Auris Nasus Larynx 46(4):548–558. https://doi.org/10.1016/j.anl.2018.11.006
Smith PL, Wise RA, Gold AR et al (1988) Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol (Bethesda, Md. : 1985) 64(2):789–795. https://doi.org/10.1152/jappl.1988.64.2.789
Kimmelman CP (1989) The problem of nasal obstruction. Otolaryngol Clin North Am 22(2):253–264. Accessed: May 18, 2021. Available: http://www.ncbi.nlm.nih.gov/pubmed/2664651
Susarla SM, Thomas RJ, Abramson ZR, Kaban LB (2010) Biomechanics of the upper airway: changing concepts in the pathogenesis of obstructive sleep apnea. Int J Oral Maxillofac Surg 39(12):1149–1159. https://doi.org/10.1016/j.ijom.2010.09.007
Ishii L, Roxbury C, Godoy A et al (2015) Does nasal surgery improve OSA in patients with nasal obstruction and OSA? A meta-analysis. Otolaryngol Head Neck Surg Official J Am Acad Otolaryngol Head Neck Surg 153(3):326–333. https://doi.org/10.1177/0194599815594374
Verse T, Maurer JT, Pirsig W (2002) Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope 112(1):64–68. https://doi.org/10.1097/00005537-200201000-00012
Friedman M, Tanyeri H, Lim JW et al (2000) Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surgery Official J Am Acad Otolaryngol Head Neck Surg 122(1):71–74. https://doi.org/10.1016/S0194-5998(00)70147-1
Iwata N, Nakata S, Inada H et al (2020) Clinical indication of nasal surgery for the CPAP intolerance in obstructive sleep apnea with nasal obstruction. Auris Nasus Larynx 47(6):1018–1022. https://doi.org/10.1016/j.anl.2020.06.005
Kribbs NB et al (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 147(4):887–895. https://doi.org/10.1164/ajrccm/147.4.887
Stewart MG, Witsell DL, Smith TL et al (2007) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg Official J Am Acad Otolaryngol Head Neck Surg 130(2):157–163. https://doi.org/10.1016/j.otohns.2003.09.016
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545. https://doi.org/10.1093/sleep/14.6.540
Weaver TE et al (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30(6):711–719. https://doi.org/10.1093/sleep/30.6.711
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178. https://doi.org/10.1513/pats.200708-119MG
Krieger J (1992) Long-term compliance with nasal continuous positive airway pressure (CPAP) in obstructive sleep apnea patients and nonapneic snorers. Sleep 15(6 Suppl):S42–S46. https://doi.org/10.1093/sleep/15.suppl_6.s42
Bachour A, Maasilta P (2004) Mouth breathing compromises adherence to nasal continuous positive airway pressure therapy. Chest 126(4):1248–1254. https://doi.org/10.1378/chest.126.4.1248
Camacho M et al (2015) The effect of nasal surgery on continuous positive airway pressure device use and therapeutic treatment pressures: a systematic review and meta-analysis. Sleep 38(2):279–286. https://doi.org/10.5665/sleep.4414
Richards GN, Cistulli PA, Ungar RG et al (1996) Mouth leak with nasal continuous positive airway pressure increases nasal airway resistance. Am J Respir Crit Care Med 154(1):182–186. https://doi.org/10.1164/ajrccm.154.1.8680678
Lebret M et al (2017) Factors contributing to unintentional leak during CPAP treatment: a systematic review. Chest 151(3):707–719. https://doi.org/10.1016/j.chest.2016.11.049
Sopkova Z, Dorkova Z, Tkacova R (2009) Predictors of compliance with continuous positive airway pressure treatment in patients with obstructive sleep apnea and metabolic syndrome. Wien Klin Wochenschr 121(11–12):398–404. https://doi.org/10.1007/s00508-009-1181-z
Balcerzak J, Niemczyk K, Arcimowicz M, Gotlib T (2007) The role of functional nasal surgery in the treatment of obstructive sleep apnea syndrome. Otolaryngol Pol Polish Otolaryngol 61(1):80–84. https://doi.org/10.1016/S0030-6657(07)70388-8
Zonato AI, Bittencourt LRA, Martinho FL et al (2006) Upper airway surgery: the effect on nasal continuous positive airway pressure titration on obstructive sleep apnea patients. European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 63(5):481–486. https://doi.org/10.1007/s00405-005-1018-y
Poirier J, George C, Rotenberg B (2014) The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope 124(1):317–319. https://doi.org/10.1002/lary.24131
Sufioğlu M et al (2012) The efficacy of nasal surgery in obstructive sleep apnea syndrome: a prospective clinical study. European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 269(2):487–494. https://doi.org/10.1007/s00405-011-1682-z
Nowak C, Bourgin P, Portier F et al (2003) Nasal obstruction and compliance to nasal positive airway pressure. Annales d’oto-laryngologie et de chirurgie cervico faciale : bulletin de la Societe d’oto-laryngologie des hopitaux de Paris 120(3):161–166. Accessed: 15 May 2021.. Available: http://www.ncbi.nlm.nih.gov/pubmed/12843985
Nakata S et al (2005) Nasal resistance for determinant factor of nasal surgery in CPAP failure patients with obstructive sleep apnea syndrome. Rhinology 43(4):296–299. Accessed: 15 May 2021. Available: http://www.ncbi.nlm.nih.gov/pubmed/16405275
Reilly EK et al (2021) Tolerance of continuous positive airway pressure after sinonasal surgery. Laryngoscope 131(3):E1013–E1018. https://doi.org/10.1002/lary.28968
Li H-Y et al (2005) Acoustic reflection for nasal airway measurement in patients with obstructive sleep apnea-hypopnea syndrome. Sleep 28(12):1554–1559. https://doi.org/10.1093/sleep/28.12.1554
Morris LG, Setlur J, Burschtin OE et al (2006) Acoustic rhinometry predicts tolerance of nasal continuous positive airway pressure: a pilot study. Am J Rhinol 20(2):133–137. https://doi.org/10.1177/194589240602000202
Bican A, Kahraman A, Bora I et al (2010) What is the efficacy of nasal surgery in patients with obstructive sleep apnea syndrome? J Craniofac Surg 21(6):1801–1806. https://doi.org/10.1097/SCS.0b013e3181f40551
Knappe SW, Sonnesen L (2020) The reliability and influence of body position on acoustic pharyngometry and rhinometry outcomes. J Oral Maxillofac Res 11(4). https://doi.org/10.5037/jomr.2020.11401
Hellgren J, Yee BJ, Dungan G, Grunstein RR (2009) Altered positional regulation of nasal patency in patients with obstructive sleep apnoea syndrome. European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 266(1):83–87. https://doi.org/10.1007/s00405-008-0701-1
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation and data collection were performed by Mahmoud Ibrahim. Data analysis was performed by Samy Elwany. The initial draft of the manuscript was written by Ahmed Yassin Bahgat and Remon Bazak. It was subsequently modified by Samy Elwany and Remon Bazak. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was performed in accordance with the Helsinki declaration and was approved by the Institutional Review Board.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent to publish the data in the study was obtained from participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elwany, S., Bahgat, A.Y., Ibrahim, M. et al. Surgical correction of nasal obstruction in obstructive sleep apnea improves CPAP outcomes and compliance. Ir J Med Sci 191, 2723–2728 (2022). https://doi.org/10.1007/s11845-021-02896-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02896-6