Abstract
Little research focuses on the association between immune thrombocytopenic purpura and human immunodeficiency virus infection in Taiwan. This study investigated whether immune thrombocytopenic purpura might be an early hematologic manifestation of undiagnosed human immunodeficiency virus infection in Taiwan. We conducted a retrospective population-based cohort study using data of individuals enrolled in Taiwan National Health Insurance Program. There were 5472 subjects aged 1–84 years with a new diagnosis of immune thrombocytopenic purpura as the purpura group since 1998–2010 and 21,887 sex-matched and age-matched, randomly selected subjects without immune thrombocytopenic purpura as the non-purpura group. The incidence of human immunodeficiency virus infection at the end of 2011 was measured in both groups. We used the multivariable Cox proportional hazards regression model to measure the hazard ratio and 95 % confidence interval (CI) for the association between immune thrombocytopenic purpura and human immunodeficiency virus infection. The overall incidence of human immunodeficiency virus infection was 6.47-fold higher in the purpura group than that in the non-purpura group (3.78 vs. 0.58 per 10,000 person-years, 95 % CI 5.83–7.18). After controlling for potential confounding factors, the adjusted HR of human immunodeficiency virus infection was 6.3 (95 % CI 2.58–15.4) for the purpura group, as compared with the non-purpura group. We conclude that individuals with immune thrombocytopenic purpura are 6.47-fold more likely to have human immunodeficiency virus infection than those without immune thrombocytopenic purpura. We suggest not all patients, but only those who have risk factors for human immunodeficiency virus infection should receive testing for undiagnosed human immunodeficiency virus infection when they develop immune thrombocytopenic purpura.
Similar content being viewed by others
Introduction
Immune (idiopathic) thrombocytopenic purpura is an immune-mediated condition characterized by a low platelet count in the circulating blood, which results from accelerated platelet destruction and insufficient platelet production, both mediated by auto-antibodies [1–3]. Different types of hemorrhage usually are the first manifestation clinically. The incidence rates of immune thrombocytopenic purpura were between 1.1 and 12.5 per 100,000 children/year in children [4, 5] and between 1.6 and 3.9 per 100,000 adult/year in adults [6, 7]. Although the etiology still remains unclear, current evidence has indicated that various infections could be related to immune idiopathic thrombocytopenic purpura, such as Helicobacter pylori [8–10], hepatitis C [9, 11, 12], and human immunodeficiency virus [9, 13–15].
The first case of human immunodeficiency virus infection was reported in Taiwan in 1984, and the total number of human immunodeficiency virus patients collected was 31,036 at the end of 2015, with male patients predominant (93.94 %) [16]. It has become a major public health concern in Taiwan. Some studies have shown that approximately 5–10 % of patients with human immunodeficiency virus infection may develop thrombocytopenia during the disease course, and immune thrombocytopenic purpura might be the early clinical feature of human immunodeficiency virus infection [17–19]. However, little epidemiological evidence is available on the association between immune thrombocytopenic purpura and human immunodeficiency virus infection in Taiwan. If immune thrombocytopenic purpura precedes undiagnosed human immunodeficiency virus infection, clinicians should examine human immunodeficiency virus status among those with risk factors for human immunodeficiency virus infection presenting with immune thrombocytopenic purpura. Therefore, we conducted a population-based cohort study to investigate whether there is an association between immune thrombocytopenic purpura and human immunodeficiency virus infection.
Methods
Study design
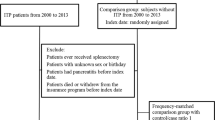
We conducted a retrospective population-based cohort study using the database of the Taiwan National Health Insurance Program. The program began in March 1995, which covered almost 99 % of the 23 million citizens living in Taiwan [20]. The program was well described in greater detail in previous studies [21–30]. The study was approved by the Institutional Review Board of China Medical University and Hospital in Taiwan (CMUH-104-REC2-115).
Study subjects, comorbidities and main outcome measurement
Subjects aged 1–84 years with a new diagnosis of immune thrombocytopenic purpura was selected as the purpura group since 1998–2010, based on the International Classification of Diseases 9th Revision (ICD-9 code 287). We defined the date of diagnosing immune thrombocytopenic purpura as the index date. We randomly selected subjects without a diagnosis of immune thrombocytopenic purpura from the same database as the non-purpura group. Both groups were matched with gender, age (every 5-year span), comorbidities, and index year of diagnosing immune thrombocytopenic purpura. Subjects with a diagnosis of human immunodeficiency virus infection (ICD-9 codes 795.71, V08, 042 and 079.53) at the baseline were excluded from the study.
