Abstract
Summary
This report describes epidemiology, burden, and treatment of osteoporosis in each of the 27 countries of the European Union (EU27).
Introduction
In 2010, 22 million women and 5.5 million men were estimated to have osteoporosis in the EU; and 3.5 million new fragility fractures were sustained, comprising 620,000 hip fractures, 520,000 vertebral fractures, 560,000 forearm fractures and 1,800,000 other fractures. The economic burden of incident and prior fragility fractures was estimated at € 37 billion. Previous and incident fractures also accounted for 1,180,000 quality-adjusted life years lost during 2010. The costs are expected to increase by 25 % in 2025. The majority of individuals who have sustained an osteoporosis-related fracture or who are at high risk of fracture are untreated and the number of patients on treatment is declining. The aim of this report was to characterize the burden of osteoporosis in each of the EU27 countries in 2010 and beyond.
Methods
The data on fracture incidence and costs of fractures in the EU27 were taken from a concurrent publication in this journal (Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden) and country specific information extracted.
Results
The clinical and economic burden of osteoporotic fractures in 2010 is given for each of the 27 countries of the EU. The costs are expected to increase on average by 25 % in 2025. The majority of individuals who have sustained an osteoporosis-related fracture or who are at high risk of fracture are untreated and the number of patients on treatment is declining.
Conclusions
In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis has decreased in recent years, suggesting that a change in healthcare policy concerning the disease is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Table of Contents
Introduction
Epidemiology and economic burden of osteoporosis in
-
1
Austria
-
2
Belgium
-
3
Bulgaria
-
4
Cyprus
-
5
Czech Republic
-
6
Denmark
-
7
Estonia
-
8
Finland
-
9
France
-
10
Germany
-
11
Greece
-
12
Hungary
-
13
Ireland
-
14
Italy
-
15
Latvia
-
16
Lithuania
-
17
Luxembourg
-
18
Malta
-
19
Netherlands
-
20
Poland
-
21
Portugal
-
22
Romania
-
23
Slovakia
-
24
Slovenia
-
25
Spain
-
26
Sweden
-
27
United Kingdom
Acknowledgements
List of abbreviations
- DDD:
-
Defined daily dosage
- DXA:
-
Dual-energy X-ray absorptiometry
- EU27:
-
Refers to the 27 countries of the European Union
- FRAX®:
-
WHO fracture risk assessment tool
- GDP:
-
Gross domestic product
- QALY:
-
Quality-adjusted life year
- SD:
-
Standard deviation
- T-score:
-
number of SDs by which BMD in an individual differs from the mean value expected in young healthy women
Introduction
Osteoporosis, literally “porous bone”, is a disease characterized by weak bone. It is a major public health problem, affecting hundreds of millions of people worldwide, predominantly postmenopausal women. The main clinical consequence of the disease is bone fractures. It is estimated that one in three women and one in five men over the age of fifty worldwide will sustain an osteoporotic fracture. Hip and spine fractures are the two most serious fracture types, associated with substantial pain and suffering, disability, and even death. As a result, osteoporosis imposes a significant burden on both the individual and society. During the past two decades, a range of medications has become available for the treatment and prevention of osteoporosis. The primary aim of pharmacological therapy is to reduce the risk of osteoporotic fractures.
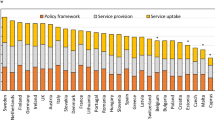
A recent report ‘Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden’ published concurrently with this report described the current burden of osteoporosis in the EU in 2010. Twenty two million women and 5.5 million men were estimated to have osteoporosis; and 3.5 million new fragility fractures were sustained, comprising 620,000 hip fractures, 520,000 vertebral fractures, 560,000 forearm fractures and 1,800,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures). The economic burden of incident and prior fragility fractures was estimated at € 37 billion. Incident fractures represented 66 % of this cost, long-term fracture care 29 % and pharmacological prevention 5 %. Previous and incident fractures also accounted for 1,180,000 quality-adjusted life years lost during 2010. The costs are expected to increase by 25 % in 2025. The majority of individuals who have sustained an osteoporosis-related fracture or who are at high risk of fracture are untreated and the number of patients on treatment is declining.
The objective of this report is to review and describe the current burden of osteoporosis in each of the EU member states. Epidemiological and health economic aspects of osteoporosis and osteoporotic fractures are summarised for 2010 with projections of the future prevalence of osteoporosis, the number of incident fractures, the direct and total cost of the disease including the value of QALYs lost. The report may serve as a basis for the formulation of healthcare policy concerning osteoporosis in general and the treatment and prevention of osteoporosis in particular. It may also provide guidance regarding the overall healthcare priority of the disease in each member state.
Epidemiology and Economic Burden of Osteoporosis in Austria
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, HP Dimai and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Hans Peter Dimai, Medical University of Graz, Department of Internal Medicine, Division of Endocrinology and Metabolism, Graz, Austria
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Austria
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Austria.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Austria, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Austria was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 87,000 new fragility fractures were sustained in Austria, comprising 16,000 hip fractures, 13,000 vertebral fractures, 13,000 forearm fractures and 44,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 799 million for the same year. Incident fractures represented 68 % of this cost, long-term fracture care 29 % and pharmacological prevention 4 %. Previous and incident fractures also accounted for 27,900 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 116,000 in 2025, representing an increase of 30,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 5,700, 4,400, 3,700 and 15,900, respectively. The burden of fractures in Austria in 2025 was estimated to increase by 28 % to € 1,025 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Austria in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Austria was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Austria
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,381,000 and 1,660,000 respectively in Austria in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 460,000 (Table 2). There were 28.7 DXA scan machines per million inhabitants [2] and guidelines for the assessment and treatment of osteoporosis are available [3, 4]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Austria [6]. Given that country specific incidences of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 322.9 and 757.2 respectively.
The number of incident fractures in 2010 was estimated at 87,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 16,000, 13,000, 13,000 and 44,000 respectively. 66 % of fractures occurred in women. These estimates are in close agreement with recently published data for 2008 [7].
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 2.44 % for hip and 2.75 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 74,000 and 84,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,018 (Table 8). Hip, vertebral and “other” fractures accounted for 505, 317 and 195 deaths respectively. Overall, approximately 55 % of deaths occurred in women.
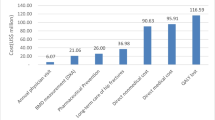
Cost of osteoporosis in Austria including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
For Austria, only inpatient costs the first year after hip fracture had been reported at the cut off date [8]. Total first year costs after fracture were imputed by applying the inpatient cost for Austria to the ratio of inpatient cost to total first year costs observed in Sweden, resulting in an estimated total first year hip fracture cost of € 13,527. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report. A recent publication provides similar estimates [7].
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 33,317 [9]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Cost of pharmacological fracture prevention including its administration were based on treatment uptake reported by IMS Health [10]. Annual drug cost for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 30 [11] and a DXA scan costing € 30 every second year to monitor treatment [11].
The cost of osteoporosis in 2010 was estimated at € 799 million (Table 10). These costs are close to recently published estimates for 2008 [7]. First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 540 million, € 229 million and € 30 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.8 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 421 million) followed by “other” (€ 300 million), spine (€ 36 million) and forearm fractures (€ 11 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites. The results are generally consistent with a recent cost of illness study undertaken for the year 2008 [7].

Fig. 1 Share (%) of fracture cost by fracture site in Austria. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 27,900 (Table 12). 66 % of the total QALY loss was incurred in women. Prior fractures accounted for 53 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 1.90 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 2.70 billion in Austria in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 20 %, 8 %, 1 %, 70 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 3.0 million in 2010 to 3.8 million in 2025, corresponding to an increase of 26 % (Table 14).
The total number of fractures was estimated to rise from 87,000 in 2010 to 116,000 in 2025 (Table 15), corresponding to an increase of 34 %. Hip, clinical spine, forearm and other fractures increased by 5,700, 4,400, 3,700 and 15,900 respectively. The increase in the number of fractures ranged from 28 % to 36 %, depending on fracture site. The increase was estimated to be particularly marked in men (49 %) compared to women (27 %). Note that the calculations assume no change in the age- and sex-specific incidence of fracture. In the case of hip fracture, there is evidence that age specific rates have been decreasing in recent years [13].
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 799 million in 2010 to € 1,025 million in 2025, corresponding to an increase of 28 % (Table 16). Costs incurred in women and men increased by 21 % and 43 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 27,900 in 2010 to 34,600 in 2025, corresponding to an increase of 24 % (Table 17). The increase was estimated to be particularly marked in men (38 %) compared to women (17 %). Incident and prior fractures accounted for 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 2.7 billion in 2010 to € 3.4 billion in 2025. The increase was estimated to be particularly marked in men (+39 %) compared to women (+18 %) (Table 18).
Treatment uptake
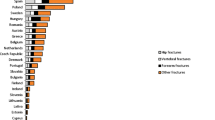
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Austria (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 3.06 % in 2001 to 6.1 % in 2006 but subsequently decreased to 5.17 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Austria were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 52 % and 51 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis J (2011) Personal communication.
3. Dimai HP, Pietschmann P, Resch H, Preisinger E, Fahrleitner-Pammer A, Dobnig H, Klaushofer K (2010) Austrian guidance for the pharmacologic treatment of osteoporosis in postmenopausal women. Wien Med Wochenschr 160: 586–89
4. Dimai HP, Pietschmann P, Resch H, Preisinger E, Fahrleitner-Pammer A, Dobnig H, Klaushofer K (2009) Austrian guidance for the pharmacological treatment of osteoporosis in postmenopausal women--update 2009. Wien Med Wochenschr Suppl: 1–34
5. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
6. Dimai HP (2008) Personal communication.
7. Dimai HP, Redlich K, Peretz M, Borgström F, Siebert U, Mahlich J (2012) Economic burden of osteoporotic fractures in Austria. Health Econ Rev 27: 12. doi: 10.1186/2191-1991-2-12.
8. Koeck CM, Schwappach DL, Niemann FM, Strassmann TJ, Ebner H, Klaushofer K (2001) Incidence and costs of osteoporosis-associated hip fractures in Austria. Wien Klin Wochenschr 113: 371–77
9. Seniorenheim (2011) Austria Nursing Home Cost. Accessed November, www.seniorenheim.at
10. IMS Health (2010) Data on pharmaceutical sales 2010.
11. NÖ Gebeitskrankenkasse (2011) Zusatzvereinbarung Honorarordning 2009. Accessed June, www.noegkk.at
12. United Nations Department of Economic and Social Affairs - Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
13. Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E, Chandran M, Borgström F (2011) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int 22: 685–92.
Epidemiology and Economic Burden of Osteoporosis in Belgium
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, M Hiligsmann, S Goemaere, J-Y Reginster and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Mickaël Hiligsmann, Department of Public Health, Epidemiology and Health Economics, University of Liège, Liège, Belgium AND Department of Health Service Research, CAPHRI School for Public Health and Primary Care, Maastricht University, Maastricht, Netherlands
Stefan Goemaere, Unit for Osteoporosis and Metabolic Bone Diseases, Ghent University Hospital, Ghent, Belgium.
Jean-Yves Reginster, Department of Public Health, Epidemiology and Health Economics, University of Liège, Liège, Belgium
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis ✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Belgium
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Belgium.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Belgium, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Belgium were reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 80,000 new fragility fractures were sustained in Belgium, comprising 15,000 hip fractures, 12,000 vertebral fractures, 12,000 forearm fractures and 41,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 606 million for the same year. Incident fractures represented 69 % of this cost, long-term fracture care 26 % and pharmacological prevention 5 %. Previous and incident fractures also accounted for 26,800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 99,000 in 2025, representing an increase of 19,000 fractures. Hip, clinical spine, forearm and other fractures was estimated to increase by 3,900, 2,900, 2,300 and 10,300, respectively. The burden of fractures in Belgium in 2025 was estimated to increase by 21 % to € 733 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial proportion of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Belgium in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Belgium was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Belgium
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,829,000 and 2,130,000 respectively in Belgium in 2010 (Table 1).
The number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 600,000 (Table 2), similar to an earlier estimate in 2008 [2]. There are 53 DXA scan machines per million inhabitants [3], and guidelines for the assessment and treatment of osteoporosis are available [4–8]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Belgium and we used a mean estimate for 2005–7 [10]. The incidence of hip fractures was determined using the national hospital database, which fully covers the annual hospital stays in Belgium (source: INAMI-RIZIV [Institut National d’Assurance Maladie Invalidité–Rijksinstituut voor Ziekte en Invaliditeitsverzekering] and SPF Public Health). Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 228.5 and 538.7 respectively.
The number of incident fractures in 2010 was estimated at 80,000 (Table 4). Incident hip, clinical vertebral, forearm and “other” fractures were estimated at 15,000, 12,000, 12,000 and 41,000 respectively. 66 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.88 % for hip and 2.04 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 74,000 and 81,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. These comprise approximately 30 % of deaths associated with fracture [11]. The number of causally related deaths in 2010 was estimated at 979 (Table 8). Hip, vertebral and “other” fractures accounted for 492, 310 and 177 deaths respectively. Overall, approximately 51 % of deaths occurred in women.
Cost of osteoporosis in Belgium including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 11,426 in Belgium [12] comparable to a more recent estimate [13]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 22,608 [14]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 19 and a DXA scan at € 34 every second year to monitor treatment [15].
The cost of osteoporosis in 2010 was estimated at € 606 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 419 million, € 157 million and € 29 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 4.8 % of the total cost. This cost is very likely overinflated since reimbursement for DXA only came into effect in August of 2010 and repeat DXA is only reimbursed at 5 years.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 308 million) followed by “other” (€ 232 million), spine (€ 28 million) and forearm fractures (€ 9 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Belgium. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 26,800 (Table 12). 67 % of the total QALY loss was incurred in women. Prior fractures accounted for 55 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 1.73 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 2.34 billion in Belgium in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 18 %, 7 %, 1 %, 74 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 4.0 million in 2010 to 4.6 million in 2025, corresponding to an increase of 17 % (Table 14).
The total number of fractures was estimated to rise from 80,000 in 2010 to 99,000 in 2025 (Table 15), corresponding to an increase of 24 %. Hip, clinical vertebral, forearm and other fractures increased by 3,900, 2,900, 2,300 and 10,300 respectively. The increase in the number of fractures ranged from 19 % to 26 %, depending on fracture site. The increase was estimated to be particularly marked in men (32 %) compared to women (20 %). Note that no change in the age and sex specific incidence was assumed over this period.
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 606 million in 2010 to € 733 million in 2025, corresponding to an increase of 21 % (Table 16). Costs incurred in women and men increased by 17 % and 29 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 26,800 in 2010 to 31,300 in 2025, corresponding to an increase of 17 % (Table 17). The increase was estimated to be particularly marked in men (25 %) compared to women (13 %). Incident and prior fractures accounted for 65 % and 35 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 2.3 billion in 2010 to € 2.8 billion in 2025. The increase was estimated to be particularly marked in men (+26 %) compared to women (+14 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Belgium (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 2 % in 2001 to 6.3 % in 2011 and thereafter decreased.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Belgium were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 45 % and 47 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk. Not all individuals at high risk as assessed by FRAX are eligible for reimbursement with the present reimbursement criteria.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Hiligsmann M (2010) Economic evaluation of osteoporosis management. PhD Thesis, University of Liège 2010.
3. Kanis JA (2011) Personal communication.
4. International Osteoporosis Foundation (2011) Osteoporosis in the European Union in 2008 - Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
5. Boonen S, Body JJ, Boutsen Y et al. (2005) Evidence-based guidelines for the treatment of postmenopausal osteoporosis: a consensus document of the Belgian Bone Club. Osteoporos Int 16: 239–254.
6. Devogelaer JP, Gomaere S, Boonen S et al. (2006) Evidence-based guidelines for the prevention and treatment of glucocorticoid-induced osteoporosis: a consensus document of the Belgian Bone Club. Osteoporos Int 17: 8–19.
7. Body J-J, Bergmann P Boonen S et al. (2010) Evidence-based guidelines for the pharmacological treatment. of postmenopausal osteoporosis: a consensus document by the Belgian Bone Club. Osteoporos Int 21: 1657–1680.
8. Body JJ, Bergmann P, Boonen S et al. (2011) Non-pharmacological management of osteoporosis: a consensus of the Belgian Bone Club. Osteoporos Int 22: 2769–2788.
9. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
10. Hiligsmann M, Bruyère O, Roberfroid D et al. (2012) Trends in Hip Fracture Incidence and in the Prescription of Antiosteoporosis Medications During the Same Time Period in Belgium (2000–2007). Arthritis Care & Research 64:744–50.
