Abstract
It is generally accepted that persons infected with human immunodeficiency virus (HIV) are at an increased risk of infection due to direct destruction of CD4+ lymphocytes and subsequently impaired cell-mediated immunity. Typically, HIV infection is associated with immunoglobulin elevations, but quantitative deficiencies in immunoglobulins have also been rarely described. We present an unusual case of common variable immunodeficiency (CVID) in a HIV-positive patient with recurrent severe respiratory infections. We review epidemiology, clinical presentation, and treatment of primary immunoglobulin deficiency. We also review the relationship between immunoglobulin deficiency and HIV and highlight the importance of recognizing the coexistence of two distinct immunodeficiency syndromes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recurrent Sinopulmonary Infections in a Patient Whose HIV Masked Common Variable Immunodeficiency
CASE
A 34-year-old man with a history of HIV presented with a three-day history of recurrent dyspnea, wheezing, and unproductive cough. Three weeks prior, he had been hospitalized for respiratory failure, requiring Bi-level positive airway pressure support (BiPap), and was diagnosed with viral pneumonia and an asthma exacerbation. His HIV infection was well-controlled, with a recent CD4+ count of 537 cells/mm3, undetectable HIV RNA, and no prior opportunistic infections. Additional medical history was significant for asthma, chronic rhinosinusitis, major depressive disorder, and six hospitalizations in the last year for recurrent pneumonia and asthma exacerbations. During these hospitalizations, the only causative pathogens recognized were metapneumovirus and rhinovirus. No bacterial or fungal pathogens were identified; however, the patient received empiric antibiotic coverage for community acquired and healthcare-associated pneumonia on multiple occasions. The patient was a former tobacco user, and he intermittently used intravenous methamphetamine and inhaled cocaine. Family history was significant for asthma, alcohol use disorder, and coronary artery disease. His medications included abacavir-lamivudine, raltegravir, albuterol inhaler, fluticasone-salmeterol inhaler, montelukast, buprenorphine-naloxone, clonazepam, citalopram, mirtazapine, and olanzapine. He was allergic to trimethoprim-sulfamethoxazole.
On presentation, his heart rate was 140 beats per minute, blood pressure 130/70 mmHg, respiratory rate 28 breaths per minute, and oxygen saturation was 97% on 4 L of nasal cannula-delivered oxygen. His physical exam was significant for diaphoresis, labored breathing, tachycardia, and diffuse expiratory wheezing. A complete blood count (CBC) and basic metabolic panel (BMP) were unremarkable; lactate dehydrogenase (LDH) was 214 U/L (normal 110 - 205 U/L). Venous blood gas showed pH 7.33, PaCO2 47 mmHg, and PaO2 52 mmHg. Chest radiograph and CT angiogram demonstrated bilateral nodular consolidative opacities with tree-in-bud appearance and bilateral pleural wall thickening. The patient was admitted to the intensive care unit, and subsequently treated with vancomycin, piperacillin-tazobactam, azithromycin, pentamidine and methylprednisolone. Bronchoalveolar lavage was performed yielding negative bacterial and respiratory viral studies. Pneumocystis jiroveci stain, Legionella PCR, Nocardia culture, herpes culture, cytomegalovirus culture, and acid-fast bacilli smear were negative. Given the discrepancy between his HIV stage and recurrent pulmonary infections, serum immunoglobulins were measured to explore the possibility of a concurrent underlying deficiency state to better explain his recurrent infections. The results were notable for serum IgA < 5 mg/dL (normal 70–400 mg/dL), IgM 75 mg/dL (normal 40–230 mg/dL), and IgG 432 mg/dL (normal 700–1600 mg/dL) (Table 1). He was discharged on a course of oral antibiotics for healthcare-associated pneumonia, a steroid taper for asthma, and a referral to an immunologist for further management of his newly diagnosed IgA and IgG deficiencies; findings that were most consistent with CVID. Treatment with intravenous immunoglobulin (IVIg) was initiated and scheduled every three weeks. The patient had one additional hospitalization for bacterial pneumonia in the subsequent four weeks; however, following his second IVIg infusion, the patient had no further hospital admissions for thirty-six months.