Some risk factors of human immunodeficiency virus infection, such as history of injection drug use and multiple sexual partners, were not documented in this database. We used drug dependence instead of injection drug use, and venereal diseases instead of history of multiple sex partners. This limitation has been mentioned in previous studies [31]. Therefore, factors potentially related to human immunodeficiency virus infection were included as follows: drug dependence (ICD-9 code 304) and venereal diseases (ICD-9 codes 090–099). All study subjects were followed until human immunodeficiency virus infection was diagnosed or to the end of 2011.
Statistical analysis
The distributions of gender, age, and comorbidities were compared between the purpura group and non-purpura groups using the Chi-square test for categorized variables and t-test for continuous variables. The incidence of human immunodeficiency virus infection was measured as the number of human immunodeficiency virus infection events detected during the follow-up period, divided by the total follow-up person-years for each group. The multivariable Cox proportional hazards regression model was used to measure the hazard ratio (HR) and 95 % confidence interval (CI) for the association between human immunodeficiency virus infection, immune thrombocytopenic purpura, and other comorbidities. The statistical significance level was set at a two-sided probability value <0.05. All analyses were performed by SAS software version 9.2 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Baseline information of the study population
Table 1 demonstrates that there were 5472 subjects in the purpura group and 21,887 subjects in the non-purpura group. The purpura group and non-purpura groups had similar distributions of gender, age, and comorbidities (Chi-square test, P > 0.05 for all). The mean ages (standard deviation) of the study subjects were 49.7 ± 21.8 years for the purpura group and 49.3 ± 21.6 for the non-purpura group (t-test, P = 0.25).
Incidence of human immunodeficiency virus infection of the study population
At the end of follow-up, the overall incidence of human immunodeficiency virus infection was 6.47-fold higher in the purpura group than that in the non-purpura group (3.78 vs. 0.58 per 10,000 person-years, 95 % CI 5.83–7.18). In stratifications of gender, age, and follow-up period, the incidence rates of human immunodeficiency virus infection are all higher in the purpura group than those in the non-purpura group. Most subjects with a new diagnosis of human immunodeficiency virus infection in the purpura group were male subjects (75 %, 9/12). Male subjects had a higher incidence of human immunodeficiency virus infection than female subjects in both groups (6.65 vs. 1.65 per 10,000 person-years in the purpura group, and 0.99 vs. 0.26 per 10,000 person-years in the non-purpura group, respectively). The purpura group aged 20–39 had the highest incidence of human immunodeficiency virus infection (11.0 per 10,000 person-years). The analysis stratified by follow-up period demonstrates that the risk of human immunodeficiency virus infection lasted throughout the follow-up period, even after 12 months of diagnosing immune thrombocytopenic purpura (incidence rate ratio 1.45, 95 % CI 1.28–1.65). However, the risk seemed to be much higher during the first 6 months of follow-up period, with an incidence rate ratio of 32.4 (95 % CI 27.8–37.7) (Table 2).
Human immunodeficiency virus infection associated with immune thrombocytopenic purpura and other comorbidities
After controlling for potential confounding factors, the multivariable Cox proportional hazards regression analysis demonstrates that the adjusted HR of human immunodeficiency virus infection is 6.3 (95 % CI 2.58–15.4) for the purpura group, as compared with the non-purpura group. Male gender (adjusted HR 3.92, 95 % CI 1.42–10.8), drug dependence (adjusted HR 25.4, 95 % CI 3.36–191.3), and venereal diseases (adjusted HR 18.2, 95 % CI 2.36–140.5) are factors significantly associated with human immunodeficiency virus infection (Table 3).
Discussion
In this retrospective population-based cohort study, 12 events of human immunodeficiency virus infection were detected in the purpura group, who were aged 15–60 years. They belonged to adult-onset immune thrombocytopenic purpura. We found that the overall incidence of human immunodeficiency virus infection is 6.47-fold higher in the purpura group than that in the non-purpura group. We found that the risk of human immunodeficiency virus infection seemed to be much higher during the first 6 months of follow-up period (Table 2). After controlling for potential confounding factors, patients with immune thrombocytopenic purpura are associated with 6.3-fold increased hazard of human immunodeficiency virus infection (Table 3).
