Abstract
Introduction
Morbid obesity is an important risk factor for developing a venous thromboembolic events (VTE) after surgery. Fast-track protocols in metabolic surgery can lower the risk of VTE in the postoperative period by reducing the immobilization period. Administration of thromboprophylaxis can be a burden for patients. This study aims to compare extended to restricted thromboprophylaxis with low molecular weight heparin (LMWH) for patients undergoing metabolic surgery.
Methods
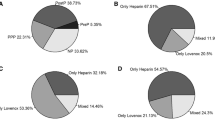
In this single center retrospective cohort study, data was collected from patients undergoing a primary Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) between 2014 and 2018. Patients operated in 2014–2017 received thromboprophylaxis for two weeks. In 2018, patients only received thromboprophylaxis during hospital admission. Patients already using anticoagulants were analyzed as a separate subgroup. The primary outcome measure was the rate of clinically significant VTEs within three months. Secondary outcome measures were postoperative hemorrhage and reoperations for hemorrhage.
Results
3666 Patients underwent a primary RYGB or SG following the fast-track protocol. In total, two patients in the 2014–2017 cohort were diagnosed with VTE versus zero patients in the 2018 cohort. In the historic group, 34/2599 (1.3%) hemorrhages occurred and in the recent cohort 8/720 (1.1%). Postoperative hemorrhage rates did not differ between the two cohorts (multivariable analysis, p = 0.475). In the subgroup of patients using anticoagulants, 21/347(6.1%) patients developed a postoperative hemorrhage. Anticoagulant use was a significant predictor of postoperative hemorrhage (p < 0.001).
Conclusion
Despite the restricted use of thromboprophylaxis administration since 2018, the rate of VTEs did not increase. This may be explained by quick mobilization and hospital discharge, as encouraged by the fast-track protocol. There was no significant difference in postoperative hemorrhage rates by thromboprophylaxis protocol. Short term use of thromboprophylaxis in metabolic surgery is safe in patients at low risk of VTE.

Similar content being viewed by others
Abbreviations
- ASMBS:
-
American Society for Metabolic and Bariatric Surgery
- BMI:
-
body mass index
- CI:
-
confidence interval
- DOAC:
-
direct oral anticoagulant
- DVT:
-
deep venous thrombosis
- ERABS:
-
enhanced recovery after bariatric surgery
- IRB:
-
institutional review board
- LMWH:
-
low molecular weight heparin
- OR:
-
odds ratio
- PE:
-
pulmonary embolism
- RYGB:
-
Roux-en-Y gastric bypass
- SG:
-
sleeve gastrectomy
- TWOR:
-
toetsingscommissie wetenschappelijk onderzoek Rotterdam
- VKA:
-
vitamin K antagonist
- VTE:
-
venous thromboembolic events
References
Kitahara CM, Flint AJ, Berrington de Gonzalez A, et al. Association between class III obesity (BMI of 40-59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11(7):e1001673.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014(8):Cd003641. https://doi.org/10.1002/14651858.CD003641.pub4
Nimeri AA, Bautista J, Ibrahim M, et al. Mandatory risk assessment reduces venous thromboembolism in bariatric surgery patients. Obes Surg. 2018;28(2):541–7.
Stein PD, Matta F. Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg. 2013;23(5):663–8.
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis: official journal of the American Society for Bariatric Surgery. 2013;9(4):493–7.
Thorell A, MacCormick AD, Awad S, et al. Guidelines for perioperative Care in Bariatric Surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40(9):2065–83.
Bhattacharya S, Kumar SS, Swamy PDK, et al. Deep vein thrombosis prophylaxis: are we overdoing? An Asian survey on trends in bariatric surgery with a systematic review of literature. Journal of minimal access surgery. 2018;14(4):285–90.
Thereaux J, Lesuffleur T, Czernichow S, et al. To what extent does Posthospital discharge chemoprophylaxis prevent venous thromboembolism after bariatric surgery?: results from a Nationwide cohort of more than 110,000 patients. Ann Surg. 2018;267(4):727–33.
Becattini C, Agnelli G, Manina G, et al. Venous thromboembolism after laparoscopic bariatric surgery for morbid obesity: clinical burden and prevention. Surg Obes Relat Dis: official journal of the American Society for Bariatric Surgery. 2012;8(1):108–15.