DISCUSSION
We present a case of an HIV-positive patient with a one-year history of recurrent sinopulmonary infections attributed to his HIV infection, ultimately diagnosed with CVID. This case highlights the importance of recognizing the clinical signs and symptoms suggestive of an underlying immune deficiency syndrome. While this case describes the co-occurrence of two distinct immunodeficiency syndromes, the clinical relationship between HIV infection and primary immunoglobulin deficiencies should also be explored.
The hallmark of HIV disease is a profound progressive immunodeficiency resulting primarily from quantitative and qualitative deficiencies in T cell–mediated immunity. Eventually, the HIV-infected host CD4+ lymphocytes are destroyed, leading to a reduction in the CD4+ count. In general, HIV-infected patients are at higher risk for community-acquired bacterial infections as compared with HIV-negative patients, but this is most striking when CD4+ counts fall below 500 cells/μL,2 and rises in proportion to the decrease in the CD4+ cell count.3 By framing the index patient in a way that acknowledged that his HIV was virologically suppressed, a new theory was proposed; that an abnormality in humoral immunity could account for the patient’s recurrent infections.
The relationship between HIV and humoral immunity is complex, but a common finding in patients infected with HIV is polyclonal hypergammaglobulinemia.4,5,6 In a review of 107 patients with HIV infection, serum IgA concentration and serum IgG were elevated in one-third and two-thirds of patients, respectively, and this was strongly associated with HIV disease progression.7 Another study found a remarkably high level of polyclonal hypergammaglobulinemia (53%) among HIV-positive patients compared with 10% of HIV-negative controls.8 The mechanism of elevated immunoglobulin levels is multifactorial and may be related to a direct immune response to HIV or other pathogens (such as Epstein-Barr virus), HIV-associated hyperactivation of naïve B cells, and loss of regulation of antibody production.4,5,6,7 The polyclonal gammopathy seen in HIV can lead to an elevation in the paraprotein gap, otherwise known as the gamma gap. The paraprotein gap is the difference between the concentration of serum total protein and serum albumin. A large gap ( > 4 g/dL) can be caused by excessive production of immunoglobulins which may reflect an underlying condition: viral infection, malignancy, hematologic disorder, or autoimmune disease.9
Given the association between hypergammaglobulinemia and HIV infection, the hypogammaglobulinemia seen in our patient suggested a concomitant primary immunoglobulin deficiency syndrome, which ultimately led to his recurrent sinopulmonary infections. Primary immunoglobulin deficiencies have an estimated prevalence of one in 10,000 people in the general population and are frequently diagnosed in adulthood.10, 11 Primary immunoglobulin deficiencies should be suspected in patients who present with recurrent bacterial infections of the sinopulmonary tract, including recurrent otitis media, sinusitis, and pneumonia.12 They should be considered in patients with HIV if the severity or frequency of infections is out of proportion to the degree of HIV infection. For example, the annual incidence of bacterial pneumonia in HIV-positive patients ranges from 5.5 per 100, compared with 0.9 per 100 in HIV-negative patients.2 Use of antiretroviral therapy and increasing CD4+ count are associated with a significant reduction in the risk of bacterial pneumonia (2.3 and 10.8 episodes per 100 in patients with more than 500 and fewer than 200 CD4+ lymphocytes per cubic millimeter, respectively)2, 13 Thus, those patients with virologically suppressed HIV presenting with recurrent infections should have laboratory evaluation for immunoglobulin deficiency. One additional clue that may prompt consideration of immunoglobulin deficiency in a patient with HIV is a low or inappropriately normal paraprotein gap. A low paraprotein gap (< 1.9 g/dL) has already been shown to be an effective tool in reducing diagnostic delays for immunoglobulin deficiency syndromes in an adult population.14, 15 Given the polyclonal gammopathy and corresponding elevation in paraprotein gap seen in patients with HIV, a low or normal paraprotein gap could prompt a clinician to evaluate for immunoglobulin deficiency in the right clinical setting.