In this present study, patients with a diagnosis of human immunodeficiency virus infection at baseline were excluded from the study. Therefore, immune thrombocytopenic purpura developed before the serological detection of human immunodeficiency virus. That is, immune thrombocytopenic purpura might be an early hematologic manifestation of undiagnosed human immunodeficiency virus infection, which was compatible with previous studies [14, 19, 32]. We found that most patients with a new diagnosis of human immunodeficiency virus infection in the purpura group were male patients (75 %, 9/12). Among these nine male patients, four patients were aged 21–30, four patients were aged 31–40, and one patient was aged 41–50. This finding indicates younger male patients predominate. We estimated that the number needed to screen for human immunodeficiency virus infection was 39.3 among male patients aged 21–30 and 53 among male patients aged 31–40 in the present study. In clinical practice, not all patients with immune thrombocytopenic purpura would have human immunodeficiency virus infection. Not all patients with immune thrombocytopenic purpura need to be screened for human immunodeficiency virus infection. We suggest that only those with risk factors for human immunodeficiency virus infection, such as history of injection drug use or multiple sexual partners, should receive testing for undiagnosed human immunodeficiency virus infection when they present with immune thrombocytopenic purpura, particularly in younger male patients during the first 6 months of follow-up period. The thorough history focusing on injection drug use and sexual contact is without question the most valuable information to determine who needs to be tested for undiagnosed human immunodeficiency virus infection. Thus, the number needed to screen will be minimized.
The pathogenesis between immune thrombocytopenic purpura and human immunodeficiency virus infection cannot be illustrated in our observational study. We review the related literature and summarize as follows. First, there may be a direct effect of human immunodeficiency virus infection on megakaryocytes and platelets, which might lead to insufficient platelet production from the bone marrow and diminished survival time of platelet [33–36]. In addition, there may be the presence of cross-reactive antibodies between human immunodeficiency virus glycoprotein and platelet glycoprotein, which might accelerate platelet destruction in the circulating blood [15, 36–38]. Both potential mechanisms further shorten the life span of the platelet. Thus, thrombocytopenia would develop.
Some limitations of this present study should be discussed. First, the small number of human immunodeficiency virus infections found still remains a question (12 events in the purpura group and 8 events in the non-purpura group). Thus, the statistical power of the study is limited. Second, due to the inherent limitation of this database, we could not make sure that risk behaviors of human immunodeficiency virus infection were introduced before or after the development of immune thrombocytopenic purpura. Third, due to the same limitation, the diagnostic criteria for ITP were not recorded in this database. We cannot verify the diagnosis based on ICD-9 code. However, the quality of this database has been well discussed by Hsing et al. [39], we think the diagnostic accuracy of comorbidities included can be certain. Fourth, due to the same limitation, the variables included in the analyses are very limited and the interpretation of our findings should be cautious. Fifth, surveillance bias might have occurred in this study. Human immunodeficiency virus infection might have been acquired before the onset of immune thrombocytopenic purpura. Therefore, patients with immune thrombocytopenic purpura should more frequently, receive routine check-ups when searching for the etiology of immune thrombocytopenic purpura. Consequently, these patients were more likely to be tested for human immunodeficiency virus infection. Sixth, although the association with drug dependence or presence of venereal diseases was even stronger than immune thrombocytopenic purpura itself (Table 3), we just wish to alert clinicians that immune thrombocytopenic purpura might be an early hematologic manifestation of undiagnosed human immunodeficiency virus infection.
Some strength of this study deserves mentioned. This is the first epidemiological study focusing on the association between immune thrombocytopenic purpura and human immunodeficiency virus infection in Taiwan.
We conclude that individuals with immune thrombocytopenic purpura are 6.47-fold more likely to have human immunodeficiency virus infection than those without immune thrombocytopenic purpura. Immune thrombocytopenic purpura may be an early hematologic manifestation of undiagnosed human immunodeficiency virus infection in Taiwan. We suggest that not all patients, but only those who have risk factors for human immunodeficiency virus infection should receive testing for undiagnosed human immunodeficiency virus infection when they develop immune thrombocytopenic purpura, particularly younger male patients during the first 6 months of follow-up period.
