Abstract
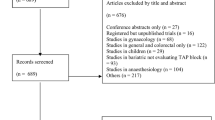
The transversus abdominis plane (TAP) block has been used to relieve pain after bariatric surgery but with conflicting data on its analgesic efficacy. We conducted this systematic review and meta-analysis with trial sequential analysis to clarify whether TAP block provides effective postoperative analgesia in patients undergoing bariatric surgery. We systematically searched the literature for any trials comparing TAP block with a control group (no block or sham injection). The primary outcome was pain scores at rest (analog scale, 0–10) at 2 postoperative hours. Secondary pain-related outcomes included pain scores at rest at 12 and 24 h and both dynamic pain scores and intravenous morphine equivalent consumption at 2, 12 and 24 h. Additional secondary outcomes sought were rates of postoperative infection, haematoma, visceral injury and local anaesthetic systemic toxicity. Thirteen trials totalling 1025 patients were identified. Pain scores at rest at 2 postoperative hours were significantly lower in the TAP block group compared with the control group, with a mean (95% CI) difference of − 1.8 (− 2.5, − 1.1); I2 = 85%; p < 0.00001. All other secondary pain-related outcomes were also significantly lower in the intervention group with the exception of dynamic pain scores and intravenous morphine equivalent consumption at 2 postoperative hours. Rates of block-related complications were not significantly different between groups. The overall quality of evidence was moderate-to-low. There is moderate-to-low level evidence that the TAP block improves postoperative analgesia after bariatric surgery up to 24 postoperative hours, when compared with a control group, without major reported complications. Clinical Trial Number
PROSPERO – registration number: CRD42019136542.




Similar content being viewed by others
References
Warner DO, Kim KO, Kim DH, et al. Comparative efficacy of bariatric surgery in the treatment of morbid obesity and diabetes mellitus: a systematic review and network meta-analysis. Obes Surg. 2019;29:2180–90.
Weingarten TN, Sprung J, Flores A, et al. Opioid requirements after laparoscopic bariatric surgery. Obes Surg. 2011;21:1407–12.
Subramani Y, Nagappa M, Wong J, et al. Death or near-death in patients with obstructive sleep apnoea: a compendium of case reports of critical complications. Br J Anaesth. 2017;119:885–99.
Ruiz-Tovar J, Albrecht E, Macfarlane A, et al. The TAP block in obese patients: pros and cons. Minerva Anestesiol. 2019;85:1024–31.
Baeriswyl M, Kirkham KR, Kern C, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121:1640–54.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, et al. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74:651–62.
Kirkham KR, Grape S, Martin R, et al. Analgesic efficacy of local infiltration analgesia vs. femoral nerve block after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Anaesthesia. 2017;72:1542–53.
Grape S, El-Boghdadly K, Albrecht E. Analgesic efficacy of PECS vs paravertebral blocks after radical mastectomy: a systematic review, meta-analysis and trial sequential analysis. J Clin Anesth. 2020;63:109745.
The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Version 6, 2019. Available from: https://training.cochrane.org/handbook/current.
Baeriswyl M, Kirkham KR, Jacot-Guillarmod A, et al. Efficacy of perineural vs systemic dexamethasone to prolong analgesia after peripheral nerve block: a systematic review and meta-analysis. Br J Anaesth. 2017;119:183–91.
Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Choi SW, Lam DM. Heterogeneity in meta-analyses. Comparing apples and oranges? Anaesthesia. 2017;72:532–4.
Carlisle JB. Systematic reviews: how they work and how to use them. Anaesthesia. 2007;62:702–7.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Wetterslev J, Thorlund K, Brok J, et al. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol. 2009;9:86.
Albrecht E1, Kirkham KR, Endersby RV, et al. Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: a prospective randomized controlled double-blinded trial. Obes Surg. 2013;23:1309–14.
De Oliveira GS, Fitzgerald P, Ahmad S, et al. Transversus abdominis plane infiltration for laparoscopic gastric banding: a pilot study. World J Gastrointest Surg. 2014;6:27–32.