Initial laboratory evaluation should include a CBC with differential and serum IgA, IgG, and IgM levels. Evaluation for secondary causes of antibody deficiencies, such as protein-losing enteropathies, malnutrition, chronic kidney disease, hematologic malignances, and drugs (e.g., carbamazepine, phenytoin, disease-modifying antirheumatic drugs), should be considered.10, 16 Given the undetectable IgA level in the setting of low IgG (Table 1) in our patient, it is worthwhile to juxtapose selective IgA deficiency with CVID.
Selective IgA deficiency is the most common primary immunodeficiency and can be associated with IgG subclass deficiency and progression to CVID.17 It is characterized by decreased serum IgA concentration (< 0.07 g/L) and normal serum IgM and IgG levels.18 The majority of patients with this disease are asymptomatic, whereas selected patients suffer from recurrent mucosal infections, allergies, and autoimmune diseases. Patients with selective IgA deficiency who develop recurrent infections should have routine serum IgG and IgM measurements to monitor for progression to CVID.17
CVID is a primary antibody deficiency disease characterized by low serum levels of IgG, IgA, and/or IgM, leading to recurrent infections noted mostly in the respiratory and gastrointestinal tract.17 A study of 224 CVID patients reported the following mean immunoglobulin levels at diagnosis: IgG of 258 mg/dL, IgA of 28 mg/dL, and IgM of 40 mg/dL.1 In our patient with undetectable IgA and IgG of 432 mg/dL, it was theorized that he initially had selective IgA deficiency that later progressed to CVID. This appears to fit his clinical picture, as the patient’s only previous manifestation of humoral immunodeficiency was chronic rhinosinusitis. His sudden development of severe and recurrent respiratory infections was arguably due to progression from selective IgA deficiency to concomitant IgG deficiency.
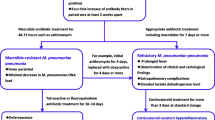
The standard treatment of CVID is IVIg, administered at a dose of 0.4 to 0.6 g/kg every 3–4 weeks.19, 20 The dose and frequency are generally adjusted to reach a goal trough IgG level of greater than 500 mg/dL.19 Supportive care, including consideration of long-term prophylactic antibiotics and pulmonary hygiene, is of utmost importance in the management of CVID.
The clinical improvement witnessed in our patient following the initiation of IVIg gives credence to concomitant humoral immunodeficiency as a paucity of evidence exists showing benefit of IVIg in HIV-infected adults without immunoglobulin deficiencies.21 Rather, treatment of patients with HIV and concomitant CVID should focus on treating each disease separately. The effect of HIV infection on patients with CVID is not completely understood; however, in rare cases, CVID has been reported to resolve transiently or permanently in patients with HIV infection.22,23,24,25,26 This resolution is based on the stimulation and recovery of IgG and IgM production following HIV infection in patients with CVID. Notably, IgA levels remained undetectable in these cases—a finding consistent with the concept that specific immunoregulatory and possibly environmental factors are required to induce CVID in patients with select IgA deficiency.23 Antiretroviral therapy and subsequent virologic suppression do not appear to effect immunoglobulin production, as two of the above cases demonstrated immunoglobulin recovery and resolution of CVID despite treatment.22, 23 Perhaps the mechanism that leads to polyclonal hypergammaglobulinemia in patients with HIV also leads to immunoglobulin recovery in patients with CVID. This remains a topic of further research that could have implications on treatment of CVID.
In summary, we have presented a case of concurrent CVID in an HIV positive patient, in whom recurrent severe respiratory infections were previously attributed to his HIV. Immunoglobulin deficiency should be considered in all patients with recurrent infections, especially in those patients whose primary medical conditions do not explain the recurrent nature or severity of their infections. The relationship between HIV, immunoglobulin deficiencies, and CVID should be further explored, and it is important to recognize that these distinct immunodeficiency syndromes can coexist.