References
Stasi R, Evangelista ML, Stipa E, Buccisano F, Venditti A, Amadori S (2008) Idiopathic thrombocytopenic purpura: current concepts in pathophysiology and management. Thromb Haemost 99:4–13
Palaniappan G, Jennings W (2009) Idiopathic thrombocytopenic purpura. Mo Med 106:69–73
Provan D (2009) Characteristics of immune thrombocytopenic purpura: a guide for clinical practice. Eur J Haematol Suppl 71:8–12
Watts RG (2004) Idiopathic thrombocytopenic purpura: a 10-year natural history study at the childrens hospital of alabama. Clin Pediatr 43:691–702
Zaki M, Hassanein AA, Khalil AF (1990) Childhood idiopathic thrombocytopenic purpura: report of 60 cases from Kuwait. J Trop Pediatr 36:10–13
Neylon AJ, Saunders PW, Howard MR, Proctor SJ, Taylor PR (2003) Clinically significant newly presenting autoimmune thrombocytopenic purpura in adults: a prospective study of a population-based cohort of 245 patients. Br J Haematol 122:966–974
Abrahamson PE, Hall SA, Feudjo-Tepie M, Mitrani-Gold FS, Logie J (2009) The incidence of idiopathic thrombocytopenic purpura among adults: a population-based study and literature review. Eur J Haematol 83:83–89
Fujimura K (2005) Helicobacter pylori infection and idiopathic thrombocytopenic purpura. Int J Hematol 81:113–118
Stasi R, Willis F, Shannon MS, Gordon-Smith EC (2009) Infectious causes of chronic immune thrombocytopenia. Hematol Oncol Clin N Am 23:1275–1297
Franchini M, Vescovi PP, Garofano M, Veneri D (2012) Helicobacter pylori-associated idiopathic thrombocytopenic purpura: a narrative review. Semin Thromb Hemost 38:463–468
Pockros PJ, Duchini A, McMillan R, Nyberg LM, McHutchison J, Viernes E (2002) Immune thrombocytopenic purpura in patients with chronic hepatitis C virus infection. Am J Gastroenterol 97:2040–2045
Nakajima H, Takagi H, Yamazaki Y, Toyoda M, Takezawa J, Nagamine T et al (2005) Immune thrombocytopenic purpura in patients with hepatitis C virus infection. Hepatogastroenterology 52:1197–1200
Karpatkin S, Nardi MA, Hymes KB (1988) Immunologic thrombocytopenic purpura after heterosexual transmission of human immunodeficiency virus (HIV). Ann Intern Med 109:190–193
Hollak CE, Kersten MJ, van der Lelie J, Lange JM (1990) Thrombocytopenic purpura as first manifestation of human immunodeficiency virus type I (HIV-1) infection. Neth J Med 37:63–68
Bettaieb A, Fromont P, Louache F, Oksenhendler E, Vainchenker W, Duedari N et al (1992) Presence of cross-reactive antibody between human immunodeficiency virus (HIV) and platelet glycoproteins in HIV-related immune thrombocytopenic purpura. Blood 80:162–169
Statistics of HIV/AIDS, Centers for Disease Control, Taiwan. http://www.cdc.gov.tw/english/index.aspx. Accessed 1 Apr 2016
Oksenhendler E, Seligmann M (1990) HIV-related thrombocytopenia. Immunodefic Rev 2:221–231
Rigaud M, Leibovitz E, Quee CS, Kaul A, Nardi M, Pollack H et al (1992) Thrombocytopenia in children infected with human immunodeficiency virus: long-term follow-up and therapeutic considerations. J Acquir Immune Defic Syndr 5:450–455
Shah I (2013) Immune thrombocytopenic purpura: a presentation of HIV infection. J Int Assoc Provid AIDS Care 12:95–97
National Health Insurance Research Database, Taiwan. http://nhird.nhri.org.tw/en/index.html. Accessed 1 Apr 2016 (English version)
Lai SW, Liao KF, Liao CC, Muo CH, Liu CS, Sung FC (2010) Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine (Baltimore) 89:295–299
Hung SC, Liao KF, Lai SW, Li CI, Chen WC (2011) Risk factors associated with symptomatic cholelithiasis in Taiwan: a population-based study. BMC Gastroenterol 11:11–111
Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC (2012) Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol 107:46–52