11. Kanis JA, Oden A, Johnell O, Laet CD, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture Bone. 30:468–73.
12. Bouee S, Lafuma A, Fagnani F, Meunier PJ, Reginster JY (2006) Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 26: 1063–72
13. Hiligsmann M, Gathon HJ, Bruyère O, Daubie M, Dercq JP, Parmentier Y, Reginster JY. Hospitalisation costs of hip fractures in Belgium. Osteoporosis Int 2011, 22 S1, S332. (abstract)
14. Autier P, Haentjens P, Bentin J, Baillon JM, Grivegnee AR, Closon MC, Boonen S (2000) Costs induced by hip fractures: a prospective controlled study in Belgium. Belgian Hip Fracture Study Group. Osteoporos Int 11: 373–80
15. INAMI-RIZIV Institute national d’assurance maladie-invalidité (2011). Accessed June: http://www.inami.fgov.be/insurer/fr/rate/pdf/last/doctors/rx20110601fr.pdf
16. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Bulgaria
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, A-M Borissova, R Kovacheva, A Shinkov, M Boyanov, R Rachkov, P Popivanov, Z Kolarov, and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Anna-Maria Borissova,, Department of Thyroid and Metabolic Bone Diseases, University Hospital of Endocrinology, Medical University of Sofia, Sofia, Bulgaria
Russanka Kovacheva, Department of Thyroid and Metabolic Bone Diseases, University Hospital of Endocrinology, Medical University of Sofia, Sofia, Bulgaria
Alexander Shinkov,, Department of Thyroid and Metabolic Bone Diseases, University Hospital of Endocrinology, Medical University of Sofia, Sofia, Bulgaria
Mihail Boyanov, Department of Internal Medicine, Clinic of Endocrinology and Metabolism, University Hospital Alexandrovska, Medical University of Sofia, Sofia, Bulgaria
Racho Rachkov, Department of Internal Medicine, Clinic of Rheumatology, University Hospital Ivan Rilski, Medical University of Sofia, Sofia, Bulgaria
Plamen Popivanov, Department of Internal Medicine, Bone Metabolic Unit, University Hospital Alexandrovska, Medical University of Sofia, Sofia, Bulgaria
Zlatimir Kolarov, Department of Internal Medicine, Clinic of Endocrinology and Metabolism, University Hospital Alexandrovska, Medical University of Sofia, Sofia, Bulgaria
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Bulgaria
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Bulgaria.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Bulgaria, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Bulgaria was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 38,000 new fragility fractures were sustained in Bulgaria, comprising 5,900 hip fractures, 6,400 vertebral fractures, 6,500 forearm fractures and 19,400 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 42 million for the same year. Incident fractures represented 71 % of this cost, long-term fracture care 25 % and pharmacological prevention 3 %. Previous and incident fractures also accounted for 12,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 40,000 in 2025, representing an increase of 1,400 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 400, 200, 100 and 600, respectively. The burden of fractures in Bulgaria in 2025 was estimated to increase by 5 % to € 45 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Bulgaria in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Bulgaria was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Bulgaria
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,270,000 and 1,606,000 respectively in Bulgaria in 2010 (Table 1). A more recent census in 2011 indicates a small decrease in the population aged 50 years or more from 2.88 million to 2.84 million [2].
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 420,000 (Table 2). Allowing for differences in the calculation of T-scores the estimate for women is similar to previously published data [3]. There are 1.2 DXA scan machines per million inhabitants [4], and guidelines for the assessment and treatment of osteoporosis are available [5]. A country specific FRAX model for the assessment of fracture risk is not available for Bulgaria.
Incidence data were not available for Bulgaria; therefore data for hip fractures was imputed from Romanian age-standardized incidence rates [7]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 170.3 and 282.3 respectively.
The number of incident fractures in 2010 was estimated at 38,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 6,000, 6,000, 6,000 and 19,000 respectively. 56 % of fractures occurred in women. The number of hip fractures is consistent with Government sources when accounting for multiple admissions [8].
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.09 % for hip and 1.14 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age, presented in Table 5, are consistent with an earlier report of a survey in Bulgarian women [9].
In the population over 50 years of age, the number of individuals with hip and clinical vertebral fractures that occurred before 2010 was estimated at 31,000 and 33,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 647 (Table 8). Hip, vertebral and “other” fractures accounted for 294, 283 and 71 deaths respectively. Overall, approximately 47 % of deaths occurred in women.
Cost of osteoporosis in Bulgaria including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 1,826 in Bulgaria based on hip fracture costs in Slovenia [10]. The costs are consistent with the information available from the Romanian National Health Insurance Fund [11]. No other fracture costs were available. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 4,044 [12]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 2 [13] and a DXA scan costing € 59 [14] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 42 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 30 million, € 11 million and € 1 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.1 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 20 million) followed by “other” (€ 18 million), spine (€ 2 million) and forearm fractures (€ 1 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Bulgaria. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 12,300 (Table 12). 58 % of the total QALY loss was incurred in women. Prior fractures accounted for 52 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 118 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 160 million in Bulgaria in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 19 %, 7 %, 1 %, and 74 %, respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to be approximately constant at 2.9 million between 2010 and 2025 (Table 14).
The total number of fractures was estimated to rise from 38,000 in 2010 to 40,000 in 2025 (Table 15), corresponding to an increase of 4 %. Hip, clinical spine, forearm and other fractures increased by 400, 200, 100 and 600 respectively. The increase in the number of fractures ranged from 2 % to 8 %, depending on fracture site. The increase in women was estimated at 7 % while a decrease is expected in men.
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 42 million in 2010 to € 45 million in 2025, corresponding to an increase of 5 % (Table 16). Costs incurred in women and men increased by 9 % and 1 % respectively.
The total number of QALYs lost due to fracture was estimated to rise only from 12,300 in 2010 to 12,800 in 2025, corresponding to an increase of 4 % (Table 17). The increase in men was estimated to be 1 % and the increase in women was estimated at 6 %. Incident and prior fractures accounted for 46 % and 54 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 160 million in 2010 to € 168 million in 2025. The increase was estimated to be 1 % in men and 7 % in women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Bulgaria (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.01 % in 2001 to 0.53 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Bulgaria were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 98 % and 95 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. National Statistical Institute (NSI) (2011) 2011 census final results. Accessed January 2013. http://censusresults.nsi.bg/Census/Reports/2/2/R1.aspx
2. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
3. Borissova A-M, Rashkov R, Boyanov M, Shinkov A, Popivanov P, Temelkova N, Vlahov J, Gavrailova M (2011) Femoral neck bone mineral density and 10-year absolute fracture risk in a national representative sample of Bulgarian women aged 50 years and older. Arch Osteoporosis 6:189–195
4. Kanis J (2011) personal communication, data on file.
5. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
6. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
7. Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2012) Incidence of hip fracture in Romania and the development of a Romanian FRAX model. Calcif Tiss Intl 92: 429–36
8. Boyanov MA (2006) Prevalence of Low Central Bone Mineral Density in a Bulgarian Female Referral Population: a Pilot Study. Rheumatol Int 26:523–9
9. Lesnyak O, Nauroy L (2010) The Eastern European and central Asian regional audit. Epidemiology, cost and burden of osteoporosis in 2010. International Osteoporosis Foundation, Nyon. Available at http://www.iofbonehealth.org/eastern-european-central-asian-audit
10. Dzajkovska B, Wertheimer AI, Mrhar A (2007) The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29: 404–11
11. Borissova A-M, personal communication, December 2012.
12. Nursing homes (2011) Personal communication—average of three Bulgarian nursing homes (750, 650, and 550 lev/month).
13. Vatkova J (2011) National Health Insurance Fund in Bulgaria. Personal communication.
14. International Osteoporosis Foundation (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges. IOF, Nyon
15. Ministry of Health Bulgaria (2011). Accessed December 2011. www.mh.government.bg/Articles.aspx?lang=bg-BG&pageid=383&categoryid=3999.
16. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Cyprus
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, GL Georgiades, C Kaisis and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
George L Georgiades, Cyprus Association for Musculoskeletal Diseases, Larnaca, Cyprus
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Cyprus
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Cyprus.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Cyprus, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Cyprus was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 5,000 new fragility fractures were sustained in Cyprus, comprising 800 hip fractures, 800 vertebral fractures, 1,000 forearm fractures and 2,600 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 52 million for the same year. Incident fractures represented 65 % of this cost, long-term fracture care 13 % and pharmacological prevention 22 %. Previous and incident fractures also accounted for 1,800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 7,700 in 2025, representing an increase of 2,600 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 440, 390, 420 and 1,300, respectively. The burden of fractures in Cyprus in 2025 was estimated to increase with 47 % to € 76 million.
Conclusions There is a high cost of osteoporosis with a substantial projected increase of the economic burden driven by an aging population, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Cyprus in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Cyprus was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Cyprus
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 150,000 and 161,000 respectively in Cyprus in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 40,000 (Table 2). There are 23.9 DXA scan machines per million (m) inhabitants [2], and there are no guidelines for osteoporosis treatment [3]. A country specific FRAX model for the assessment of fracture risk is not available for Cyprus.
Incidence data was not available for Cyprus, therefore data for hip fractures was imputed from Greek age-standardized incidence rates [5]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 212.7 and 494.0 respectively. The incidence of vertebral, forearm and “other” fractures was imputed using the methods described in Chapter 3 of the main report.
The number of incident fractures in 2010 was estimated at approximately 5,000 (Table 4). Incident hip, clinical spine, forearm fractures were estimated at approximately 1,000 each and “other” fractures were estimated at 3,000. 61 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.58 % for hip and 1.98 % for vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 5,000 and 6,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 53 (Table 8). Hip, vertebral and “other” fractures accounted for 27, 19 and 8 deaths respectively. Overall, approximately 46 % of deaths occurred in women.
Cost of osteoporosis in Cyprus including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 14,821 in Cyprus based on cost estimates in Italy [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 15,261 [7,8], approximated by adjusting the Bulgarian cost for health adjusted price levels) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 14 [9] and a DXA scan costing € 75 [10] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 52 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 34 million, € 7 million and € 12 million, respectively. It is notable that pharmacological fracture prevention costs accounted for only 22.4 % of the total cost.
When stratifying costs of osteoporosis by fracture type, “other” fractures were most costly (€ 20 million) followed by hip (€ 17 million), spine (€ 2 million) and forearm fractures (€ 1 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in Cyprus. Note that costs for fracture prevention therapy and monitoring are not included.
The number of QALYs lost due to osteoporosis in 2010 was estimated at 1,800 (Table 12). Prior fractures accounted for 58 % of the total loss and 63 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 78 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 130 million in Cyprus in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 26 %, 5 %, 9 % and 60 %, respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 311,000 in 2010 to 430,000 in 2025, corresponding to an increase of 38 % (Table 14).
The total number of fractures was estimated to rise from 5,000 in 2010 to 8,000 in 2025 (Table 15), corresponding to an increase of 50 %. Hip, clinical spine, forearm and other fractures increased by 400, 400, 400 and 1,300 respectively. The increase in the number of fractures ranged from 44 % to 57 %, depending on fracture site. The increase was estimated to be particularly marked in men (49 %) compared to women (51 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 52 million in 2010 to € 76 million in 2025, corresponding to an increase of 47 % (Table 16). Costs incurred in women and men increased by 47 % and 48 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 1,800 in 2010 to 2,300 in 2025, corresponding to an increase of 29 % (Table 17). The increase was estimated to be particularly marked in men (38 %) compared to women (24 %). Incident and prior fractures accounted for 73 % and 27 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 130 million in 2010 to € 177 million in 2025. The increase was estimated to be particularly marked in men (+42 %) compared to women (+33 %) (Table 18).
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. International Osteoporosis Foundation (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Paspati I, Galanos A, Lyritis GP (1998) Hip fracture epidemiology in Greece during 1977–1992. Calcif Tissue Int 62: 542–47
6. Visentin P, Ciravegna R, Fabris F (1997) Estimating the cost per avoided hip fracture by osteoporosis treatment in Italy. Maturitas 26: 185–92
7. Nursing homes (2011) Personal communication—average of three Bulgarian nursing homes (750, 650, and 550 lev/month).
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. Ministry of Health Cyprus (2011). Accessed June: www.moh.gov.cy
10. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in the Czech Republic
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, M Bayer and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Milan Bayer, Charles University Prague, Medical Faculty in Hradec Králové, Hradec Králové, Czech Republic
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Czech Republic
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in the Czech Republic.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in the Czech Republic, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the Czech Republic was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 72,000 new fragility fractures were sustained in the Czech Republic, comprising 12,000 hip fractures, 11,000 vertebral fractures, 12,000 forearm fractures and 37,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 273 million for the same year. Incident fractures represented 60 % of this cost, long-term fracture care 20 % and pharmacological prevention 19 %. Previous and incident fractures also accounted for 22,800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 94,000 in 2025, representing an increase of 21,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 4,700, 3,400, 2,400 and 11,000, respectively. The burden of fractures in the Czech Republic in 2025 was estimated to increase by 29 % to € 352 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in the Czech Republic in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in the Czech Republic was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in the Czech Republic
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,710,000 and 2,092,000 respectively in the Czech Republic in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 530,000 (Table 2). There are 5.2 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for the Czech Republic [5]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 277.1 and 566.6 respectively.
The number of incident fractures in 2010 was estimated at 72,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 12,000, 11,000, 12,000 and 37,000 respectively. 61 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.55 % for hip and 1.69 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 59,000 and 64,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,034 (Table 8). Hip, vertebral and “other” fractures accounted for 501, 380 and 154 deaths respectively. Overall, approximately 50 % of deaths occurred in women.
Cost of osteoporosis in the Czech Republic including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 5,169 in the Czech Republic [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 10,614 [6]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 18 (approximated by adjusting Polish cost for health adjusted price levels [7]) and a DXA scan costing € 32 [8] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 273 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 165 million, € 56 million and € 53 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 19.2 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 110 million) followed by “other” (€ 96 million), spine (€ 11 million) and forearm fractures (€ 4 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in the Czech Republic. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 22,800 (Table 12). Prior fractures accounted for 52 % of the total loss and 63 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 630 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 900 million in Czech Republic in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 18 %, 6 %, 6 %, and 70 %, respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 3.8 million in 2010 to 4.3 million in 2025, corresponding to an increase of 13 % (Table 14).
The total number of fractures was estimated to rise from 72,000 in 2010 to 94,000 in 2025 (Table 15), corresponding to an increase of 31 %. Hip, clinical spine, forearm and other fractures increased by 4,700, 3,400, 2,400 and 11,000 respectively. The increase in the number of fractures ranged from 20 % to 39 %, depending on fracture site. The increase was estimated to be similar in men (29 %) and women (30 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 273 million in 2010 to € 352 million in 2025, corresponding to an increase of 29 % (Table 16). Costs incurred in women and men increased by 27 % and 33 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 22,800 in 2010 to 27,900 in 2025, corresponding to an increase of 22 % (Table 17). The increase was estimated to be particularly marked in men (27 %) compared to women (19 %). Incident and prior fractures accounted for 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 900 million in 2010 to € 1.1 billion in 2025. The increase was estimated to be particularly marked in men (+28 %) compared to women (+22 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig.2 Treatment uptake in the Czech Republic (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.64 % in 2001 to 2.29 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in the Czech Republic were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 88 % and 76 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis J (2011) personal communication, data on file.
3. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Stepan J (2010) Personal communication.
6. Kudrna K, Krska Z (2005) Expense analysis of the proximal femoral fractures treatment. [Rozbor nákladů na léčbu zlomenin horního konce stehenní kosti]. Rozhl Chir 84: 631–34
7. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
8. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
9. SÚKL State Institute for Drug Control in Czech Republic (2011). Accessed in June: www.sukl.eu/
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Denmark
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, B Abrahamsen and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Bo Abrahamsen, Department of Medicine F, Gentofte Hospital, Hellerup, Denmark.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Denmark
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Denmark.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Denmark, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Denmark was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 66,000 new fragility fractures were sustained in Denmark, comprising 12,000 hip fractures, 10,000 vertebral fractures, 10,000 forearm fractures and 34,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 1,055 million for the same year. Incident fractures represented 68 % of this cost, long-term fracture care 28 % and pharmacological prevention 4 %. Previous and incident fractures also accounted for 20,200 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 86,000 in 2025, representing an increase of 20,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 4,300, 3,200, 2,400 and 10,300, respectively. The burden of fractures in Denmark in 2025 was estimated to increase by 27 % to € 1,344 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Denmark in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Denmark was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis. Where possible, country-specific data were used (see below).
Epidemiology of osteoporosis in Denmark
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 950,000 and 1,053,000 respectively in Denmark in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 280,000 (Table 2). Note that the numbers do not include patients with vertebral osteoporosis (spine T-score <−2.5) in whom femoral neck BMD lies in the normal or osteopenic range. There are 14.6 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Epidemiology of fracture in Denmark
Data on hip fracture incidence are available for Denmark [5], based on admission statistics from the Danish National Board of Health. These rates also included repeat admissions which overestimate somewhat the hip fracture incidence. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not available, these were imputed using the methods described in Chapter 3 of the main report. Briefly, it was assumed for each age and sex that the ratio of the incidence of non-hip fracture to hip fractures in Sweden would be comparable to the ratio of vertebral fracture incidence to hip fracture incidence in Denmark. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 386.0 and 853.0 respectively.
The number of incident fractures in 2010 was estimated at 66,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 12,000, 10,000, 10,000 and 34,000 respectively. 63 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 2.48 % for hip and 2.92 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 50,000 and 59,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 879 (Table 8). Hip, vertebral and “other” fractures accounted for 427, 293 and 158 deaths respectively. Overall, approximately 52 % of deaths occurred in women.
Cost of osteoporosis in Denmark including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 25,117 in Denmark [7, 8]. No other fracture costs were available. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 64,831 [9]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 160 [10] and a DXA scan costing € 187 [10] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 1,055 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 718 million, € 300 million and € 37 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.5 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 564 million) followed by “other” (€ 431 million), spine (€ 12 million) and forearm fractures (€ 12 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in Denmark. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 20,200 (Table 12). Prior fractures accounted for 50 % of the total loss and 63 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 1.7 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 2.76 billion in Denmark in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 26 %, 11 %, 1 %, 62 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 2.0 million in 2010 to 2.4 million in 2025, corresponding to an increase of 18 % (Table 14).
The total number of fractures was estimated to rise from 66,000 in 2010 to 86,000 in 2025 (Table 15), corresponding to an increase of 30 %, assuming that age-specific fracture rates remain unchanged over time. At present, hip fracture rates are falling in Denmark [13], so that if this trend continues, the present analysis may be an overestimate. Hip, spine, forearm and other fractures increased by 4,300, 3,200, 2,400 and 10,300, respectively. The increase in the number of fractures ranged from 23 % to 35 %, depending on fracture site. The increase was estimated to be particularly marked in men (35 %) compared to women (28 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 1055 million in 2010 to € 1344 million in 2025, corresponding to an increase of 27 % (Table 16). Costs incurred in women and men increased by 23 % and 34 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 20,200 in 2010 to 24,900 in 2025, corresponding to an increase of 23 % (Table 17). The increase was estimated to be particularly marked in men (30 %) compared to women (19 %). Incident and prior fractures accounted for 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 2.8 billion in 2010 to € 3.4 billion in 2025. The increase was estimated to be particularly marked in men (+32 %) compared to women (+21 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Denmark (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.79 % in 2001 to 5.71 % in 2011. This is near the European average but high by North European standards.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in each country were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 50 % and 54 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis J (2011) personal communication, data on file.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468-89
5. Abrahamsen B (2011) Personal communication.
6. Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32; 468–473.
7. Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA (2007) Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries—an economic evaluation based on the fracture intervention trial. Osteoporos Int 18: 1047–61
8. Kronborg C, Vass M, Lauridsen J, Avlund K (2006) Cost effectiveness of preventive home visits to the elderly: economic evaluation alongside randomized controlled study. Eur J Health Econ 7: 238–46
9. Nurmi I, Narinen A, Luthje P, Tanninen S (2003) Cost analysis of hip fracture treatment among the elderly for the public health services: a 1-year prospective study in 106 consecutive patients. Arch Orthop Trauma Surg 123:551-554
10. The Danish Ministry of Health (2000). Takstsystem 2011 ISBN 978-87-7601304-2:
11. Danish Medicines Agency (2011). Accessed July: http://www.medicinpriser.dk
12. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
13. Abrahamsen B, Vestergaard P (2010) Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int 21: 373–380.
Epidemiology and Economic Burden of Osteoporosis in Estonia
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, K Maasalu and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Katre Maasalu, Department of Traumatology and Orthopaedics, University of Tartu, Estonia
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Estonia
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Estonia.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Estonia, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Estonia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 9,000 new fragility fractures were sustained in Estonia, comprising 1,600 hip fractures, 1,400 vertebral fractures, 1,400 forearm fractures and 4,300 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 30 million for the same year. Incident fractures represented 73 % of this cost, long-term fracture care 23 % and pharmacological prevention 3 %. Previous and incident fractures also accounted for 2,800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 10,000 in 2025, representing an increase of 1,500 fractures. Hip, clinical spine (vertebral), forearm and other fractures were estimated to increase by 400, 200, 100 and 800, respectively. The burden of fractures in Estonia in 2025 was estimated to increase by 18 % to € 35 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above whom received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Estonia in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Estonia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Estonia
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 188,000 and 297,000 respectively in Estonia in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 80,000 (Table 2). There are 8.9 DXA scan machines per million (m) inhabitants, and guidelines for the assessment and treatment of osteoporosis are available [2]. A country specific FRAX model for the assessment of fracture risk is not available for Estonia. Based on the likelihood that the fracture rate and mortality in Lithuania was equal to Estonia, the FRAX model for Lithuania was used as a surrogate,
There are limited data on fracture rates in Estonia and no specific information on hip fracture incidence [4] Data for hip fractures were imputed from Finnish age-standardized incidence rates [5]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 238 and 440 respectively.
The number of incident fractures in 2010 was estimated at 8,700 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 1,600, 1,400, 1,400 and 4,300 respectively. 69 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.52 % for hip and 1.54 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of both men and women with hip or vertebral fractures that occurred before 2010 was estimated at 7,000 (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 134 (Table 8). Hip, vertebral and “other” fractures accounted for 65, 50 and 19 deaths respectively. Overall, approximately 54 % of deaths occurred in women.
Cost of osteoporosis in Estonia including and excluding value of QALYs Lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
In Estonia, the cost of a hip fracture has been estimated at € 5,580 using the fracture cost in Finland [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 10,483 [7,8], based on Finnish cost of nursing home that was PPP adjusted) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 12 [9] and a DXA scan costing € 187 [9] every second year to monitor treatment. The cost is conservative in that monitoring is usually conducted annually.
The cost of osteoporosis in 2010 was estimated at € 30 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 22 million, € 7 million and € 1 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.3 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 15 million) followed by “other” (€ 12 million), spine (€ 1.5 million) and forearm fractures (€ 0.5 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in Estonia. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 2,800 (Table 12). 72 % of the total QALY loss was incurred in women. Prior fractures accounted for 52 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 60 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 90 million in Estonia in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 25 %, 8 %, 1 %, 66 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 485,000 in 2010 to 511,000 in 2025, corresponding to an increase of 5 % (Table 14).
The total number of fractures was estimated to rise from 9,000 in 2010 to 10,000 in 2025 (Table 15), corresponding to an increase of 11 %. Hip, clinical spine, forearm and other fractures increased by 400, 200, 100 and 800 respectively. The increase in the number of fractures ranged from 9 % to 23 %, depending on fracture site. The increase was estimated to be 19 % in men and 17 % in women.
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 30 million in 2010 to € 35 million in 2025, corresponding to an increase of 18 % (Table 16). Costs incurred in both women and men increased by 18 %.
The total number of QALYs lost due to fracture was estimated to rise from 2,800 in 2010 to 3,200 in 2025, corresponding to an increase of 15 % (Table 17). The increase was estimated to be particularly marked in men (17 %) compared to women (15 %). Incident and prior fractures accounted for 53 % and 47 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 89 million in 2010 to € 104 million in 2025. The increase was estimated to be 17 % in men and 16 % in women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 1 Treatment uptake in Estonia (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.13 % in 2001 to 1.66 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Estonia were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 93 % and 86 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
3. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
4. National Institute for Health Development, Estonia. Accessed January 2013 http://pxweb.tai.ee/esf/pxweb2008/Database_en/Morbidity/databasetree.asp
5. Kroger H (2011) Personal communication.
6. Nurmi I, Narinen A, Luthje P, Tanninen S (2003) Cost analysis of hip fracture treatment among the elderly for the public health services: a 1-year prospective study in 106 consecutive patients. Arch Orthop Trauma Surg 123: 551–54
7. Hujanen T, Kapiainen S, Tuominen U, Pekurinen M (2008) Terveydenhuollon yksikkökustannukset Suomessa vuonna 2006.
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. Estonian Health Insurance Fund (2011). Available at Riigi Teataja: www.riigiteataja.ee/akt/121062011024#para17
10. Estonian Medicine Information (Raviminfo) (2011). Accessed August: http://www.raviminfo.ee/otsing.php
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Finland
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, H Kröger and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Heikki Kröger, Department of Orthopaedics, Traumatology and Hand Surgery, Kuopio University Hospital and University of Eastern Finland, Kuopio, Finland
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Finland
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Finland.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Finland, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Finland was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 36,000 new fragility fractures were sustained in Finland, comprising 7,000 hip fractures, 6,000 vertebral fractures, 6,000 forearm fractures and 19,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 383 million for the same year. Incident fractures represented 70 % of this cost, long-term fracture care 27 % and pharmacological prevention 3 %. Previous and incident fractures also accounted for 12,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 49,000 in 2025, representing an increase of 13,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 2,900, 2,000, 1,200 and 6,600, respectively. The burden of fractures in Finland in 2025 was estimated to increase by 34 % to € 514 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Finland in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Finland was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Finland
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 960,000 and 1,130,000 respectively in Finland in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 300,000 (Table 2). There are 16.8 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk ( http://www.shef.ac.uk/FRAX/).
Data on the incidence of hip fractures are available for Finland [5–7] and that used to build the FRAX model was chosen for this study [7]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Empirical data are expected in the near future [8]. Fracture incidence is presented in Table 3. Standardized to the EU27 population for 2010, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 238.0 and 440.0 respectively.
The number of incident fractures in 2010 was estimated at 36,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 7,000, 6,000, 6,000 and 19,000 respectively. 60 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.64 % for hip and 1.78 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 34,000 and 37,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 425 (Table 8). Hip, vertebral and “other” fractures accounted for 209, 144 and 72 deaths respectively. Overall, approximately 47 % of deaths occurred in women.
Cost of osteoporosis in Finland including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
In Finland, the cost of a hip fracture has been estimated at € 16,066 [10] No other fracture costs were available. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 32,930 [11]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 17 [12] and a DXA scan costing € 146 [12] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 383 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 269 million, € 104 million and € 10 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 2.6 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 198 million) followed by “other” (€ 151 million), spine (€ 18 million) and forearm fractures (€ 5 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in Finland. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 12,300 (Table 12). 62 % of the total QALY loss was incurred in women. Prior fractures accounted for 55 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 830 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 1.21 billion in Finland in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 22 %, 9 %, 1 %, 68 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 2.1 million in 2010 to 2.3 million in 2025, corresponding to an increase of 12 % (Table 14).
The total number of fractures was estimated to rise from 36,000 in 2010 to 49,000 in 2025 (Table 15), corresponding to an increase of 36 %. Hip, clinical spine, forearm and other fractures increased by 2,900, 2,000, 1,200 and 6,600 respectively. The increase in the number of fractures ranged from 21 % to 44 %, depending on fracture site. The increase was estimated to be particularly marked in men (42 %) compared to women (30 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 383 million in 2010 to € 514 million in 2025, corresponding to an increase of 34 % (Table 16). Costs incurred in women and men increased by 28 % and 44 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 12,300 in 2010 to 15,800 in 2025, corresponding to an increase of 28 % (Table 17). The increase was estimated to be particularly marked in men (38 %) compared to women (22 %). Incident and prior fractures accounted for 59 % and 41 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 1.2 billion in 2010 to € 1.6 billion in 2025. The increase was estimated to be particularly marked in men (+40 %) compared to women (+24 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Finland (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.38 % in 2001 to 4.22 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Finland were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the numberof individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 84 % and 69 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis J (2011) personal communication, data on file.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468-89
5. Sund R (2007) Utilization of routinely collected administrative data in monitoring the incidence of aging dependent hip fracture. Epidemiol Perspect Innov. 4:2
6. Huusko T, Arnala I, Aro H, Impivaara O, Jäntti P, Laukkanen P, Piirtola M, Sipilä R, Sund R, Tarkkila P, Varis T, Välimäki VV: Hip fracture—Current Care Summary. Duodecim 2011;127:1508–9. http://www.kaypahoito.fi/web/kh/suositukset/naytaartikkeli/…/ccs00092
7. Kroger H and Sund R (2011) Personal communication.
8. Koski AM, Patala A, Patala E, Sund R (2013) Incidence of osteoporotic fractures in elderly women and men in Finland during 2005–2006—a population-based study. Scandinavian Journal of Surgery, in press.
9. Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32; 468–473.
10. Nurmi I, Narinen A, Luthje P, Tanninen S (2003) Cost analysis of hip fracture treatment among the elderly for the public health services: a 1-year prospective study in 106 consecutive patients. Arch Orthop Trauma Surg 123: 551–54
11. Hujanen T, Kapiainen S, Tuominen U, Pekurinen M (2008) Terveydenhuollon yksikkökustannukset Suomessa vuonna 2006.
12. The Social Insurance Institution of Finland (2011). Accessed July: http://kela.fi/
13. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in France
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Local author—to be determined
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in France
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in France.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in France, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in France was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 377,000 new fragility fractures were sustained in France, comprising 74,000 hip fractures, 56,000 vertebral fractures, 56,000 forearm fractures and 191,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 4,853 million for the same year. Incident fractures represented 66 % of this cost, long-term fracture care 27 % and pharmacological prevention 7 %. Previous and incident fractures also accounted for 139,400 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 491,000 in 2025, representing an increase of 115,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 24,500, 17,200, 12,900 and 60,000, respectively. The burden of fractures in France in 2025 was estimated to increase by 26 % to € 6,111 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in France in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in France was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in France
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 10,287,000 and 12,358,000 respectively in France in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 3,480,000 (Table 2). There are 29.1 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for France [5]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 168 and 443 respectively.
The number of incident fractures in 2010 was estimated at 377,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 74,000, 56,000, 56,000 and 191,000 respectively. 68 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.92 % for hip and 1.92 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 435,000 and 436,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 4,233 (Table 8). Hip, vertebral and “other” fractures accounted for 2,098, 1,256 and 880 deaths respectively. Overall, approximately 51 % of deaths occurred in women.
Cost of osteoporosis in France including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture in France was not available. Therefore, it was imputed from the UK cost of a hip fracture by adjusting for differences in health care price levels and estimated at € 12,030 [6,7]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 31,512 [6], imputed from the UK long term care cost adjusting for differences in the health care price levels) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 50 [8] and a DXA scan costing € 41 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 4,853 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 3,179 million, € 1,329 million and € 346 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 7.1 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 2,588 million) followed by “other” (€ 1,689 million), spine (€ 153 million) and forearm fractures (€ 77 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in France. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 139,400 (Table 12). 70 % of the total QALY loss was incurred in women. Prior fractures accounted for 60 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 8.31 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 13.16 billion in France in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 24 %, 10 %, 3 %, and 63 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 22.6 million in 2010 to 27.1 million in 2025, corresponding to an increase of 20 % (Table 14).
The total number of fractures was estimated to rise from 377,000 in 2010 to 491,000 in 2025 (Table 15), corresponding to an increase of 30 %. Hip, clinical spine, forearm and other fractures increased by 24,500, 17,200, 12,900 and 60,000 respectively. The increase in the number of fractures ranged from 23 % to 33 %, depending on fracture site. The increase was estimated to be particularly marked in men (36 %) compared to women (28 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 4.9 billion in 2010 to € 6.1 billion in 2025, corresponding to an increase of 26 % (Table 16). Costs incurred in women and men increased by 23 % and 35 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 139,400 in 2010 to 167,900 in 2025, corresponding to an increase of 20 % (Table 17). The increase was estimated to be particularly marked in men (29 %) compared to women (17 %). Incident and prior fractures accounted for 61 % and 39 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 13.2 billion in 2010 to € 16.1 billion in 2025. The increase was estimated to be particularly marked in men (+31 %) compared to women (+19 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in France (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.21 % in 2001 to 7.18 % in 2008, but fell back to 6.30 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in France were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 26 % and 43 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468-89
5. Delmas PD (2006) Personal Communication.
6. Stevenson M, Davis S (2006) Analyses of the cost-effectiveness of pooled alendronate and risedronate, compared with strontium ranelate, raloxifene, etidronate and teriparatide. ScHARR: School of Health and Related Research.
7. Stevenson M, Davis S, Kanis J (2006) The hospitalization costs and outpatient costs of fragility fractures. Women’s Health Medicine 3: 149–51
8. Saraux A, Brun-Strang C, Mimaud V, Vigneron AM, Lafuma A (2007) Epidemiology, impact, management, and cost of Paget’s disease of bone in France. Joint Bone Spine 74: 90–95
9. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
10. Vidal-pro (L’information de référence sur le médicament) (2011). www.vidal.fr/
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Germany
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, K Dreinhoefer and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Karsten Dreinhoefer, Department of Muskuloskeletal Rehabilitation, Prevention and Health Service Research, Center for Sport Science and Sport Medicine (CSSB), Center for Musculoskeletal Surgery (CMSC), Charité Universitätsmedizin, Berlin; Department of Orthopedics and Traumatology, Medical Park Berlin Humboldtmühle, Berlin, Germany
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Germany
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Germany.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Germany, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Germany was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 725,000 new fragility fractures were sustained in Germany, comprising 130,000 hip fractures, 114,000 vertebral fractures, 118,000 forearm fractures and 363,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 9,008 million for the same year. Incident fractures represented 73 % of this cost, long-term fracture care 23 % and pharmacological prevention 4 %. Previous and incident fractures also accounted for 246,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 928,000 in 2025, representing an increase of 203,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 42,900, 28,000, 23,200 and 108,800, respectively. The burden of fractures in Germany in 2025 was estimated to increase by 25 % to € 11,261 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Germany in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Germany was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Germany
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 15,246,000 and 17,764,000 respectively in Germany in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 5,020,000 (Table 2). There are 29.1 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Germany [4] and are in the process of being updated [5]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 218 and 522 respectively.
The number of incident fractures in 2010 was estimated at 725,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 130,000, 114,000, 118,000 and 363,000 respectively. 67 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 2.03 % for hip and 2.35 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 670,000 and 776,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 8,777 (Table 8). Hip, vertebral and “other” fractures accounted for 4,285, 2,965 and 1,527 deaths respectively. Overall, approximately 57 % of deaths occurred in women.
Cost of osteoporosis in Germany including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long–term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
In Germany, the cost of a hip fracture and the cost of a vertebral fracture has been estimated at € 19,218 [6] and €5,585 [7], respectively. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 34,534 [8], an average of 4 long term care facilities) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 38 [9] and a DXA scan costing € 36 [10] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 9,008 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 6,617 million, € 2,055 million and € 336 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.7 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 4,251 million) followed by “other” (€ 3,625 million), spine (€ 657 million) and forearm fractures (€ 139 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Germany. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 246,300 (Table 12). 68 % of the total QALY loss was incurred in women. Prior fractures accounted for 55 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 14.93 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 23.94 billion in Germany in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 28 %, 9 %, 1 % and 62 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 33 million in 2010 to 38.5 million in 2025, corresponding to an increase of 17 % (Table 14).
