Abstract
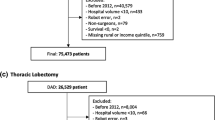
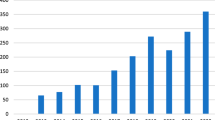
To evaluate trends in contemporary robotic surgery across multiple organ sites as they relate to robotic prostatectomy volume. We queried the National Cancer Database for patients who underwent surgery from 2010 to 2013 for prostate, kidney, bladder, corpus uteri, uterus, cervix, colon, sigmoid, rectum, lung and bronchus. The trend between volumes of robotic surgery for each organ site was analyzed using the Cochran–Armitage test. Multivariable models were then created to determine independent predictors of robotic surgery within each organ site by calculating the odds ratio with 95% CI. Among the 566,399 surgical cases analyzed, 35.1% were performed using robot assistance. Institutions whose robotic prostatectomy volume was in the top 75 percentile compared to the bottom 25 percentile performed a larger percentage of robotic surgery on the following sites: kidney 32.6 vs. 28.8%, bladder 23.6 vs. 18.6%, uterus 52.5 vs. 47.7%, cervix 43.5 vs. 39.2%, colon 3.2 vs. 2.9%, rectum 10.7 vs. 8.9%, and lung 7.3 vs. 6.8% (all p < 0.0001). It appears that increased trends toward robotic surgery in urology have lead to increased robotic utilization within other surgical fields. Future analysis in benign utilizations of robotic surgery as well as outcome data comparing robotic to open approaches are needed to better understand the ever-evolving nature of minimally invasive surgery within the United States.


Similar content being viewed by others
References
Barbash GI, Glied SA (2010) New technology and health care costs—the case of robot-assisted surgery. N Engl J Med 363:701–704. https://doi.org/10.1056/NEJMp1006602
Menon M, Tewari A, Peabody JO et al (2004) Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin North Am 31:701–717. https://doi.org/10.1016/j.ucl.2004.06.011
Beauval J-B, Roumiguié M, Ouali M et al (2015) A prospective trial comparing consecutive series of open retropubic and robot-assisted laparoscopic radical prostatectomy in a centre: Oncologic and functional outcomes. Prog En Urol J Assoc Fr Urol Société Fr Urol 25:370–378. https://doi.org/10.1016/j.purol.2015.03.007
Alemozaffar M, Sanda M, Yecies D et al (2015) Benchmarks for operative outcomes of robotic and open radical prostatectomy: results from the Health Professionals Follow-up Study. Eur Urol 67:432–438. https://doi.org/10.1016/j.eururo.2014.01.039
Haglind E, Carlsson S, Stranne J et al (2015) Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol 68:216–225. https://doi.org/10.1016/j.eururo.2015.02.029
Caras RJ, Lustik MB, Kern SQ et al (2014) Laparoscopic radical prostatectomy demonstrates less morbidity than open radical prostatectomy: an analysis of the American College of Surgeons-National Surgical Quality Improvement Program database with a focus on surgical trainee involvement. J Endourol Endourol Soc 28:298–305. https://doi.org/10.1089/end.2013.0475
Pearce SM, Pariser JJ, Karrison T et al (2016) Comparison of perioperative and early oncologic outcomes between open and robotic assisted laparoscopic prostatectomy in a contemporary population based cohort. J Urol. https://doi.org/10.1016/j.juro.2016.01.105
Lowrance WT, Eastham JA, Savage C et al (2012) Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol 187:2087–2092. https://doi.org/10.1016/j.juro.2012.01.061
Lowrance WT, Parekh DJ (2012) The rapid uptake of robotic prostatectomy and its collateral effects. Cancer 118:4–7. https://doi.org/10.1002/cncr.26275