Chen HY, Lai SW, Muo CH, Chen PC, Wang IJ (2012) Ethambutol-induced optic neuropathy: a nationwide population-based study from Taiwan. Br J Ophthalmol 96:1368–1371
Cheng KC, Chen YL, Lai SW, Mou CH, Tsai PY, Sung FC (2012) Patients with chronic kidney disease are at an elevated risk of dementia: a population-based cohort study in Taiwan. BMC Nephrol 13:1471–2369
Cheng KC, Chen YL, Lai SW, Tsai PY, Sung FC (2012) Risk of esophagus cancer in diabetes mellitus: a population-based case-control study in Taiwan. BMC Gastroenterol 12:12–177
Chen YL, Cheng KC, Lai SW, Tsai IJ, Lin CC, Sung FC et al (2013) Diabetes and risk of subsequent gastric cancer: a population-based cohort study in Taiwan. Gastric Cancer 16:389–396
Kuo SC, Lai SW, Hung HC, Muo CH, Hung SC, Liu LL et al (2015) Association between comorbidities and dementia in diabetes mellitus patients: population-based retrospective cohort study. J Diabetes Complic 29:1071–1076
Lai HC, Lin CC, Cheng KS, Kao JT, Chou JW, Peng CY et al (2014) Increased incidence of gastrointestinal cancers among patients with pyogenic liver abscess: a population-based cohort study. Gastroenterology 146:129–137
Yang SP, Muo CH, Wang IK, Chang YJ, Lai SW, Lee CW et al (2015) Risk of type 2 diabetes mellitus in female breast cancer patients treated with morphine: a retrospective population-based time-dependent cohort study. Diabetes Res Clin Pract 110:285–290
Lai SW, Lin CL, Liao KF, Chen WC (2016) Herpes zoster could be an early manifestation of undiagnosed human immunodeficiency virus infection. J Formos Med Assoc 115:372–376
Elezovic I, Jevtovic D, Rolovic Z (1989) Immunologic thrombocytopenic purpura as a clinical manifestation of HIV infection. Srp Arh Celok Lek 117:499–506
Zucker-Franklin D, Cao YZ (1989) Megakaryocytes of human immunodeficiency virus-infected individuals express viral RNA. Proc Natl Acad Sci USA 86:5595–5599
Ballem PJ, Belzberg A, Devine DV, Lyster D, Spruston B, Chambers H et al (1992) Kinetic studies of the mechanism of thrombocytopenia in patients with human immunodeficiency virus infection. N Engl J Med 327:1779–1784
Cole JL, Marzec UM, Gunthel CJ, Karpatkin S, Worford L, Sundell IB et al (1998) Ineffective platelet production in thrombocytopenic human immunodeficiency virus-infected patients. Blood 91:3239–3246
Leissinger CA (2001) Platelet kinetics in immune thrombocytopenic purpura and human immunodeficiency virus thrombocytopenia. Curr Opin Hematol 8:299–305
Nardi MA, Liu LX, Karpatkin S (1997) GPIIIa-(49–66) is a major pathophysiologically relevant antigenic determinant for anti-platelet GPIIIa of HIV-1-related immunologic thrombocytopenia. Proc Natl Acad Sci USA 94:7589–7594
Chia WK, Blanchette V, Mody M, Wright JF, Freedman J (1998) Characterization of HIV-1-specific antibodies and HIV-1-crossreactive antibodies to platelets in HIV-1-infected haemophiliac patients. Br J Haematol 103:1014–1022
Hsing AW, Ioannidis JP (2015) Nationwide population science: lessons from the Taiwan National Health Insurance Research Database. JAMA Intern Med 175:1527–1529
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019). This funding agency did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Statements of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
None.
Additional information
S.-W. Lai and H.-F. Lin contributed equally to this study.
Rights and permissions
About this article
Cite this article
Lai, SW., Lin, HF., Lin, CL. et al. Immune thrombocytopenic purpura might be an early hematologic manifestation of undiagnosed human immunodeficiency virus infection. Intern Emerg Med 12, 157–162 (2017). https://doi.org/10.1007/s11739-016-1520-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1520-9