The total number of fractures was estimated to rise from 725,000 in 2010 to 928,000 in 2025 (Table 15), corresponding to an increase of 28 %. Hip, clinical spine, forearm and other fractures increased by 42,900, 28,000, 23,200 and 108,800 respectively. The increase in the number of fractures ranged from 20 % to 33 %, depending on fracture site. The increase was estimated to be particularly marked in men (37 %) compared to women (24 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 9 billion in 2010 to € 11 billion in 2025, corresponding to an increase of 25 % (Table 16). Costs incurred in women and men increased by 21 % and 34 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 246,300 in 2010 to 296,800 in 2025, corresponding to an increase of 20 % (Table 17). The increase was estimated to be particularly marked in men (31 %) compared to women (16 %). Incident and prior fractures accounted for 60 % and 40 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 23.9 billion in 2010 to € 29.2 billion in 2025. The increase was estimated to be particularly marked in men (+32 %) compared to women (+17 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Germany (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.59 % in 2001 to 2.67 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Germany were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 80 % and 77 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
4. Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19: 1139–45
5. Linder R, Klein S, Hadji P, Gothe H, Verheyen F, Häussler B (2012) Bone Evaluation Study (BEST): Epidemiologie der Osteoporose in Deutschland sowie Analysen zur Inanspruchnahme von Diagnostik und Therapie. German Medical Science. Accessed January 2013 http://www.egms.de/static/en/meetings/gmds2012/12gmds165.shtml
6. Brecht JG, Kruse HP, Mohrke W, Oestreich A, Huppertz E (2004) Health-economic comparison of three recommended drugs for the treatment of osteoporosis. Int J Clin Pharmacol Res 24: 1–10
7. Brecht JG, Kruse HP, Felsenberg D, Mohrke W, Oestreich A, Huppertz E (2003) Pharmacoeconomic analysis of osteoporosis treatment with risedronate. Int J Clin Pharmacol Res 23:93–105
8. Seniorenpartner Elisabeth Schulz (2011) Alten-und Pflegeheim Wiblingen. SeniorenCentrum. Domicil. www.pflegeheim-haus-am-see.de, www.aphw.telebus.de, www.hausstiftstrasse.de, www.domicil-seniorenresidenzen.de:
9. Lordick F, Ehlken B, Ihbe-Heffinger A, Berger K, Krobot KJ, Pellissier J, Davies G, Deuson R (2007) Health outcomes and cost-effectiveness of aprepitant in outpatients receiving antiemetic prophylaxis for highly emetogenic chemotherapy in Germany. Eur J Cancer 43: 299–307
10. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
11. Rote Liste (2011). www.rote-liste.de
12. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Greece
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, GP Lyritis, P Makras and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
George P Lyritis, Hellenic Osteoporosis Foundation, Athens, Greece
Polyzois Makras, Department of Endocrinology and Diabetes, 251 Hellenic Air Force General Hospital, Athens, Greece
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Greece
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Greece.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Greece, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Greece was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 86,000 new fragility fractures were sustained in Greece, comprising 15,000 hip fractures, 13,000 vertebral fractures, 15,000 forearm fractures and 43,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 680 million for the same year. Incident fractures represented 72 % of this cost, long-term fracture care 15 % and pharmacological prevention 13 %. Previous and incident fractures also accounted for 31,000 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 107,000 in 2025, representing an increase of 21,000 fractures. Hip, clinical spine, forearm and other fractures were estimated to increase by 4,100, 3,000, 2,800 and 11,300, respectively. The burden of fractures in Greece in 2025 was estimated to increase by 20 % to € 814 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap in women and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Greece in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Greece was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Greece
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,959,000 and 2,277,000 respectively in Greece in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at c. 640,000 (Table 2). There are 37.5 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3] and have been recently updated [4]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Greece [6] which has very recently been updated [7]. We used the earlier report which was available at the time of writing [6]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 213 and 494 respectively.
The number of incident fractures in 2010 was estimated at 86,000 (Table 4). Incident hip, clinical vertebral, forearm and “other” fractures were estimated at 15,000, 13,000, 15,000 and 43,000 respectively. 64 % of fractures occurred in women.
In the population aged 50 years or more, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 2.06 % for hip and 2.40 % for vertebral fractures. The estimated proportions of men and women with prior hip and clinical vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 87,000 and 102,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,128 (Table 8). Hip, vertebral and “other” fractures accounted for 566, 352 and 210 deaths respectively. Overall, approximately 54 % of deaths occurred in women.
Cost of osteoporosis in Greece including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As from March 2012 the Greek National Health System reimburses € 470 (2 days admission) for a hip fracture treated with osteosynthesis and € 1,463 (7 days admission) for a hip fracture treated by hemiarthroplasty. More than 90 % of all hip fractures are treated surgically, usually by hemiarthroplasty. Specific data for the cost of a hip fracture was not available for Greece before 2012, and the cost of hip fracture was estimated at € 12,550 using information from Italy [8]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 13,271 [9, 10], based on Bulgarian cost of nursing home, purchasing power parity adjusted) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, since patients can be followed either in a private or in a public setting, it was assumed that patients on treatment made an annual physician visit costing € 8 [11] and a DXA scan at two sites costing € 115 [12] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 680 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 488 million, € 102 million and € 91 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 13.4 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 260 million) followed by “other” (€ 284 million), spine (€ 34 million) and forearm fractures (€ 11 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Greece. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 31,000 (Table 12). 66 % of the total QALY loss was incurred in women. Prior fractures accounted for 58 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 1.26 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 1.94 billion in Greece in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 25 %, 5 %, 5 % and 65 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 4.2 million in 2010 to 5.1 million in 2025, corresponding to an increase of 20 % (Table 14).
The total number of fractures was estimated to rise from 86,000 in 2010 to 107,000 in 2025 (Table 15), corresponding to an increase of 24 %. Hip, clinical spine, forearm and other fractures increased by 4,100, 3,000, 2,800 and 11,300 respectively. The increase in the number of fractures ranged from 19 % to 28 %, depending on fracture site. The increase was estimated to be particularly marked in men (28 %) compared to women (23 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 680 million in 2010 to € 814 million in 2025, corresponding to an increase of 20 % (Table 16). Costs incurred in women and men increased by 18 % and 24 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 31,000 in 2010 to 35,200 in 2025, corresponding to an increase of 14 % (Table 17). The increase was estimated to be particularly marked in men (21 %) compared to women (10 %). Incident and prior fractures accounted for about 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 1.9 billion in 2010 to € 2.2 billion in 2025. The increase was estimated to be particularly marked in men (+22 %) compared to women (+13 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Greece (defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.67 % in 2001 to 9.1 % in 2009 but subsequently decreased to 8.2 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Greece were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. For men, the data indicate that the volume of sold osteoporosis drugs would be sufficient to cover treatment for more patients than the number that fall above the fracture threshold. It should be noted, however, that the results from this analysis should be interpreted with some caution since it has been assumed that the distribution of drug use between genders observed in Sweden is valid for all countries. The treatment gap in men and women were estimated at −25 % and 31 % respectively (Table 19). Also note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis J (2011) personal communication, data on file.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Makras P, Vaiopoulos G, Lyritis GP; Greek National Medicine Agency (2012) 2011 guidelines for the diagnosis and treatment of osteoporosis in Greece. J Musculoskelet Neuronal Interact. 12(1):38–42.
5. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
6. Paspati I, Galanos A, Lyritis GP (1998) Hip fracture epidemiology in Greece during 1977–1992. Calcif Tissue Int 62: 542–47
7. Lyritis GP, Rizou S, Galanos A, Makras P (2013) Incidence of hip fractures in Greece during a 30-year period: 1977–2007. Osteoporos Int 24: 1579–85
8. Visentin P, Ciravegna R, Fabris F (1997) Estimating the cost per avoided hip fracture by osteoporosis treatment in Italy. Maturitas 26: 185–92
9. Nursing homes (2011) Personal communication—average of three Bulgarian nursing homes (750, 650, and 550 lev/month).
10. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
11. IKA Social Insurance Instiute G (2011). Accessed July: http://www.ika.gr/
12. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
13. (2011) Hellenic Association of Pharmaceutical Companies, SFEE. Accessed July: www.sfee.gr
14. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retreived in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Hungary
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson P Lakatos, L Szekeres, I Marton, K Zalatnai and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Peter Lakatos, 1st Department of Medicine, Semmelweis University Medical School, Budapest, Hungary
Laszlo Szekeres, Országos Reumatológiai és Fizioterápiás Intézet (ORFI), Budapest, Hungary
Istvan Marton, Rozsakert Medical Center and Hungarian Society for Osteoporosis and Osteoarthrology, Budapest, Hungary
Klára Zalatnai, Hungarian Osteoporosis Patient Association, Budapest, Hungary.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Hungary
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Hungary.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Hungary, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Hungary was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 102,000 new fragility fractures were sustained in Hungary, comprising 13,000 hip fractures, 11,000 vertebral fractures, 39,000 forearm fractures and 38,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 197 million for the same year. Incident fractures represented 64 % of this cost, long-term fracture care 15 % and pharmacological prevention 20 %. Previous and incident fractures also accounted for 23,700 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 116,000 in 2025, representing an increase of 13,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 2,900, 1,700, 2,700 and 6,000, respectively. The burden of fractures in Hungary in 2025 was estimated to increase by 15 % to € 226 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Hungary in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Hungary was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Hungary
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,540,000 and 2,143,000 respectively in Hungary in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 550,000 (Table 2). There are 6 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence and forearm incidence are available for Hungary [5]. Given that country specific incidence of the vertebral and “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 274.1 and 560.6 respectively.
The number of incident fractures in 2010 was estimated at 102,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 13,000, 11,000, 39,000 and 38,000 respectively. 67 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.55 % for hip and 1.65 % for vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 57,000 and 61,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,241 (Table 8). Hip, vertebral and “other” fractures accounted for 592, 460 and 189 deaths respectively. Overall, approximately 51 % of deaths occurred in women.
Cost of osteoporosis in Hungary including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture was not available specifically for Hungary, therefore the hip fracture cost was estimated at € 3,594 based on the cost in Slovenia [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 5,789 [7]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 43 (approximated by adjusting Romanian cost for health adjusted price levels [8]) and a DXA scan costing € 7 [7] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 197 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 127 million, € 30 million and € 40 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 20.3 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 71 million) followed by “other” (€ 69 million), forearm (€ 9 million) and spine fractures (€ 8 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost (%) by fracture site in Hungary. Note that costs for fracture prevention therapy and monitoring are not included
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 23,700 (Table 12). 68 % of the total QALY loss was incurred in women. Prior fractures accounted for 48 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 460 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 660 million in Hungary in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 19 %, 5 %, 6 % and 70 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 3.7 million in 2010 to 3.9 million in 2025, corresponding to an increase of 5 % (Table 14).
The total number of fractures was estimated to rise from 102,000 in 2010 to 116,000 in 2025 (Table 15), corresponding to an increase of 13 %. Hip, clinical spine, forearm and other fractures increased by 2,900, 1,700, 2,700 and 6,000 respectively. The increase in the number of fractures ranged from 7 % to 22 %, depending on fracture site. The increase was estimated to be 11 % in men and 14 % in women.
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 197 million in 2010 to € 226 million in 2025, corresponding to an increase of 15 % (Table 16). Costs incurred in women and men increased by 15 % and 14 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 23,700 in 2010 to 26,200 in 2025, corresponding to an increase of 11 % (Table 17). The increase was estimated to be 12 % in men and 11 % in women. Incident and prior fractures accounted for 71 % and 29 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 660 million in 2010 to € 740 million in 2025. The increase was estimated to be 12 % in both men and women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Hungary (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.97 % in 2001 to 7.6 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Hungary were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 41 % and 28 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk. Notwithstanding, there is some evidence that hip fracture rates are declining in Hungary, a phenomenon attributed to pharmaceutical treatment [11].
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468-89
5. Pentek M, Horvath C, Boncz I, Falusi Z, Toth E, Sebestyen A, Majer I, Brodszky V, Gulacsi L (2008) Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999–2003. Osteoporos Int 19: 243–49
6. Dzajkovska B, Wertheimer AI, Mrhar A (2007) The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29: 404–11
7. Freyler P, Hungarian National Health Insurance Fund OEP (2011) Personal communication.
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. Common European Drug Database (2011). Accessed June 2012: www.cedd.oep.hu,
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
11. Lakatos P, Tóth E, Szekeres L, Poór Gy, Héjj G, Takács I (2012) A csontritkulás kezelésének hatékonysága Magyarországon. Az Országos Egészségbiztosítási Pénztár adatainak elemzése [Efficiency of osteoporosis treatment in Hungary—An analysis of the Hungarian Insurance Company’s data] Lam Kid 2: 5–12.
Epidemiology and Economic Burden of Osteoporosis in Ireland
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, M O’Brien and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Michele O'Brien, The Irish Osteoporosis Society, Dublin, Ireland
John A Kanis,WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Ireland
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Ireland.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Ireland, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Ireland was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 18,000 new fragility fractures were sustained in Ireland, comprising 3,200 hip fractures, 2,700 vertebral fractures, 3,000 forearm fractures and 9,200 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 223 million for the same year. Incident fractures represented 56 % of this cost, long-term fracture care 28 % and pharmacological prevention 16 %. Previous and incident fractures also accounted for 6,100 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 28,000 in 2025, representing an increase of 9,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 1,800, 1,400, 1,400 and 4,900, respectively. The burden of fractures in Ireland in 2025 was estimated to increase by 44 % to € 320 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Ireland in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Ireland was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Ireland
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 599,000 and 647,000 respectively in Ireland in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 170,000 (Table 2). There are 10 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Ireland [5]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 167 and 488 respectively.
The number of incident fractures in 2010 was estimated at 18,000 (Table 4). Incident hip, clinical spine and forearm fractures were each estimated at 3 000, and “other” fractures were estimated at 9,000. 66 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.38 % for hip and 1.50 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 17,000 and 19,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 209 (Table 8). Hip, vertebral and “other” fractures accounted for 104, 68 and 38 deaths respectively. Overall, approximately 53 % of deaths occurred in women.
Cost of osteoporosis in Ireland including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 15,230 in Ireland based on first year hospital costs [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 39,073 [7,8], based on purchasing power parity adjusted UK cost of public nursing home) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 46 [9] and a DXA scan costing € 99 [10] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 223 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 125 million, € 62 million and € 35 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 15.8 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 105 million) followed by “other” (€ 72 million), spine (€ 8 million) and forearm fractures (€ 3 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Ireland. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 6,100 (Table 12). 68 % of the total QALY loss was incurred in women. Prior fractures accounted for 56 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 430 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 650 million in Ireland in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 19 %, 10 %, 5 % and 66 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 1.2 million in 2010 to 1.8 million in 2025, corresponding to an increase of 42 % (Table 14).
The total number of fractures was estimated to rise from 18,000 in 2010 to 28,000 in 2025 (Table 15), corresponding to an increase of 53 %. Hip, clinical spine, forearm and other fractures increased by 1,800, 1,400, 1,400 and 4,900 respectively. The increase in the number of fractures ranged from 47 % to 56 %, depending on fracture site. The increase was estimated to be 57 % in men and 50 % in women.
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 223 million in 2010 to € 320 million in 2025, corresponding to an increase of 44 % (Table 16). Costs incurred in women and men increased by 40 % and 52 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 6,100 in 2010 to 8,200 in 2025, corresponding to an increase of 34 % (Table 17). The increase was estimated to be particularly marked in men (46 %) compared to women (29 %). Incident and prior fractures accounted for 68 % and 32 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 650 million in 2010 to € 890 million in 2025. The increase was estimated to be particularly marked in men (+48 %) compared to women (+33 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Ireland (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.57 % in 2001 to 8.56 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Ireland were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 20 % and 26 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. Irish Osteoporosis Society (2011) Guidelines. www.irishosteoporosis.ie/images/uploads/Osteoporosis-Guidelines.pdf
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Dodds MK, Codd MB, Looney A, Mulhall KJ (2009) Incidence of hip fracture in the Republic of Ireland and future projections: a population-based study. Osteoporos Int 20: 2105–10
6. Azhar A, Lim C, Kelly E, O’Rourke K, Dudeney S, Hurson B, Quinlan W (2008) Cost induced by hip fractures. Ir Med J 101: 213–15
7. Stevenson M, Davis S (2006) Analyses of the cost-effectiveness of pooled alendronate and risedronate, compared with strontium ranelate, raloxifene, etidronate and teriparatide. School of Health and Related Research, University of Sheffield. Sheffield
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. Gillespie P, O’Shea E, Murphy AW, Byrne MC, Byrne M, Smith SM, Cupples ME (2010) The cost-effectiveness of the SPHERE intervention for the secondary prevention of coronary heart disease. Int J Technol Assess Health Care 26: 263–71
10. Irish Osteoporosis Society (2011). Communication with Michele O’Brien in August 2011: www.irishosteoporosis.ie
11. Common European Drug Database (2011). Accessed June 2011: www.cedd.oep.hu,
12. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Italy
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
A Svedbom, E Hernlund, M Ivergård, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, M L Brandi, F Silveri, M Rossini and JA Kanis
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Maria Luisa Brandi, Department of Internal Medicine, University of Florence, Florence Italy
Ferdinando Silveri, Department of Rheumatology, Università Politecnica delle Marche, Ancona, Italy; Italian Federation of Osteoporosis and Diseases of the Skeleton (FEDIOS)
Maurizio Rossini, Department of Rheumatology, Università di Verona, Verona, Italy; Italian Federation of Osteoporosis and Diseases of the Skeleton (FEDIOS)
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Italy
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Italy.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Italy, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Italy was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 465,000 new fragility fractures were sustained in Italy, comprising 91,000 hip fractures, 71,000 clinical vertebral fractures, 72,000 forearm fractures and 232,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 7,032 million for the same year. Incident fractures represented 61 % of this cost, long-term fracture care 34 % and pharmacological prevention 5 %. Previous and incident fractures also accounted for 171,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 598,000 in 2025, representing an increase of 132,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 27,900, 18,800, 15,400 and 70,300, respectively. The burden of fractures in Italy in 2025 was estimated to increase by 23 % to € 8,644 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Italy in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Italy was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Italy
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 10,791,000 and 12,997,000 respectively in Italy in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 3,790,000 (Table 2). There are 18.6 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Italy [5]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 189.5 and 498.4 respectively.
The number of incident fractures in 2010 was estimated at 465,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 91,000, 71,000, 72,000 and 232,000 respectively. 69 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 2.17 % for hip and 2.27 % for vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 517,000 and 539,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 5,476 (Table 8). Hip, vertebral and “other” fractures accounted for 2,778, 1,659 and 1,039 deaths respectively. Overall, approximately 53 % of deaths occurred in women.
Cost of osteoporosis in Italy including and excluding value of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”), and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
Total first year costs after fracture were imputed by applying the inpatient cost for Italy to the ratio of inpatient cost to total first year costs observed in Sweden, resulting in an estimated total first year hip fracture cost of € 19,602. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 50,202 [6]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 50 [7] and a DXA scan costing € 81 [8] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 7,032 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 4,269 million, € 2,402 million and € 361 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 5.1 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 3,977 million) followed by “other” (€ 2,324 million), spine (€ 284 million) and forearm fractures (€ 86 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share of fracture cost by fracture site in Italy. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 171,300 (Table 12). 70 % of the total QALY loss was incurred in women. Prior fractures accounted for 59 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 8.77 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 15.8 billion in Italy in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 27 %, 15 %, 2 % and 56 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 23.8 million in 2010 to 29.2 million in 2025, corresponding to an increase of 23 % (Table 14).