Tapper A-M, Hannola M, Zeitlin R et al (2014) A systematic review and cost analysis of robot-assisted hysterectomy in malignant and benign conditions. Eur J Obstet Gynecol Reprod Biol 177:1–10. https://doi.org/10.1016/j.ejogrb.2014.03.010
Yafchak R (2000) A longitudinal study of economies of scale in the hospital industry. J Health Care Finance 27:67–89
Bilimoria KY, Stewart AK, Winchester DP, Ko CY (2008) The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 15:683–690. https://doi.org/10.1245/s10434-007-9747-3
Halabi WJ, Kang CY, Jafari MD et al (2013) Robotic-assisted colorectal surgery in the United States: a nationwide analysis of trends and outcomes. World J Surg 37:2782–2790. https://doi.org/10.1007/s00268-013-2024-7
Kent M, Wang T, Whyte R et al (2014) Open, video-assisted thoracic surgery, and robotic lobectomy: review of a national database. Ann Thorac Surg 97:236–242. https://doi.org/10.1016/j.athoracsur.2013.07.117
Conrad LB, Ramirez PT, Burke W et al (2015) Role of minimally invasive surgery in gynecologic oncology: an updated survey of members of the society of gynecologic oncology. Int Gynecol Cancer Soc 25:1121–1127. https://doi.org/10.1097/IGC.0000000000000450
Barkun JS, Aronson JK, Feldman LS et al (2009) Evaluation and stages of surgical innovations. Lancet Lond Engl 374:1089–1096. https://doi.org/10.1016/S0140-6736(09)61083-7
Kim J, ElRayes W, Wilson F et al (2015) Disparities in the receipt of robot-assisted radical prostatectomy: between-hospital and within-hospital analysis using 2009–2011 California inpatient data. BMJ Open 5:e007409. https://doi.org/10.1136/bmjopen-2014-007409
Kim SP, Boorjian SA, Shah ND et al (2013) Disparities in access to hospitals with robotic surgery for patients with prostate cancer undergoing radical prostatectomy. J Urol 189:514–520. https://doi.org/10.1016/j.juro.2012.09.033
Blake EA, Sheeder J, Behbakht K et al (2016) Factors impacting use of robotic surgery for treatment of endometrial cancer in the United States. Ann Surg Oncol. https://doi.org/10.1245/s10434-016-5252-x
Esselen KM, Vitonis A, Einarsson J et al (2015) Health care disparities in hysterectomy for gynecologic cancers: data from the 2012 national inpatient sample. Obstet Gynecol 126:1029–1039. https://doi.org/10.1097/AOG.0000000000001088
Robinson CN, Balentine CJ, Sansgiry S, Berger DH (2012) Disparities in the use of minimally invasive surgery for colorectal disease. J Gastrointest Surg 16:897–903. https://doi.org/10.1007/s11605-012-1844-3
Siemens DR, Mackillop WJ, Peng Y et al (2014) Processes of care and the impact of surgical volumes on cancer-specific survival: a population-based study in bladder cancer. Urology 84:1049–1057. https://doi.org/10.1016/j.urology.2014.06.070
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137:511–520
Keller DS, Hashemi L, Lu M, Delaney CP (2013) Short-term outcomes for robotic colorectal surgery by provider volume. J Am Coll Surg 217:1063–1069.e1. https://doi.org/10.1016/j.jamcollsurg.2013.07.390
Geller EJ, Matthews CA (2013) Impact of robotic operative efficiency on profitability. Am J Obstet Gynecol 209:20.e1-5. https://doi.org/10.1016/j.ajog.2013.03.030
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Richard J. Fantus, Andrew Cohen, Christopher B. Riedinger, Kristine Kuchta, Chi H. Wang, Katharine Yao, Sangtae Park declare they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fantus, R.J., Cohen, A., Riedinger, C.B. et al. Facility-level analysis of robot utilization across disciplines in the National Cancer Database. J Robotic Surg 13, 293–299 (2019). https://doi.org/10.1007/s11701-018-0855-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-018-0855-9