Blanchet MC, Gignoux B, Matussiere Y, et al. Experience with an enhanced recovery after surgery (ERAS) program for bariatric surgery: comparison of MGB and LSG in 374 patients. Obes Surg. 2017;27(7):1896–900.
Mannaerts GH, van Mil SR, Stepaniak PS, et al. Results of implementing an enhanced recovery after bariatric surgery (ERABS) protocol. Obes Surg. 2016;26(2):303–12.
Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Disease-a-month : DM. 2005;51(2–3):70–8.
Apers J, Wijkmans R, Totte E, et al. Implementation of mini gastric bypass in the Netherlands: early and midterm results from a high-volume unit. Surg Endosc. 2018;32(9):3949–55.
Biter LU, Gadiot RP, Grotenhuis BA, et al. The sleeve bypass trial: a multicentre randomized controlled trial comparing the long term outcome of laparoscopic sleeve gastrectomy and gastric bypass for morbid obesity in terms of excess BMI loss percentage and quality of life. BMC Obesity. 2015;2:30.
Gadiot RP, Biter LU, Zengerink HJ, et al. Laparoscopic sleeve gastrectomy with an extensive posterior mobilization: technique and preliminary results. Obes Surg. 2012;22(2):320–9.
van Mil SR, Duinhouwer LE, Mannaerts GHH, et al. The standardized postoperative checklist for bariatric surgery; a tool for safe early discharge? Obes Surg. 2017;27(12):3102–9.
Raftopoulos I, Ercole J, Udekwu AO, et al. Outcomes of roux-en-Y gastric bypass stratified by a body mass index of 70 kg/m2: a comparative analysis of 825 procedures. J Gastrointest Surg: official journal of the Society for Surgery of the Alimentary Tract. 2005;9(1):44–52. discussion -3
Raftopoulos I, Martindale C, Cronin A, et al. The effect of extended post-discharge chemical thromboprophylaxis on venous thromboembolism rates after bariatric surgery: a prospective comparison trial. Surg Endosc. 2008;22(11):2384–91.
Chan MM, Hamza N, Ammori BJ. Duration of surgery independently influences risk of venous thromboembolism after laparoscopic bariatric surgery. Surg Obes Relat Dis: official journal of the American Society for Bariatric Surgery. 2013;9(1):88–93.
Froehling DA, Daniels PR, Mauck KF, et al. Incidence of venous thromboembolism after bariatric surgery: a population-based cohort study. Obes Surg. 2013;23(11):1874–9.
Zafar SN, Miller K, Felton J, et al. Postoperative bleeding after laparoscopic roux en Y gastric bypass: predictors and consequences. Surg Endosc. 2018;33(1):272–80.
Zellmer JD, Mathiason MA, Kallies KJ, et al. Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic roux-en-Y gastric bypass? A meta-analysis. Am J Surg. 2014;208(6):903–10; discussion 9-10
Coblijn UK, Karres J, de Raaff CAL, et al. Predicting postoperative complications after bariatric surgery: the bariatric surgery index for complications, BASIC. Surg Endosc. 2017;31(11):4438–45.
Picetti R, Shakur-Still H, Medcalf RL, et al. What concentration of tranexamic acid is needed to inhibit fibrinolysis? A systematic review of pharmacodynamics studies. Blood Coagul Fibrinolysis : an international journal in haemostasis and thrombosis. 2019;30(1):1–10.
Klaassen RA, Selles CA, van den Berg JW, et al. Tranexamic acid therapy for postoperative bleeding after bariatric surgery. BMC Obes. 2018;5:36.
Altieri MS, Yang J, Hajagos J, et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32:4805–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the institutional review board (IRB) and the regional Medical Research Ethics Committee TWOR, Rotterdam, the Netherlands (protocol number 2018–03).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leeman, M., Biter, L.U., Apers, J.A. et al. A Single-Center Comparison of Extended and Restricted THROMBOPROPHYLAXIS with LMWH after Metabolic Surgery. OBES SURG 30, 553–559 (2020). https://doi.org/10.1007/s11695-019-04188-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04188-6