The total number of fractures was estimated to rise from 465,000 in 2010 to 598,000 in 2025 (Table 15), corresponding to an increase of 28 %. Hip, clinical spine, forearm and other fractures increased by 27,900, 18,800, 15,400 and 70,300 respectively. The increase in the number of fractures ranged from 21 % to 31 %, depending on fracture site. The increase was estimated to be particularly marked in men (37 %) compared to women (24 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 7 billion in 2010 to € 8.6 billion in 2025, corresponding to an increase of 23 % (Table 16). Costs incurred in women and men increased by 20 % and 31 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 171,300 in 2010 to 205,100 in 2025, corresponding to an increase of 20 % (Table 17). The increase was estimated to be particularly marked in men (28 %) compared to women (16 %). Incident and prior fractures accounted for 59 % and 41 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 15.8 billion in 2010 to € 19.1 billion in 2025. The increase was estimated to be particularly marked in men (+29 %) compared to women (+18 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Italy (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.03 % in 2001 to 5.2 % in 2010 but subsequently decreased to 5.14 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Italy were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 30 % and 59 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Piscitelli P, Brandi ML, Chitano G, Johannson H, Kanis JA, Black DM (2013) Updated fracture incidence rates for the Italian version of FRAX®. Osteoporos Int 24:859–66
6. Visentin P, Ciravegna R, Fabris F (1997) Estimating the cost per avoided hip fracture by osteoporosis treatment in Italy. Maturitas 26: 185–92
7. Capri S, Perlini S (2005) Cost-effectiveness in Italy of preventive treatment with ramipril in patients at high risk of cardiovascular events. Curr Med Res Opin 21: 913–21
8. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
9. Agenzia Italiana del Farmco (2011). www.agenziafarmaco.it
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Latvia
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson I Rasa, I Pavlina, S Berza and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Ingvars Rasa, Latvian Osteoporosis and Bone Metabolic Diseases Association, Rīga Stradiņš University, Riga East Clinical University Hospital, Riga, Latvia
Inese Pavliņa, Latvian Osteoporosis and Bone Metabolic Diseases Association, Riga East Clinical University Hospital, Riga, Latvia
Santa Berza, Riga Business School, Riga Technical University, Riga, Latvia
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Latvia
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Latvia.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Latvia, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Latvia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 14,000 new fragility fractures were sustained in Latvia, comprising 3,000 hip fractures, 2,000 vertebral fractures, 2,000 forearm fractures and 7,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 38 million for the same year. Incident fractures represented 78 % of this cost, long-term fracture care 17 % and pharmacological prevention 5 %. Previous and incident fractures also accounted for 4,500 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 16,000 in 2025, representing an increase of 2,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 500, 300, 100 and 1,100, respectively. The burden of fractures in Latvia in 2025 was estimated to increase by 13 % to € 43 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Latvia in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Latvia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Latvia
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 313,000 and 499,000 respectively in Latvia in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 130,000 (Table 2). There are 4.9 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model for the assessment of fracture risk is not available for Latvia.
Incidence data was not available for Latvia, therefore data for hip fractures was imputed from Finnish age-standardized incidence rates [5]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 238.0 and 440.0 respectively.
The number of incident fractures in 2010 was estimated at 14,300 (Table 4). Incident hip, clinical spine, forearm and other fractures were estimated at 2,600, 2,300, 2,400 and 7,000 respectively. 69 % of fractures occurred in women. The number of hip fractures is close to recent but unpublished estimates [6].
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.46 % for hip and 1.43 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 12,000 and 12,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 241 (Table 8). Hip, vertebral and other fractures accounted for 116, 92 and 33 deaths respectively. Overall, approximately 56 % of deaths occurred in women.
Cost of osteoporosis in Latvia including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As the cost of a hip fracture was not available in Latvia, the cost of a hip fracture has been estimated at € 4,522 in Latvia based on the cost in Finland [7]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 6,169 [8], average for all municipalities and other organizations administering adult social care centers) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing at € 9 [9] and a DXA scan at € 18 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 38 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 29 million, € 7 million and € 2 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 5.0 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 17 million) followed by other (€ 17 million), spine (€ 2 million) and forearm fractures (€ 1 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig.1 Share (%) of fracture cost by fracture site in Latvia. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 4,500 (Table 12). 73 % of the total QALY loss was incurred in women. Prior fractures accounted for 51 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 72 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 110 million in Latvia in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 27 %, 6 %, 2 % and 66 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase modestly from 0.81 million in 2010 to 0.84 million in 2025, corresponding to an increase of 4 % (Table 14).
The total number of fractures was estimated to rise from 14,000 in 2010 to 16,000 in 2025 (Table 15), corresponding to an increase of 13 %. Hip, clinical spine, forearm and other fractures increased by 500, 300, 100 and 1,100 respectively. The increase in the number of fractures ranged from 5 % to 18 %, depending on fracture site. The increase was estimated to be particularly marked in men (20 %) compared to women (10 %).
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 38 million in 2010 to € 43 million in 2025, corresponding to an increase of 13 % (Table 16). Costs incurred in women and men increased by 10 % and 18 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 4,500 in 2010 to 5,000 in 2025, corresponding to an increase of 11 % (Table 17). The increase was estimated to be particularly marked in men (17 %) compared to women (9 %). Incident and prior fractures accounted for 58 % and 42 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 110 million in 2010 to € 123 million in 2025. The increase was estimated to be particularly marked in men (+17 %) compared to women (+9 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Latvia (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.06 % in 2001 to 2.12 % in 2008 but subsequently decreased to 1.5 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Latvia were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 93 % and 85 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. Latvian Osteoporosis and Metabolic Diseases Association (2012) Osteporosis Clinical Guidelines [Osteoporozes klīniskās vadlīnijas]. Nacionālais veselības dienests. Accessed Jan 2013 http://www.vmnvd.gov.lv/lv/420-kliniskas-vadlinijas/klinisko-vadliniju-datu-baze/registretas-2012gada
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Kroger H (2011) Personal communication.
6. Rasa I (2012) Personal communication.
7. Nurmi I, Narinen A, Luthje P, Tanninen S (2003) Cost analysis of hip fracture treatment among the elderly for the public health services: a 1-year prospective study in 106 consecutive patients. Arch Orthop Trauma Surg 123: 551–54
8. Latvia Ministry (2011) Latvijas Republikas—Labklajibas Ministrija. www.lm.gov.lv/index.php
9. Health Payment Center in Latvia (VNC) (2011) communication with Toms Noviks August, 2011. http://www.vnc.gov.lv/
10. Common European Drug Database (2011). Accessed June: www.cedd.oep.hu,
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Lithuania
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, V Alekna, M Tamulaitiene, and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Vidmantas Alekna, Lithuanian Osteoporosis Foundation, Vilnius, Lithuania and Vilnius University, Vilnius, Lithuania
Marija Tamulaitiene, Lithuanian Osteoporosis Foundation, Vilnius, Lithuania and Vilnius University, Vilnius, Lithuania
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Lithuania
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Lithuania.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Lithuania, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Lithuania was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 15,000 new fragility fractures were sustained in Lithuania, comprising 3,000 hip fractures, 2,000 vertebral fractures, 3,000 forearm fractures and 7,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 47 million for the same year. Incident fractures represented 68 % of this cost, long-term fracture care 26 % and pharmacological prevention 6 %. Previous and incident fractures also accounted for 4,900 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 17,000 in 2025, representing an increase of 2,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 500, 300, 300 and 1,300, respectively. The burden of fractures in Lithuania in 2025 was estimated to increase by 14 % to € 54 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Lithuania in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Lithuania was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Lithuania
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 442,000 and 685,000 respectively in Lithuania in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 180,000 (Table 2). There are 2.4 DXA scan machines per million (m) inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
At the time of writing the report, national data on the incidence of fracture was not available for Lithuania, therefore data for hip fractures was imputed from Polish age–standardized incidence rates [5]. Since then, data have become available from Vilnius [6]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 166.5 and 333.2 respectively.
The number of incident fractures in 2010 was estimated at 15,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 2,600, 2,400, 2,500 and 7,500 respectively. 67 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.16 % for hip and 1.13 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and clinical vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 13,000 and 13,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 244 (Table 8). Hip, vertebral and “other” fractures accounted for 114, 98 and 32 deaths respectively. Overall, approximately 52 % of deaths occurred in women.
Cost of osteoporosis in Lithuania including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 4,810 based on Finnish costs [7]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 10,691 [8]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 3 [9] and a DXA scan costing € 28 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 47 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 32 million, € 12 million and € 3 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 5.5 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 23 million) followed by “other” (€ 18 million), spine (€ 2 million) and forearm fractures (€ 1 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Lithuania. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 4,900 (Table 12). 70 % of the total QALY loss was incurred in women. Prior fractures accounted for 52 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 80 m.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 130 million in Lithuania in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 25 %, 9 %, 2 % and 63 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 1.1 million in 2010 to 1.2 million in 2025, corresponding to an increase of 8 % (Table 14).
The total number of fractures was estimated to rise from 15,000 in 2010 to 17,000 in 2025 (Table 15), corresponding to an increase of 16 %. Hip, clinical spine, forearm and other fractures increased by 500, 300, 300 and 1,300 respectively. The increase in the number of fractures ranged from 11 % to 19 %, depending on fracture site. The increase was estimated to be 16 % in both men and women.
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 47 million in 2010 to € 54 million in 2025, corresponding to an increase of 15 % (Table 16). Costs incurred in women and men increased by 15 % and 13 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 4,900 in 2010 to 5,500 in 2025, corresponding to an increase of 13 % (Table 17). The increase was estimated to be 12 % in men and 13 % in women. Incident and prior fractures accounted for 57 % and 43 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 128 million in 2010 to € 145 million in 2025. The increase was estimated to be 12 % in men and 14 % in women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Lithuania (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.4 % in 2001 to 1.38 % in 2008 but subsequently decreased to 1.21 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Lithuania were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 95 % and 90 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Czerwinski E, Lorenc R (2011) Personal communication.
6. Tamulaitiene M and Alekna V (2012) Incidence and direct hospitalisation costs of hipfractures in Vilnius, capital of Lithuania, in 2010. BMC Public Health 12: 495–503
7. Nurmi I, Narinen A, Luthje P, Tanninen S (2003) Cost analysis of hip fracture treatment among the elderly for the public health services: a 1-year prospective study in 106 consecutive patients. Arch Orthop Trauma Surg 123: 551–54
8. Republic of Lithuania—Ministry of Health (2011) Kauno Territorial Health Insurance Fund. Accessed June 2011 www.sam.lt/index.php?3474664842
9. Republic of Lithuania—Ministry of Health (2011) Lithuanian National Health Insurance Fund under the Ministry of Health. www.vlk.lt
10. Common European Drug Database (2011). Accessed June: www.cedd.oep.hu,
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Luxembourg
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, M Hirsch and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Marco Hirsch, Department of Rheumatology, Zithaklinik, Luxembourg
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Luxembourg
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Luxembourg.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Luxembourg, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Luxembourg was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 2,700 new fragility fractures were sustained in Luxembourg, comprising 470 hip fractures, 410 vertebral fractures, 460 forearm fractures and 1,400 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 22 million for the same year. Incident fractures represented 71 % of this cost, long-term fracture care 20 % and pharmacological prevention 9 %. Previous and incident fractures also accounted for 900 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 4,000 in 2025, representing an increase of 1,300 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 240, 200, 180 and 700, respectively. The burden of fractures in Luxembourg in 2025 was estimated to increase by 41 % to € 31 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap in women and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Luxembourg in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Luxembourg was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Luxembourg
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 75,000 and 83,000 respectively in Luxembourg in 2010 (Table 1). It should be noted that this includes a substantial proportion of French, Belgian and German nationals.
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 22,000 (Table 2). There are 2 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model for the assessment of fracture risk is not available for Luxembourg.
Incidence data was not available for Luxembourg, therefore data for hip fractures was imputed from Belgian age-standardized incidence rates [5]. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 228.5 and 538.7 respectively.
The number of incident fractures in 2010 was estimated at 2,700 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 470, 400, 460 and 1,400 respectively. 66 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportions of individuals who had suffered a fracture prior to 2010 were estimated at 1.55 % for hip and 1.77 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 2,400 and 2,800 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 28 (Table 8). Hip, vertebral and “other” fractures accounted for 14, 10 and 4 deaths respectively. Overall, approximately 56 % of deaths occurred in women.
Cost of osteoporosis in Luxembourg including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture was not available specifically for Luxembourg, therefore hip fracture costs has been estimated at € 12,616 based on Belgian costs [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 19,787 [7,8], based on Belgian cost of public nursing home) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 30 [9] and a DXA scan at € 59 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 22 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 15 million, € 4 million and € 2 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 9.1 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 10 million) followed by “other” (€ 9 million), spine (€ 1 million) and forearm fractures (€ 0.4 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Luxembourg. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 900 (Table 12). 67 % of the total QALY loss was incurred in women. Prior fractures accounted for 55 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 150 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 170 million in Luxembourg in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 9 %, 3 %, 1 % and 87 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 158,000 in 2010 to 220,000 in 2025, corresponding to an increase of 39 % (Table 14).
The total number of fractures was estimated to rise from approximately 2,700 in 2010 to 4,000 in 2025 (Table 15), corresponding to an increase of 49 %. Hip, clinical spine, forearm and other fractures increased by 200, 200, 200 and 700 respectively. The increase in the number of fractures ranged from 40 % to 52 %, depending on fracture site. The increase was estimated to be particularly marked in men (66 %) compared to women (41 %).
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 22 million in 2010 to € 31 million in 2025, corresponding to an increase of 41 % (Table 16). Costs incurred in women and men increased by 33 % and 59 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 900 in 2010 to 1,200 in 2025, corresponding to an increase of 30 % (Table 17). The increase was estimated to be particularly marked in men (48 %) compared to women (21 %). Incident and prior fractures accounted for 75 % and 25 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 170 million in 2010 to € 220 million in 2025. The increase was estimated to be particularly marked in men (+49 %) compared to women (+23 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Luxembourg (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 4.65 % in 2001 to 8.25 % in 2006 but subsequently decreased to 5.78 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Luxembourg were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. For men, the data indicate that the volume of sold osteoporosis drugs would be sufficient to cover treatment for more patients than the number that fall above the fracture threshold. It should be noted, however, that the results from this analysis should be interpreted with some caution since it has been assumed that the distribution of drug use between genders observed in Sweden is valid for all countries. The treatment gaps in men and women were estimated at −35 % and 43 % respectively (Table 19). Also note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk. This has been shown not to be the case [11].
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. Conseil scientifique, Domaine de la Santé, Analyses de laboratoire (2010) Ostéoporose. Accessed Jan 2013 http://www.conseil-scientifique.lu/index.php?id=84
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Hiligsmann M, Bruyère O, Roberfroid D et al (2012) Trends in hip fracture incidence and in the prescription of antiosteoporosis medications during the same time period in Belgium (2000–2007). Arthrit Care Res 64: 744-50.
6. Bouee S, Lafuma A, Fagnani F, Meunier PJ, Reginster JY (2006) Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 26: 1063–72
7. Autier P, Haentjens P, Bentin J, Baillon JM, Grivegnee AR, Closon MC, Boonen S (2000) Costs induced by hip fractures: a prospective controlled study in Belgium. Belgian Hip Fracture Study Group. Osteoporos Int 11: 373–80
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. Caisse Nationale de Santé Luxembourg (2011) Accessed June 2011: www.cns.lu
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
11. Hirsch M, Triki R, Marinescu R, Rolland-Portal I, Koch P (2010) Discrepancies between antiosteoporotic therapies and diagnostic intervention for osteoporosis in Luxembourg. Presentation to the Royal Belgian Society of Rheumatology.
Epidemiology and Economic Burden of Osteoporosis in Malta
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, RP Galea and JA Kanis
Emma Hernlund, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Moa Ivergård, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, Uk
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Raymond P Galea, Department of Obstetrics and Gynaecology, Mater Dei Hospital, Malta Malta
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Malta
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Malta.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Malta, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Malta was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 2,600 new fragility fractures were sustained in Malta, comprising 450 hip fractures, 430 vertebral fractures, 470 forearm fractures and 1,300 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 17 million for the same year. Incident fractures represented 65 % of this cost, long-term fracture care 24 % and pharmacological prevention 12 %. Previous and incident fractures also accounted for 800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 3,800 in 2025, representing an increase of 1,100 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 230, 190, 140 and 580, respectively. The burden of fractures in Malta in 2025 was estimated to increase by 39 % to € 24 million.
Conclusions There is a high cost of osteoporosis with a substantial projected increase of the economic burden driven by aging populations, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Malta in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Malta was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Malta
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 71,000 and 81,000 respectively in Malta in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at c. 20,000 (Table 2). There are 9.7 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Malta for the years 2003–2007 [5]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 206.1 and 502.5 respectively.
The number of incident fractures in 2010 was estimated at 2,600 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 450, 430, 470 and 1,300 respectively. 68 % of fractures occurred in women. These figures may be conservative since hip fracture rates appear to have increased recently. Thus, the annual number of hip fractures in men and women appears to have risen from approximately 450 using the source data for 2003–2007 to 550/year for the years 2009–2011 [6].
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.30 % for hip and 1.52 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 2,000 and 2,300 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 30 (Table 8). Hip, vertebral and “other” fractures accounted for 15, 11 and 4 deaths respectively. Overall, approximately 56 % of deaths occurred in women.
Cost of osteoporosis in Malta including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As the cost of a hip fracture was not available specifically for Malta, the cost of a hip fracture has been estimated at € 9,084 based on Italian costs [7]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 23,265 [7,8], approximated using the PPP adjusted Italian cost of public nursing home) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 23 [8] (approximated using the PPP adjusted Italian cost) and a DXA scan costing € 184 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 17 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 11 million, € 4 million and € 2 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 11.8 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 8 million) followed by “other” (€ 6 million), spine (€ 0.8 million) and forearm fractures (€ 0.3 million) (Table 11 and Fig. 1). As noted above, the fracture rates may be underestimated by about 20 % so that the costs may be proportionately higher. Note also that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1. Share (%) of fracture cost by fracture site in Malta. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 800 (Table 12). 70 % of the total QALY loss was incurred in women. Prior fractures accounted for 50 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 24 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 41 million in Malta in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 27 %, 10 %, 5 %, 58 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 152,000 in 2010 to 176,000 in 2025, corresponding to an increase of 16 % (Table 14).