Emile SH, Abdel-Razik MA, Elbahrawy K, et al. Impact of ultrasound-guided transversus abdominis plane block on postoperative pain and early outcome after laparoscopic bariatric surgery: a randomized double-blinded controlled trial. Obes Surg. 2019;29:1534–41.
Ibrahim M, El Shamaa H. Efficacy of ultrasound-guided oblique subcostal transversus abdominis plane block after laparoscopic sleeve gastrectomy: a double blind, randomized, placebo controlled study. Egypt J Anaesth. 2014;30:285–92.
Mittal T, Dey A, Siddhartha R, et al. Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc. 2018;32:4985–9.
Ruiz-Tovar J, Gonzalez G, Sarmiento A, et al. Analgesic effect of postoperative laparoscopic-guided transversus abdominis plane (TAP) block, associated with preoperative port-site infiltration, within an enhanced recovery after surgery protocol in one-anastomosis gastric bypass: a randomized clinical trial. Surg Endosc. 2020;
Saber AA, Lee YC, Chandrasekaran A, et al. Efficacy of transversus abdominis plane (TAP) block in pain management after laparoscopic sleeve gastrectomy (LSG): a double-blind randomized controlled trial. Am J Surg. 2019;217:126–32.
Said A, Balamoun HA. Continuous transversus abdominis plane blocks via laparoscopically placed catheters for bariatric surgery. Obes Surg. 2017;27:2575–82.
Shafeek AM, Gomaa GA, Abd El Malek Fady AG. A comparative study between ultrasound guided quadratus lumborum block versus ultrasound guided transversus abdominis plane block in laparoscopic bariatric surgery. Egypt J Hosp Med. 2018;70:2090–199.
Sherif Abeer A, Koptan HM, Soliman Samer MK. Feasibility and perioperative pain-relieving efficacy of ultrasound-guided transversus abdominis plane block in morbidly obese patients undergoing laparoscopic bariatric surgery. Res Op Anesth Int Care. 2015;2:50–6.
Sinha AL, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23:548–53.
Tülübaş EK, Seyit H, İpek B, et al. Laparoscopic transversus abdominal plane block is effective in multimodal analgesia for laparoscopic sleeve gastrectomy. Bakırköy Tıp Dergisi. 2019;15:198–203.
Wassef M, Lee DY, Levine JL, et al. Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J Pain Res. 2013;6:837–41.
Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017;118:424–9.
Jones DB, Abu-Nuwar MR, Ku CM, et al. Less pain and earlier discharge after implementation of a multidisciplinary enhanced recovery after surgery (ERAS) protocol for laparoscopic sleeve gastrectomy. Surg Endosc. 2020;
Albrecht E, Grape S, Frauenknecht J, et al. Low- versus high-dose intraoperative opioids: a systematic review with meta-analyses and trial sequential analyses. Acta Anaesthesiol Scand. 2020;64:6–22.
Acknowledgements
We are grateful to Mrs. Cécile Jaques (Medical Library, Research and Education Department, Lausanne University Hospital, Switzerland) for the assistance in the literature search.
Funding
This work was supported by departmental funding (Department of Anaesthesia, University Hospital of Lausanne, Lausanne, Switzerland, and Department of Anaesthesia and Intensive Care Medicine, Valais Hospital, Sion, Switzerland).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
EA has received grants from the Swiss Academy for Anaesthesia Research (SACAR), Lausanne, Switzerland (no grant numbers attributed), from B. Braun Medical AG, Sempach, Switzerland (no grant numbers attributed) and from the Swiss National Science Foundation to support his clinical research. EA has also received an honorarium from B. Braun Melsungen AG, Melsungen, Germany.
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grape, S., Kirkham, K.R. & Albrecht, E. The Analgesic Efficacy of Transversus Abdominis Plane Block After Bariatric Surgery: a Systematic Review and Meta-analysis with Trial Sequential Analysis. OBES SURG 30, 4061–4070 (2020). https://doi.org/10.1007/s11695-020-04768-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04768-x