The total number of fractures was estimated to rise from approximately 2,600 in 2010 to 3,800 in 2025 (Table 15), corresponding to an increase of 43 %. Hip, clinical spine, forearm and other fractures increased by 200, 200, 100 and 600 respectively. The increase in the number of fractures ranged from 30 % to 52 %, depending on fracture site. The increase was estimated to be particularly marked in men (58 %) compared to women (36 %).
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 17 million in 2010 to € 24 million in 2025, corresponding to an increase of 40 % (Table 16). Costs incurred in women and men increased by 33 % and 55 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 800 in 2010 to 1,100 in 2025, corresponding to an increase of 32 % (Table 17). The increase was estimated to be particularly marked in men (47 %) compared to women (25 %). Incident and prior fractures accounted for about 70 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 41 million in 2010 to € 55 million in 2025. The increase was estimated to be particularly marked in men (+50 %) compared to women (+29 %) (Table 18).
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Schembri A (2011) Personal communication.
6. Galea RP (2013) Personal communication
6. Visentin P, Ciravegna R, Fabris F (1997) Estimating the cost per avoided hip fracture by osteoporosis treatment in Italy. Maturitas 26: 185–92
7. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
8. Ministry for Health (2011) Elderly and Community Care, Malta. Mater Dei Hospital price: www.sahha.gov.mt,
9. Malta Competition and Consumer Affairs Authority (2011). Communication with Gianpiero Fava: www.msa.org.mt
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in the Netherlands
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, S Papapoulos and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
S Papapoulos, Department of Endocrinology & Metabolic Diseases, Leiden University Medical Center, Leiden, The Netherlands
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in the Netherlands
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in the Netherlands.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in the Netherlands, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the Netherlands was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 76,000 new fragility fractures were sustained in the Netherlands, comprising 13,000 hip fractures, 12,000 vertebral fractures, 12,000 forearm fractures and 38,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 824 million for the same year. Incident fractures represented 44 % of this cost, long-term fracture care 53 % and pharmacological prevention 4 %. Previous and incident fractures also accounted for 26,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 107,000 in 2025, representing an increase of 31,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 6,100, 4,800, 3,900 and 15,900, respectively. The burden of fractures in the Netherlands in 2025 was estimated to increase by 30 % to € 1,069 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in the Netherlands in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in the Netherlands was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in the Netherlands
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 2,798,000 and 3,095,000 respectively in the Netherlands in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 820,000 (Table 2). There are 10.7 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for the Netherlands [5]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 163.8 and 368.3 respectively.
The number of incident fractures in 2010 was estimated at 76,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 13,000, 12,000, 12,000 and 38,000 respectively. 64 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.27 % for hip and 1.39 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 75,000 and 82,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 870 (Table 8). Hip, vertebral and “other” fractures accounted for 431, 285 and 154 deaths respectively. Overall, approximately 50 % of deaths occurred in women.
Cost of osteoporosis in the Netherlands including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 10,458 in the Netherlands [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 63,685 [7]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 23 [8] and a DXA scan at € 84 [8] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 824 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 360 million, € 434 million and € 29 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.5 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 559 million) followed by “other” (€ 203 million), spine (€ 25 million) and forearm fractures (€ 8 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in the Netherlands. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 26,300 (Table 12). 66 % of the total QALY loss was incurred in women. Prior fractures accounted for 57 % of the total QALY loss. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 1.86 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 2.69 billion in Netherlands in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 13 %, 16 %, 1 % and 69 %, respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 5.9 million in 2010 to 7.4 million in 2025, corresponding to an increase of 26 % (Table 14).
The total number of fractures was estimated to rise from 76,000 in 2010 to 107,000 in 2025 (Table 15), corresponding to an increase of 41 %. Hip, clinical spine, forearm and other fractures increased by 6,100, 4,800, 3,900 and 15,900 respectively. The increase in the number of fractures ranged from 31 % to 45 %, depending on fracture site. The increase was estimated to be particularly marked in men (51 %) compared to women (35 %).
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 824 million in 2010 to € 1069 million in 2025, corresponding to an increase of 30 % (Table 16). Costs incurred in women and men increased by 23 % and 44 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 26,300 in 2010 to 33,800 in 2025, corresponding to an increase of 28 % (Table 17). The increase was estimated to be particularly marked in men (41 %) compared to women (22 %). Incident and prior fractures accounted for 63 % and 37 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 2.7 billion in 2010 to € 3.5 billion in 2025. The increase was estimated to be particularly marked in men (+42 %) compared to women (+22 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in the Netherlands (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 2.2 % in 2001 to 4.69 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in the Netherlands were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 52 % and 60 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. De Vries F (2009) Personal communication.
6. Jansen JP, Gaugris S, Bergman G, Sen SS (2008) Cost-effectiveness of a fixed dose combination of alendronate and cholecalciferol in the treatment and prevention of osteoporosis in the United Kingdom and The Netherlands. Curr Med Res Opin 24: 671–84
7. Meerding WJ, Mulder S, van Beeck EF (2006) Incidence and costs of injuries in The Netherlands. Eur J Public Health 16: 272–78
8. The Dutch Healthcare Authority (NZa) (2011). Accessed August: www.nza.nl
9. Health Care Insurance Board’s medicine price list (2011). Accessed August: www.medicijnkosten.nl
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Poland
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, E Czerwinski, JE Badurski,
R Lorenc, M Jaworski and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Edward Czerwinski, Department of Bone and Joint Diseases, Medical College Jagiellonian University, Krakow, Poland
Janusz E. Badurski, The Polish Foundation of Osteoporosis Research Team, Białystok, Poland.
Roman S Lorenc, Department of Biochemistry and Experimental Medicine, The Children’s Memorial Health Institute, Warsaw, Poland.
Maciej Jaworski, Department of Biochemistry, Radioimmunology and Experimental Medicine, The Children’s Memorial Health Institute, Warsaw, Poland.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Poland
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Poland.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Poland, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 168,000 new fragility fractures were sustained in Poland, comprising 28,000 hip fractures, 26,000 vertebral fractures, 28,000 forearm fractures and 85,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 593 million for the same year. Incident fractures represented 60 % of this cost, long-term fracture care 27 % and pharmacological prevention 13 %. Previous and incident fractures also accounted for 53,300 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 209,000 in 2025, representing an increase of 42,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 9,200, 6,800, 4,600 and 21,100, respectively. The burden of fractures in Poland in 2025 was estimated to increase by 27 % to € 753 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Poland in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Poland was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Poland
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 5,822,000 and 7,528,000 respectively in Poland in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria by DXA at the femoral neck [2]—was estimated at 1,850,000 (Table 2). There are 4.3 DXA scan machines per million inhabitants [3], and guidelines for the assessment and treatment of osteoporosis are available [4]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Poland [6]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 166.5 and 333.2 respectively.
The number of incident fractures in 2010 was estimated at 168,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 28,000, 26,000, 28,000 and 85,000 respectively. 61 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.04 % for hip and 1.09 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 139,000 and 145,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 2,343 (Table 8). Hip, vertebral and “other” fractures accounted for 1,083, 941 and 319 deaths respectively. Overall, approximately 49 % of deaths occurred in women.
Cost of osteoporosis in Poland including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As the cost of a hip fracture was not available specifically for Poland, hip fracture costs were estimated at € 4,881 based on data from the Czech Republic [7]. No other fracture costs were available. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 13,242 [8, 9], an average of 4 long term care facilities in Germany, PPP adjusted) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug costs (€) for individual treatments are shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 17 [10] and a DXA scan costing € 10 [11] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 593 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 355 million, € 162 million and € 76 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 12.8 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 279 million) followed by “other” (€ 204 million), spine (€ 26 million) and forearm fractures (€ 8 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Poland. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 53,300 (Table 12). Prior fractures accounted for 52 % of the total loss and 64 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 990 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 1,580 million in Poland in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 22 %, 10 %, 5 %, 63 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 13.4 million in 2010 to 14.7 million in 2025, corresponding to an increase of 10 % (Table 14).
The total number of fractures was estimated to rise from 168,000 in 2010 to 209,000 in 2025 (Table 15), corresponding to an increase of 25 %. Hip, clinical spine, forearm and other fractures increased by 9,200, 6,800, 4,600 and 21,100 respectively. The increase in the number of fractures ranged from 16 % to 33 %, depending on fracture site. The increase was estimated to be particularly marked in women (27 %) compared to men (22 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 593 million in 2010 to € 753 million in 2025, corresponding to an increase of 27 % (Table 16). Costs incurred in women and men both increased by 27 %.
The total number of QALYs lost due to fracture was estimated to rise from 53,300 in 2010 to 64,800 in 2025, corresponding to an increase of 22 % (Table 17). The increase was estimated to be 21 % in men and 22 % in women. Incident and prior fractures accounted for 57 % and 43 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 1.6 billion in 2010 to € 2.0 billion in 2025. The increase was estimated to be 23 % in men and 24 % in women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Poland (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.59 % in 2001 to 2.46 % in 2007 but subsequently decreased to 2.10 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Poland were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 91 % and 78 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42: 467–75.
3. Kanis JA (2011) Personal communication.
4. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
5. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
6. Czerwinski E, Lorenc R (2011) Personal communication.
7. Kudrna K, Krska Z (2005) Expense analysis of the proximal femoral fractures treatment. Rozhl Chir 84: 631–34
8. Seniorenpartner Elisabeth Schulz (2011) Alten-und Pflegeheim Wiblingen. SeniorenCentrum. Domicil. www.pflegeheim-haus-am-see.de, www.aphw.telebus.de, www.hausstiftstrasse.de, www.domicil-seniorenresidenzen.de:
9. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
10. Dal NR, Piskorz P, Vives R, Guilera M, Sazonov K, V, Badia X (2007) Healthcare utilisation and costs associated with adding montelukast to current therapy in patients with mild to moderate asthma and co-morbid allergic rhinitis: PRAACTICAL study. Pharmacoeconomics 25: 665–76
11. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
12. Common European Drug Database (2011). Accessed June: www.cedd.oep.hu
13. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Portugal
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, J Monteiro and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Jacinto Monteiro, Orthopaedic and Trauma Department of the University Hospital of Santa Maria, Lisbon, Portugal, Portuguese Society of Ostheoporosis and other bone metabolic diseases (SPODOM)
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Portugal
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Portugal.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Portugal, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 52,000 new fragility fractures were sustained in Portugal, comprising 10,000 hip fractures, 8,000 vertebral fractures, 8,000 forearm fractures and 26,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 577 million for the same year. Incident fractures represented 51 % of this cost, long-term fracture care 46 % and pharmacological prevention 3 %. Previous and incident fractures also accounted for 17,900 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 69,000 in 2025, representing an increase of 17,000 fractures. Hip, clinical spine (vertebral), forearm and other fractures were estimated to increase by 3,700, 2,400, 2,000 and 9,100, respectively. The burden of fractures in Portugal in 2025 was estimated to increase by 24 % to € 717 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Portugal in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Portugal was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Portugal
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,762,000 and 2,160,000 respectively in Portugal in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 590,000 (Table 2). There are 26.9 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Portugal [5]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 139.0 and 408.2 respectively.
The number of incident fractures in 2010 was estimated at 52,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 10,000, 8,000, 8,000 and 26,000 respectively. 70 % of fractures occurred in women.
In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.33 % for hip and 1.37 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 52,000 and 54,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 665 (Table 8). Hip, vertebral and “other” fractures accounted for 336, 204 and 124 deaths respectively. Overall, approximately 55 % of deaths occurred in women.
Cost of osteoporosis in Portugal including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”) and; (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 12,031 in Portugal [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 54,140 [7], based on nursing home costs in Spain) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 3 [8] and a DXA scan costing € 5 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 577 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 293 million, € 264 million and € 20 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 3.5 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 368 million) followed by “other” (€ 164 million), spine (€ 19 million) and forearm fractures (€ 6 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Portugal. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 17,900 (Table 12). Prior fractures accounted for 57 % of the total loss and 71 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 580 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 1.16 billion in Portugal in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 25 %, 23 %, 2 %, 50 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 3.9 million in 2010 to 4.8 million in 2025, corresponding to an increase of 21 % (Table 14).
The total number of fractures was estimated to rise from 52,000 in 2010 to 69,000 in 2025 (Table 15), corresponding to an increase of 33 %. Hip, clinical spine, forearm and other fractures increased by 3,700, 2,400, 2,000 and 9,100 respectively. The increase in the number of fractures ranged from 25 % to 38 %, depending on fracture site. The increase was estimated to be particularly marked in men (38 %) compared to women (31 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 577 million in 2010 to € 717 million in 2025, corresponding to an increase of 24 % (Table 16). Costs incurred in women and men increased by 22 % and 30 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 17,900 in 2010 to 21,700 in 2025, corresponding to an increase of 21 % (Table 17). The increase was estimated to be particularly marked in men (30 %) compared to women (18 %). Incident and prior fractures accounted for 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 1.2 billion in 2010 to € 1.4 billion in 2025. The increase was estimated to be particularly marked in men (+30 %) compared to women (+20 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Portugal (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 2.22 % in 2001 to 8.65 % in 2008 but subsequently decreased to 7.12 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Portugal were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 24 % and 37 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. de Pina MF, Alves SM, Barbosa M, Barros H (2008) Hip fractures cluster in space: an epidemiological analysis in Portugal. Osteoporos Int 19: 1797–804
6. ECOO Program (2011). Osteoporosis International 22: 71–89
7. Kobelt G, Berg J, Lindgren P, Izquierdo G, Sanchez-Solino O, Perez-Miranda J, Casado MA (2006) Costs and quality of life of multiple sclerosis in Spain. Eur J Health Econ 7 Suppl 2: S65–S74
8. Secretaria-Geral Ministério da Saudé Portugal (2011). Communication with Lina Freitas: http://www.sg.min-saude.pt/
9. Portal da Saudé Portugal (2011). Accessed in July: www.portaldasaude.pt
10. National Authority of Medicines and Health Products Portugal (2011). Accessed July: http://www.infarmed.pt/
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Romania
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, D Grigorie and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Daniel Grigorie, Carol Davila University of Medicine, National Institute of Endocrinology, Bucharest, Romania.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Romania
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Romania.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Romania, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 94,000 new fragility fractures were sustained in Romania, comprising 14,000 hip fractures, 16,000 vertebral fractures, 16,000 forearm fractures and 48,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 129 million for the same year. Incident fractures represented 68 % of this cost, long-term fracture care 27 % and pharmacological prevention 5 %. Previous and incident fractures also accounted for 29,700 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 110,000 in 2025, representing an increase of 16,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 3,000, 2,400, 2,300 and 8,200, respectively. The burden of fractures in Romania in 2025 was estimated to increase by 17 % to € 151 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above that received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Romania in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Romania was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Romania
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 3,212,000 and 4,077,000 respectively in Romania in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 1,030,000 (Table 2). There are 2.4 DXA scan machines per million inhabitants, and guidelines for osteoporosis treatment are available [2]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Romania [4]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 170.3 and 282.3 respectively.
The number of incident fractures in 2010 was estimated at 94,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 14,000, 16,000, 16,000 and 48,000 respectively. 56 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 0.99 % for hip and 1.14 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 72,000 and 83,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,609 (Table 8). Hip, vertebral and “other” fractures accounted for 723, 712 and 174 deaths respectively. Overall, approximately 47 % of deaths occurred in women.
Cost of osteoporosis in Romania including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As the cost of a hip fracture was not specifically available for Romania, hip fracture costs were estimated at € 2,168 based on costs in Slovenia [5]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 5,756 [6]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 26 [7] and a DXA scan reimbursed at € 5 [7] every second year to monitor treatment. In practice, the price of DXA is much higher and borne by the patient.
The cost of osteoporosis in 2010 was estimated at € 129 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 88 million, € 35 million and € 7 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 5.2 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 61 million) followed by “other” (€ 53 million), spine (€ 7 million) and forearm fractures (€ 2 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share of fracture cost (%) by fracture site in Romania. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 29,700 (Table 12). Prior fractures accounted for 51 % of the total loss and 58 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 340 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 470 million in Romania in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 19 %, 7 %, 1 %, 72 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 7.3 million in 2010 to 8.2 million in 2025, corresponding to an increase of 12 % (Table 14).
The total number of fractures was estimated to rise from 94,000 in 2010 to 110,000 in 2025 (Table 15), corresponding to an increase of 17 %. Hip, clinical spine, forearm and other fractures increased by 3,000, 2,400, 2,300 and 8,200 respectively. The increase in the number of fractures ranged from 14 % to 21 %, depending on fracture site. The increase was estimated to be 13 % in men and 20 % in women.
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 129 million in 2010 to € 151 million in 2025, corresponding to an increase of 17 % (Table 16). Costs incurred in women and men increased by 20 % and 13 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 29,700 in 2010 to 33,800 in 2025, corresponding to an increase of 14 % (Table 17). The increase was estimated to be 11 % in men and 16 % in women. Incident and prior fractures accounted for 59 % and 41 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 468 million in 2010 to € 537 million in 2025. The increase was estimated to be 12 % in men and 17 % in women (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Romania (defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 0.05 % in 2001 to 1.65 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Romania were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 94 % and 83 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Romanian Ministry of Health (2010) Guidelines for the diagnosis and treatment of postmenopausal osteoporosis. Order number 1322/2010. (www.ms.ro).
3. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
4. Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) Incidence of hip fracture in Romania and the development of a Romanian FRAX model. Calcif Tiss Int 92: 429–36
5. Dzajkovska B, Wertheimer AI, Mrhar A (2007) The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29: 404–11
6. Garaiacu A (2011) Personal communication—National Health Insurance House.
7. Casa de Asagurari de Sanatate a Municipiului Bucuresti (2011). Accessed August, 2011: http://www.casmb.ro/
8. Casa National de Asigurari de Sanatate (2011). Accessed August, 2011: http://www.cnas.ro/medicamente/lista-medicamentelor-2011
9. United Nations Department of Economic and Social Affairs–Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Slovakia
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, P Masaryk, J Payer, P Jackuliak and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Pavol Masaryk, National Institute of Rheumatic Diseases, Piestany, Slovakia, Slovak Society for Osteoporosis and Metabolic Bone Diseases
Juraj Payer, 5th Department of Internal medicine, Medical Faculty of Comenius University, Bratislava, Slovakia, Slovak Society for Osteoporosis and Metabolic Bone Diseases
Peter Jackuliak, 5th Department of Internal medicine, Medical Faculty of Comenius University, Bratislava, Slovakia, Slovak Society for Osteoporosis and Metabolic Bone Diseases.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Slovakia
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Slovakia.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Slovakia, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in Slovakia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 39,000 new fragility fractures were sustained in Slovakia, comprising 6,000 hip fractures, 6,000 vertebral fractures, 7,000 forearm fractures and 20,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 107 million for the same year. Incident fractures represented 71 % of this cost, long-term fracture care 18 % and pharmacological prevention 10 %. Previous and incident fractures also accounted for 11,700 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 50,000 in 2025, representing an increase of 11,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 2,100, 1,900, 1,600 and 5,700, respectively. The burden of fractures in Slovakia in 2025 was estimated to increase by 31 % to € 140 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by aging populations, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Slovakia in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Slovakia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Slovakia
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 755,000 and 975,000 respectively in Slovakia in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 230,000 (Table 2). There are 10.7 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on hip fracture incidence are available for Slovakia [5]. Given that country specific incidence of the vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 326 and 572 respectively.
The number of incident fractures in 2010 was estimated at 39,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 6,000, 6,000, 7,000 and 20,000 respectively. 57 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.62 % for hip and 1.88 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 28,000 and 32,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 574 (Table 8). Hip, vertebral and “other” fractures accounted for 261, 241 and 71 deaths respectively. Overall, approximately 47 % of deaths occurred in women.
Cost of osteoporosis in Slovakia including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
As the cost of a hip fracture was not available specifically for Slovakia, hip fracture costs were estimated at € 4,690 based on costs in the Czech Republic [6]. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 8,030 [7]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 16 [8] (approximated by adjusting Polish cost for health adjusted price levels) and a DXA scan costing € 32 [9] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 107 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 76 million, € 19 million and € 11 million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 10.6 % of the total cost.
When stratifying costs of osteoporosis by fracture type, other fractures were most costly (€ 45 million) followed by hip (€ 43 million), spine (€ 6 million) and forearm fractures (€ 2 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Slovakia. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 11,700 (Table 12). Prior fractures accounted for 50 % of the total loss and 60 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 280 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 390 million in Slovakia in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 20 %, 5 %, 3 %, 73 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 1.7 million in 2010 to 2.1 million in 2025, corresponding to an increase of 21 % (Table 14).
The total number of fractures was estimated to rise from 39,000 in 2010 to 50,000 in 2025 (Table 15), corresponding to an increase of 29 %. Hip, clinical spine, forearm and other fractures increased by 2,100, 1,900, 1,600 and 5,700 respectively. The increase in the number of fractures ranged from 23 % to 35 %, depending on fracture site. The increase was estimated to be the same in both men and women (29 %).
The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 107 million in 2010 to € 140 million in 2025, corresponding to an increase of 31 % (Table 16). Costs incurred in women and men increased by 30 % and 33 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 11,700 in 2010 to 14,500 in 2025, corresponding to an increase of 24 % (Table 17). The increase was estimated to be particularly marked in men (26 %) compared to women (22 %). Incident and prior fractures accounted for 64 % and 36 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 390 million in 2010 to € 490 million in 2025. The increase was estimated to be particularly marked in men (+28 %) compared to women (+24 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Slovakia (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.07 % in 2001 to 5.08 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Slovakia were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 78 % and 49 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Sensitivity Analysis
Following the analysis presented in this report, a non-indexed local language publication on the costs of osteoporotic fracture came to our attention. This suggested that we had markedly underestimated the cost of fracture [12]. We estimated the first year direct costs cost of hip, clinical spine and forearm fracture at €4,690, €1,037 and €287, respectively whereas the empirical cost was given as €15,889, €13,774 and €2,249, respectively i.e. 4 to 10 times higher than the assumptions used in the present report. Along with the inclusion of these costs, we also updated costs for pharmaceuticals [13], physician visits and DXA scans [14], and present the results as a sensitivity analysis. Except for the assumptions and costs described above, all other assumptions and costs were the same as in the base case analysis.
Fracture cost for 2010 The cost of osteoporosis in 2010 was estimated at € 352 million (Table 20). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 323 million, € 19 million and € 10 million, respectively. The total cost of €352 million exceeds the base case estimate by approximately 3-fold (see Table 10). It is notable that pharmacological fracture prevention costs amounted to only 2.9 % of the total cost.
When stratifying costs of osteoporosis by fracture type, “other fractures” were most costly (€154 million) followed by hip (€99 million), spine (€ 74 million) and forearm fractures (€ 15 million) accounting for 45 %, 29 %, 22 % and 4 % of the total cost, respectively. Note that costs for pharmacological fracture prevention are not included.
As would be expected, when the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP) the costs were substantially higher than given in the base case. The cost of osteoporosis amounted to € 636 million in Slovakia for 2010 compared with the estimate of € 390 million in the base case (see Table 13). Incident fracture, prior fracture, pharmacological intervention, and value of QALYs lost accounted for 51 %, 3 %, 2 %, and 45 % of the cost, respectively.
Fracture cost up to 2025 The cost of osteoporosis (excluding values of QALYs lost) was estimated to rise from € 352 million in 2010 to € 467 million in 2025, corresponding to an increase of 33 % (Table 21). This compared to an increase from € 107 million in 2010 to € 140 million in the base case over the same interval (see Table 16). Costs incurred in women and men increased by 32 % and 34 % respectively.
The cost of osteoporosis including the value of QALYs lost was estimated to increase from approximately € 636 million in 2010 to € 818 million in 2025. This compared to an increase from € 390 million in 2010 to € 491 million in the base case over the same interval (see Table 18). The increase was estimated to be more marked in men (+31 %) compared to women (+27 %).
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Masaryk P (2012) Hodnotenie rizika osteoporotických zlomenín v primárnej praxi (Fracture risk assessment in primary care), Rheumatologia 26: 127–133
6. Kudrna K, Krska Z (2005) Expense analysis of the proximal femoral fractures treatment. Rozhl Chir 84: 631–34
7. Seniorville Nursing Home (2011). www.seniorville.sk
8. International Bank for Reconstruction and Development/The World Bank (2008) 2005 International Comparison Program, Tables of final results.
9. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
10. Common European Drug Database (2011). Accessed June: www.cedd.oep.hu
11. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
12. Bielik J., Jureček Ľ., Hroncová D (2010) Epidemiologické a ekonomické aspekty osteoporózy. Farmakoekonomika a lieková politika 6:25–28
13. List of reimbursed drugs. Ministry of Health, Slovak Republic, 2010. www.health.gov.sk, Accessed December 2012
14. Personal communication J Payer, January 2013.
Epidemiology and Economic Burden of Osteoporosis in Slovenia
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, T Kocjan and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, , Oxford, UKUK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Tomaz Kocjan, Department of Endocrinology, Diabetes and Metabolic Diseases, University Medical Centre Ljubljana, Ljubljana, Slovenia
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Slovenia
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Slovenia.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Slovenia, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 16,000 new fragility fractures were sustained in Slovenia, comprising 3,000 hip fractures, 2,000 vertebral fractures, 2,000 forearm fractures and 8,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 56 million for the same year. Incident fractures represented 65 % of this cost, long-term fracture care 23 % and pharmacological prevention 13 %. Previous and incident fractures also accounted for 4,900 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 22,000 in 2025, representing an increase of 6,000 fractures. Hip, clinical spine, forearm and other fractures were estimated to increase by 1,400, 900, 700 and 3,400, respectively. The burden of fractures in Slovenia in 2025 was estimated to increase by 37 % to € 77 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Slovenia in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Slovenia was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Slovenia
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 343,000 and 416,000 respectively in Slovenia in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 110,000 (Table 2). There are 27.1 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model for the assessment of fracture risk is not available for Slovenia.
Detailed incidence data were not available for Slovenia, therefore data for hip fractures were imputed from Hungarian age-standardized incidence rates [5]. The incidences of vertebral, forearm and “other” fractures were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, this hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 273.8 and 558.6 respectively.
The number of incident fractures in 2010 was estimated at approximately 15,500 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 2,800, 2,300, 2,500 and 7,900 respectively. 64 % of fractures occurred in women.
In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.64 % for hip and 1.88 % for vertebral fractures. The estimated proportions of men and women with prior hip and clinical vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 12,000 and 14,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 192 (Table 8). Hip, vertebral and “other” fractures accounted for 95, 66 and 31 deaths respectively. Overall, approximately 54 % of deaths occurred in women.
Cost of osteoporosis in Slovenia including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
In Slovenia, the costs of hip, vertebral, and forearm fractures have been estimated at € 5,306, € 810, and € 161, respectively [6]. Costs for “other fractures” were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 11,308 [7]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 15 [8] and a DXA scan costing € 29 [8] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 56 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 36 million, € 13 million and € 7 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 12.5 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 26 million) followed by “other” (€ 21 million), spine (€ 2 million) and forearm fractures (€ 0.4 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Slovenia. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 4,900 (Table 12). Prior fractures accounted for 52 % of the total loss and 66 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 170 million.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 220 million in Slovenia in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 16 %, 6 %, 3 %, 75 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 760,000 in 2010 to 910,000 in 2025, corresponding to an increase of 20 % (Table 14).
The total number of fractures was estimated to rise from 16,000 in 2010 to 22,000 in 2025 (Table 15), corresponding to an increase of 41 %. Hip, clinical spine, forearm and other fractures increased by 1,400, 900, 700 and 3,400 respectively. The increase in the number of fractures ranged from 27 % to 50 %, depending on fracture site. The increase was estimated to be particularly marked in men (47 %) compared to women (37 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 56 million in 2010 to € 77 million in 2025, corresponding to an increase of 37 % (Table 16). Costs incurred in women and men increased by 32 % and 47 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 4,900 in 2010 to 6,300 in 2025, corresponding to an increase of 30 % (Table 17). The increase was estimated to be particularly marked in men (40 %) compared to women (25 %). Incident and prior fractures accounted for 65 % and 35 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 224 million in 2010 to € 296 million in 2025. The increase was estimated to be particularly marked in men (+41 %) compared to women (+27 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Slovenia (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 2.35 % in 2001 to 5.88 % in 2008 but subsequently decreased to 5.11 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Slovenia were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Given that a FRAX model for Slovenia was not available, the FRAX model for Hungary was used as a surrogate. Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 63 % and 44 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Eastern European & Central Asian Regional Audit—Individual Country Reports. www.iofbonehealth.org/publications/eastern-european-central-asian-audit-2010.html;
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Pentek M, Horvath C, Boncz I, Falusi Z, Toth E, Sebestyen A, Majer I, Brodszky V, Gulacsi L (2008) Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999–2003. Osteoporos Int 19: 243–49
6. Dzajkovska B, Wertheimer AI, Mrhar A (2007) The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29: 404–11
7. Health Insurance Institute of Slovenia (ZZZS) (2011). e-mail conversation with Maja Tomšic: www.zzzs.si
8. Health Insurance Institute of Slovenia (ZZZS) (2011). Communication with Maja Tomšic: www.zzzs.si
9. Common European Drug Database (2011). Accessed June: www.cedd.oep.hu
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Spain
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, A Diez-Perez and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, Cambridge, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Adolfo Diez-Perez, Department of Internal Medicine, Hospital del Mar-IMIM, University of Barcelona, Barcelona, Spain
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Spain
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Spain.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Spain, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 204,000 new fragility fractures were sustained in Spain, comprising 40,000 hip fractures, 30,000 vertebral fractures, 30,000 forearm fractures and 104,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 2,842 million for the same year. Incident fractures represented 48 % of this cost, long-term fracture care 37 % and pharmacological prevention 15 %. Previous and incident fractures also accounted for 70,800 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 286,000 in 2025, representing an increase of 82,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 16,700, 11,500, 10,000 and 43,500, respectively. The burden of fractures in Spain in 2025 was estimated to increase by 30 % to € 3,680 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment declined in the past few years. A substantial minority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Spain in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Spain was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Spain
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 7,277,000 and 8,628,000 respectively in Spain in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 2,450,000 (Table 2). There are 8.4 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Incidence data for hip fractures were retrieved from mean values of four regional estimates [5–8]. Given that country specific incidence of vertebral, forearm and, “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 125.9 and 353.0 respectively.
The number of incident fractures in 2010 was estimated at 204,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 40,000, 30,000, 30,000 and 104,000 respectively. 68 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.32 % for hip and 1.34 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 211,000 and 212,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 2,550 (Table 8). Hip, vertebral and “other” fractures accounted for 1,289, 719 and 542 deaths respectively. Overall, approximately 53 % of deaths occurred in women.
Cost of osteoporosis in Spain including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of a hip fracture has been estimated at € 9,421 in Spain, imputed from the UK data [9,10] by adjusting for differences in health care price levels. Given that no cost data for the other fracture sites were found, these were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 51,786 [11]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9 for 2010. For the purposes of this report drug costs were used for 2010 [12]. In addition, it was assumed that patients on treatment made an annual physician visit costing € 109 [13] and a DXA scan costing € 79 [14] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 2,842 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 1,372 million, € 1,055 million and € 414 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 14.6 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 1,591 million) followed by “other” (€ 742 million), spine (€ 63 million) and forearm fractures (€ 32 milllion) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Spain. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 70,800 (Table 12). Prior fractures accounted for 57 % of the total loss and 69 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 3.27 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 6.11 billion in Spain in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 22 %, 17 %, 7 %, 54 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 15.9 million in 2010 to 21.5 million in 2025, corresponding to an increase of 35 % (Table 14).
The total number of fractures was estimated to rise from 204,000 in 2010 to 286,000 in 2025 (Table 15), corresponding to an increase of 40 %. Hip, clinical spine, forearm and other fractures increased by 16,700, 11,500, 10,000 and 43,500 respectively. The increase in the number of fractures ranged from 34 % to 42 %, depending on fracture site. The increase was estimated to be particularly marked in men (49 %) compared to women (36 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 2.8 billion in 2010 to € 3.7 billion in 2025, corresponding to an increase of 30 % (Table 16). Costs incurred in women and men increased by 26 % and 39 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 70,800 in 2010 to 89,000 in 2025, corresponding to an increase of 26 % (Table 17). The increase was estimated to be particularly marked in men (37 %) compared to women (21 %). Incident and prior fractures accounted for 66 % and 34 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 6.1 billion in 2010 to € 7.8 billion in 2025. The increase was estimated to be particularly marked in men (+38 %) compared to women (+23 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Spain (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 2.74 % in 2001 to 9.56 % in 2009 but subsequently decreased to 8.51 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Spain were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 20 % and 25 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Elffors I, Allander E, Kanis JA, Gullberg B, Johnell O, Dequeker J, Dilsen G, Gennari C, Lopes Vaz AA, Lyritis G (1994) The variable incidence of hip fracture in southern Europe: the MEDOS Study. Osteoporos Int 4: 253–63
6. Diez A, Puig J, Martinez MT, Diez JL, Aubia J, Vivancos J (1989) Epidemiology of fractures of the proximal femur associated with osteoporosis in Barcelona, Spain. Calcif Tissue Int 44: 382–86
7. Izquierdo SM, Ochoa SC, Sanchez B, I, Hidalgo Prieto MC, Lozano d, V, Martin GT (1997) [Epidemiology of osteoporotic hip fractures in the province of Zamora (1993)]. Rev Esp Salud Publica 71: 357–67
8. Sosa M, Segarra MC, Hernandez D, Gonzalez A, Liminana JM, Betancor P (1993) Epidemiology of proximal femoral fracture in Gran Canaria (Canary Islands). Age Ageing 22: 285–88
9. Stevenson M, Davis S, Kanis J (2006) The hospitalization costs and outpatient costs of fragility fractures. Women’s Health Medicine: 149–51
10. Stevenson M, Davis S (2006) Analyses of the cost-effectiveness of pooled alendronate and risedronate, compared with strontium ranelate, raloxifene, etidronate and teriparatide.
11. Kobelt G, Berg J, Lindgren P, Izquierdo G, Sanchez-Solino O, Perez-Miranda J, Casado MA (2006) Costs and quality of life of multiple sclerosis in Spain. Eur J Health Econ 7 Suppl 2: S65–S74
12. Portal Farma (2011). www.portalfarma.com
13. Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA (2007) Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries—an economic evaluation based on the fracture intervention trial. Osteoporos Int 18: 1047–61
14. International Osteoporosis Foundation, IOF (2011) Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges.
15. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in Sweden
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson, K Åkesson and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, UK
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
Kristina Åkesson, Department of Orthopaedics, Malmo University Hospital, Malmo, Sweden.
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in Sweden
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in Sweden.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in Sweden, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the EU27 was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap.
Results It was estimated that approximately 107,000 new fragility fractures were sustained in Sweden, comprising 20,000 hip fractures, 16,000 vertebral fractures, 16,000 forearm fractures and 54,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at € 1,486 million for the same year. Incident fractures represented 62 % of this cost, long-term fracture care 36 % and pharmacological prevention 2 %. Previous and incident fractures also accounted for 36,000 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 135,000 in 2025, representing an increase of 28,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 6,100, 4,500, 3,300 and 14,400, respectively. The burden of fractures in Sweden in 2025 was estimated to increase by 23 % to € 1,828 million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 or above who received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in Sweden in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in Sweden was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in Sweden
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 1,659,000 and 1,830,000 respectively in Sweden in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 520,000 (Table 2). There are 10 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Data on incidence for all fracture types under consideration are available for Sweden [5,6]. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 318.6 and 802.8 respectively.
The number of incident fractures in 2010 was estimated at 107,000 (Table 4). Incident hip, clinical spine, forearm and “other” fractures were estimated at 20,000, 16,000, 16,000 and 54,000 respectively. 66 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 2.84 % for hip and 3.19 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 99,000 and 111,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 1,171 (Table 8). Hip, vertebral and “other” fractures accounted for 589, 362 and 220 deaths respectively. Overall, approximately 54 % of deaths occurred in women.
Cost of osteoporosis in Sweden including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) were considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
In Sweden, the costs of hip and vertebral fractures have been estimated to range from € 12,870 to € 19,667, and from €2,048 to €14,219 respectively. The cost of forearm fracture has been estimated at € 2,401 [7]. Costs for “other fractures” were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home (€ 57,247 [7]) with the simulated number of individuals with prior fractures that had been transferred to nursing home due to the fracture.
Annual drug cost (€) for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing € 130 [8] and a DXA scan costing € 152 [8] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at € 1,486 million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to € 927 million, € 529 million and € 29 million respectively. It is notable that pharmacological fracture prevention costs amounted to only 2.0 % of the total cost.
When stratifying costs of osteoporosis by fracture type, hip fractures were most costly (€ 823 million) followed by “other” (€ 421 million), spine (€ 173 million) and forearm fractures (€ 39 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in Sweden. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 36,000 (Table 12). Prior fractures accounted for 55 % of the total loss and 64 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at € 2.67 billion.
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to € 4.15 billion in Sweden in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 22 %, 13 %, 1 %, 64 % respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 3.5 million in 2010 to 4.1 million in 2025, corresponding to an increase of 18 % (Table 14).
The total number of fractures was estimated to rise from 107,000 in 2010 to 135,000 in 2025 (Table 15), corresponding to an increase of 26 %. Hip, clinical spine, forearm and other fractures increased by 6,100, 4,500, 3,300 and 14,400 respectively. The increase in the number of fractures ranged from 20 % to 30 %, depending on fracture site. The increase was estimated to be particularly marked in men (33 %) compared to women (23 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from € 1.5 billion in 2010 to € 1.8 billion in 2025, corresponding to an increase of 23 % (Table 16). Costs incurred in women and men increased by 19 % and 32 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 36,000 in 2010 to 43,300 in 2025, corresponding to an increase of 20 % (Table 17). The increase was estimated to be particularly marked in men (27 %) compared to women (16 %). Incident and prior fractures accounted for 61 % and 39 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately € 4.2 billion in 2010 to € 5 billion in 2025. The increase was estimated to be particularly marked in men (+29 %) compared to women (+17 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in Sweden (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.53 % in 2001 to 3.28 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in Sweden were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. The treatment gaps in men and women were estimated at 63 % and 72 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11: 669–74
6. Kanis Kanis JA, Oden A, Johnell O, Jonsson B, De Laet C, Dawson A, (2001) The Burden of Osteoporotic Fractures: A Method for Setting. Osteoporos Int 12: 417–27
7. Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Lunsjo K, Thorngren KG, Sernbo I, Rehnberg C, Jonsson B (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17: 637–50
8. Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA (2007) Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9. European countries—an economic evaluation based on the fracture intervention trial. Osteoporos Int 18: 1047–61
9. FASS (2009). www.fass.se
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Epidemiology and Economic Burden of Osteoporosis in the UK
A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA).
M Ivergård, A Svedbom, E Hernlund, J Compston, C Cooper, J Stenmark, EV McCloskey, B Jönsson and JA Kanis
Moa Ivergård, OptumInsight, Stockholm, Sweden
Axel Svedbom, OptumInsight, Stockholm, Sweden
Emma Hernlund, OptumInsight, Stockholm, Sweden
Juliet Compston, Department of Medicine, Addenbrooke’s Hospital, Cambridge University, UK, Cambridge,
Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton and NIHR Musculoskeletal Biomedical Research Unit, Institute of Musculoskeletal Sciences, University of Oxford, Oxford, UK
Judy Stenmark, International Osteoporosis Foundation, Nyon, Switzerland
Eugene V McCloskey, Academic Unit of Bone Metabolism, Northern General Hospital, Sheffield, UK and WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Bengt Jönsson, Stockholm School of Economics, Stockholm, Sweden
John A Kanis, WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, Sheffield, UK
Author for correspondence
Prof John A Kanis (✉) WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School,
Beech Hill Road, Sheffield S10 2RX, UK;
Tel: +44 114 285 1109;
Fax: +44 114 285 1813;
w.j.pontefract@shef.ac.uk
Running title: Burden of osteoporosis in the UK
Abstract
Summary This report describes epidemiology, burden, and treatment of osteoporosis in the UK.
Introduction Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this study is to describe the epidemiology and economic burden of fragility fractures as a consequence of osteoporosis in the UK, as a further detailed addition to the report for the entire European Union (EU27): Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden.
Methods The literature on fracture incidence and costs of fractures in the UK was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Furthermore, data on sales of osteoporosis treatments and the population at high risk were used to estimate treatment uptake and treatment gap. Costs, calculated in Euros, were converted to £ for the purpose of this report (1.00 GBP = € 1.23; 21st Dec 2012).
Results It was estimated that approximately 536,000 new fragility fractures were sustained in the UK, comprising 79,000 hip fractures, 66,000 vertebral fractures, 69,000 forearm fractures and 322,000 other fractures (i.e. fractures of the pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures) in 2010. The economic burden of incident and previous fragility fractures was estimated at £ 3,496 (€ 5,408) million for the same year. Incident fractures represented 74 % of this cost, long-term fracture care 25 % and pharmacological prevention 2 %. Previous and incident fractures also accounted for 158,700 quality-adjusted life years (QALYs) lost during 2010. When accounting for the demographic projections for 2025, the number of incident fractures was estimated at 682,000 in 2025, representing an increase of 146,000 fractures. Hip, clinical vertebral (spine), forearm and other fractures were estimated to increase by 23,000, 18,000, 15,900 and 89,300, respectively. The burden of fractures in the UK in 2025 was estimated to increase by 24 % to £ 5,465 (€ 6,723) million. Though the uptake of osteoporosis treatments increased from 2001, the proportion of patients aged 50 years or above that received treatment remained at very low levels in the past few years. The majority of women at high fracture risk did not receive active treatment.
Conclusions In spite of the high cost of osteoporosis, a substantial treatment gap in women and projected increase of the economic burden driven by an aging population, the use of pharmacological prevention of osteoporosis is significantly less than optimal, suggesting that a change in healthcare policy concerning the disease is warranted.
Introduction
Osteoporosis is characterized by reduced bone mass and disruption of bone architecture, resulting in increased risks of fragility fractures which represent the main clinical consequence of the disease. Fragility fractures are associated with substantial pain and suffering, disability and even death for the affected patients and substantial costs to society. The aim of this report was to characterize the burden of osteoporosis in the UK in 2010 and beyond.
Methods
The literature on fracture incidence and costs of fractures in the UK was reviewed and incorporated into a model estimating the clinical and economic burden of osteoporotic fractures in 2010. Details of the methods used are found in Chapters 3 and 4 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden, published concurrently in Archives of Osteoporosis.
Epidemiology of osteoporosis in the UK
For the purpose of this report, the population at risk of osteoporosis was considered to include men and women ≥50 years. The number of men and women ≥50 years of age amounted to 10,102,000 and 11,534,000 respectively in the UK in 2010 (Table 1).
In the population at risk, the number of individuals with osteoporosis—as defined by the WHO diagnostic criteria—was estimated at 3.21 million (Table 2). There are 8.2 DXA scan machines per million inhabitants [2], and guidelines for the assessment and treatment of osteoporosis are available [3]. A country specific FRAX model is also available for the assessment of fracture risk (http://www.shef.ac.uk/FRAX/).
Incidence data for hip and forearm fractures were retrieved from Singer et al. [5]. Given that country specific incidences of vertebral and “other” fractures were not found, these were imputed using the methods described in Chapter 3 of the main report. Fracture incidence is presented in Table 3. Standardized to the EU27 population, hip fracture incidence (per 100,000 person years) in men and women ≥50 years of age was estimated at 186.0 and 523.5 respectively.
The number of incident fractures in 2010 was estimated at 536,000 (Table 4). Incident hip, clinical vertebral, forearm and “other” fractures were estimated at 79,000, 66,000, 69,000 and 322,000 respectively. 64 % of fractures occurred in women.
A prior fracture was defined as a fracture in an individual who was alive during the index year (i.e. 2010) which had occurred after the age of 50 years and before 2010. In the population ≥50 years of age, the proportion of individuals who had suffered a fracture prior to 2010 was estimated at 1.94 % for hip and 2.02 % for clinical vertebral fractures. The estimated proportions of men and women with prior hip and vertebral fractures by age are presented in Table 5.
In the population over 50 years of age, the number of individuals with hip and vertebral fractures that occurred before 2010 was estimated at 419,000 and 437,000 respectively (Table 6). Note that fractures sustained in 2010 were not included in the estimate.
The incidence of causally related deaths (per 100,000) in the first year after fracture by age is presented in Table 7. The number of causally related deaths in 2010 was estimated at 6,059 (Table 8). Hip, vertebral and “other” fractures accounted for 2,764, 1,795 and 1,500 deaths respectively. Overall, approximately 54 % of deaths occurred in women.
Cost of osteoporosis in the UK including and excluding values of QALYs lost
For the purpose of this report, the cost of osteoporosis in 2010 (excluding value of QALYs lost) was considered to consist of three components: (i) cost of fractures that occurred in 2010 (“first year costs”); (ii) cost of fractures sustained prior to year 2010 but which still incurred costs in 2010 (“long-term disability cost”); and (iii) cost of pharmacological fracture prevention including administration and monitoring costs (“pharmacological fracture prevention costs”). See Chapter 4 of the main report for further details.
The cost of hip, vertebral and forearm fractures has been estimated at £ 9,390 (€ 11,055), £ 2,341 (€ 2,756), and £ 1,073 (€ 1,263) respectively [6,7]. Costs for “other fractures” were imputed as described in Chapter 4 of the main report.
Long-term disability costs were estimated by multiplying the yearly cost of residing in nursing home £24,444 (€ 33,756) [6]) with the simulated number of individuals with prior fractures that had been transferred to nursing homes due to the fracture.
Annual drug cost for individual treatments is shown in Table 9. In addition, it was assumed that patients on treatment made an annual physician visit costing £ 41 (€ 50) [8] and a DXA scan costing £ 41 (€ 51) [6] every second year to monitor treatment.
The cost of osteoporosis in 2010 was estimated at £ 4,397 (€ 5,408) million (Table 10). First year costs, subsequent year costs and pharmacological fracture prevention costs amounted to £3,233 (€ 3,977) million, £ 1,080 (€ 1,328) million and £84 (€ 103) million, respectively. It is notable that pharmacological fracture prevention costs amounted to only 1.9 % of the total cost.
When stratifying costs of osteoporosis by fracture type, “other fractures” were most costly at £2,069 million (€ 2,545 million) followed by hip fractures at £2,039 million (€ 2,508 million), vertebral fractures at £ 134 million (€ 165 million) and forearm fractures at £71 million (€ 87 million) (Table 11 and Fig. 1). Please note that costs for pharmacological fracture prevention were not included given that they cannot be allocated to specific fracture sites.

Fig. 1 Share (%) of fracture cost by fracture site in the UK. Note that costs for fracture prevention therapy and monitoring are not included.
The number of quality adjusted life years (QALYs) lost due to osteoporosis in 2010 was estimated at 158,700 (Table 12). Prior fractures accounted for 52 % of the total loss and 64 % of the loss occurred in women. The monetary value of a QALY was varied between 1 to 3 times the gross domestic product (GDP) per capita (Table 13). Assuming a QALY is valued at 2 times GDP/capita, the total cost of the QALYs lost was estimated at £7.0 billion (€ 8.7 billion).
When the cost of osteoporosis was combined with the value for QALYs lost (valued at 2 × GDP), the cost of osteoporosis amounted to £11.47 billion (€ 14.11 billion) in the UK in 2010. Incident fracture, prior fracture, pharmacological fracture prevention, and value of QALYs lost accounted for 28 %, 9 %, 1 % and 62 %, respectively.
Burden of osteoporosis up to 2025
The population above 50 years of age is expected to increase from 21.6 million in 2010 to 26.2 million in 2025, corresponding to an increase of 21 % (Table 14).
The total number of fractures was estimated to rise from 536,000 in 2010 to 682,000 in 2025 (Table 15), corresponding to an increase of 27 %. Hip, clinical vertebral, forearm and other fractures increased by 23,000, 18,000, 15,900 and 89,300 respectively. The increase in the number of fractures ranged from 23 % to 29 %, depending on fracture site. The increase was estimated to be particularly marked in men (32 %) compared to women (24 %).
The cost of osteoporosis (excluding value of QALYs lost) was estimated to rise from £ 4.4 billion (€ 5.4 billion) in 2010 to £ 5.5 billion (€ 6.7 billion) in 2025, corresponding to an increase of 24 % (Table 16). Costs incurred in women and men increased by 20 % and 32 % respectively.
The total number of QALYs lost due to fracture was estimated to rise from 158,700 in 2010 to 190,500 in 2025, corresponding to an increase of 20 % (Table 17). The increase was estimated to be particularly marked in men (27 %) compared to women (16 %). Incident and prior fractures accounted for 67 % and 33 % of the increase respectively.
The cost of osteoporosis including value of QALYs lost was estimated to increase from approximately £11.5 billion (€ 14.1 billion) in 2010 to £14.0 billion (€ 17.2 billion) in 2025. The increase was estimated to be particularly marked in men (+29 %) compared to women (+18 %) (Table 18).
Treatment uptake
To estimate uptake of individual osteoporosis treatments, sales data from IMS Health (2001–2011) were used to derive the number of defined daily doses (DDDs) sold per 100,000 persons aged 50 years or above (Fig. 2).

Fig. 2 Treatment uptake in the UK (Defined daily doses [DDDs] per 100,000 persons aged 50 years or above)
Adjusting the sales data for compliance allowed for an estimation of the proportion of population aged 50 years or above who received any osteoporosis treatment (see Chapter 5 of the report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden for further details). The proportion of persons over the age of 50 years who were treated increased from 1.11 % in 2001 to 5.5 % in 2011.
Treatment gap
In order to assess the potential treatment gap, the numbers of men and women eligible for treatment in the UK were defined as individuals with a 10-year fracture probability exceeding that of a woman with a prior fragility fracture derived from FRAX®, equivalent to a ‘fracture threshold’ (See Chapter 5 of the main report for further details). Subsequently, these estimates were compared to the number of individuals who received osteoporosis treatment obtained from the analysis of IMS Health data. For men, the data indicate that the volume of sold osteoporosis drugs would be sufficient to cover treatment for more patients than the number that fall above the fracture threshold. It should be noted, however, that the results from this analysis should be interpreted with some caution since it has been assumed that the distribution of drug use between genders observed in Sweden is valid for all countries. The treatment gaps in men and women were estimated at −34 % and 54 % respectively (Table 19). Note that the estimate of the treatment gap is conservative given that it assumes that current use of osteoporosis treatments are only directed to men and women at high risk.
Acknowledgements This report has been sponsored by an unrestricted educational grant from the European Federation of Pharmaceutical Industry Associations (EFPIA) and the International Osteoporosis Foundation (IOF). The data in this report have been used to populate a more detailed report on Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. We acknowledge the help of Helena Johansson and Prof Anders Odén for their help in the calculations of fracture probability. We thank Oskar Ström and Fredrik Borgström who were prominent authors of an earlier report covering a similar topic in a sample of EU countries and provided the template for the present report. We also thank Dr Dominique Pierroz, Carey Kyer and Ageeth Van Leersum of the IOF for their help in editing the report. The report has been reviewed by the members of the IOF EU Osteoporosis Consultation Panel and the IOF European Parliament Osteoporosis Interest Group, and we are grateful for their local insights on the management of osteoporosis in each country.
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
1. Eurostat (2011) Statistics database. Data retrieved in November, 2011: http://epp.eurostat.ec.europa.eu
2. Kanis JA (2011) Personal communication.
3. The International Osteoporosis Foundation (IOF) (2011) Osteoporosis in the European Union in 2008—Country reports. www.iofbonehealth.org/policy-advocacy/europe/eu-osteoporosis-consultation-panel/country-reports-08.html
4. Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–89
5. Singer BR, McLauchlan GJ, Robinson CM, Christie J (1998) Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br 80: 243–48
6. Stevenson M, Davis S (2006) Analyses of the cost-effectiveness of pooled alendronate and risedronate, compared with strontium ranelate, raloxifene, etidronate and teriparatide.
7. Stevenson M, Davis S, Kanis J (2006) The hospitalization costs and outpatient costs of fragility fractures. Women’s Health Medicine: 149–51
8. Curtis L (2008) Unit Costs of Health and Social Care.
9. British National Formulary (2011). http://www.bnf.org/bnf/
10. United Nations Department of Economic and Social Affairs—Population Division (2011) World Population Prospects test. Data retrieved in November, 2011: http://esa.un.org/unpd/wpp/unpp/p2k0data.asp
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
EU review panel of the IOF
Austria: HP Dimai; Belgium: M Hiligsmann, S Goemaere, J-Y Reginster; Bulgaria: A-M Borissova, M Boyanov, Z Kolarov, R Kovacheva, R Rachkov, P Popivanov, A Shinkov; Cyprus: GL Georgiades; Czech Republic: M Bayer; Denmark: B Abrahamsen; Estonia: K Maasalu; Finland: H Kröger; Germany: K Dreinhoefer; Greece: GP Lyritis, P Makras; Hungary: P Lakatos, I Marton, L Szekeres, K Zalatnai; Ireland: M O’Brien; Italy: ML Brandi, M Rossini, F Silveri; Latvia: S Berza; I Pavlina, I Rasa; Lithuania: V Alekna, M Tamulaitiene; Luxembourg: M Hirsch; Malta: RP Galea; Netherlands: S Papapoulos; Poland: JE Badurski, E Czerwinski, M Jaworski, R Lorenc; Portugal: J Monteiro; Romania: D Grigorie; Slovakia: P Jackuliak, P Masaryk, J Payer; Slovenia: T Kocjan; Spain: A Diez-Perez; Sweden: K Åkesson
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Svedbom, A., Hernlund, E., Ivergård, M. et al. Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8, 137 (2013). https://doi.org/10.1007/s11657-013-0137-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-013-0137-0