References
Quinti I, Soresina A, Spadaro G, et al. Long-term follow-up and outcome of a large cohort of patients with common variable immunodeficiency. J Clin Immunol. 2007;27(3):308-316.
Hirschtick RE, Glassroth J, Jordan MC, et al. Bacterial pneumonia in persons infected with the human immunodeficiency virus. Pulmonary Complications of HIV Infection Study Group. The New England journal of medicine. 1995;333(13):845-851.
Kovacs JA, Masur H. Prophylaxis against opportunistic infections in patients with human immunodeficiency virus infection. The New England journal of medicine. 2000;342(19):1416-1429.
Lane HC, Masur H, Edgar LC, Whalen G, Rook AH, Fauci AS. Abnormalities of B-cell activation and immunoregulation in patients with the acquired immunodeficiency syndrome. The New England journal of medicine. 1983;309(8):453-458.
Moir S, Fauci AS. B cells in HIV infection and disease. Nat Rev Immunol. 2009;9(4):235-245.
De Milito A, Nilsson A, Titanji K, et al. Mechanisms of hypergammaglobulinemia and impaired antigen-specific humoral immunity in HIV-1 infection. Blood. 2004;103(6):2180-2186.
Fling JA, Fischer JR, Jr., Boswell RN, Reid MJ. The relationship of serum IgA concentration to human immunodeficiency virus (HIV) infection: a cross-sectional study of HIV-seropositive individuals detected by screening in the United States Air Force. J Allergy Clin Immunol. 1988;82(6):965-970.
Zemlin AE, Ipp H, Maleka S, Erasmus RT. Serum protein electrophoresis patterns in human immunodeficiency virus-infected individuals not on antiretroviral treatment. Ann Clin Biochem. 2015;52(Pt 3):346-351.
Dispenzieri A, Gertz MA, Therneau TM, Kyle RA. Retrospective cohort study of 148 patients with polyclonal gammopathy. Mayo Clin Proc. 2001;76(5):476-487.
Azar AE, Ballas ZK. Evaluation of the adult with suspected immunodeficiency. Am J Med. 2007;120(9):764-768.
Bonilla FA, Khan DA, Ballas ZK, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015;136(5):1186-1205 e1181-1178.
Yong PF, Chee R, Grimbacher B. Hypogammaglobulinaemia. Immunol Allergy Clin North Am. 2008;28(4):691-713, vii.
Sullivan JH, Moore RD, Keruly JC, Chaisson RE. Effect of antiretroviral therapy on the incidence of bacterial pneumonia in patients with advanced HIV infection. Am J Respir Crit Care Med. 2000;162(1):64-67.
Pecoraro A, Jolles S, Crescenzi L, et al. Validation of Calculated Globulin (CG) as a Screening Test for Antibody Deficiency in an Italian University Hospital. Curr Pharm Biotechnol. 2018;19(9):728-733.
Holding S, Khan S, Sewell WA, Jolles S, Dore PC. Using calculated globulin fraction to reduce diagnostic delay in primary and secondary hypogammaglobulinaemias: results of a demonstration project. Ann Clin Biochem. 2015;52(Pt 3):319-326.
Rose ME, Lang DM. Evaluating and managing hypogammaglobulinemia. Cleve Clin J Med. 2006;73(2):133-137. , 140, 143-134.
Aghamohammadi A, Mohammadi J, Parvaneh N, et al. Progression of selective IgA deficiency to common variable immunodeficiency. Int Arch Allergy Immunol. 2008;147(2):87-92.
Hammarstrom L, Vorechovsky I, Webster D. Selective IgA deficiency (SIgAD) and common variable immunodeficiency (CVID). Clin Exp Immunol. 2000;120(2):225-231.
Orange JS, Hossny EM, Weiler CR, et al. Use of intravenous immunoglobulin in human disease: a review of evidence by members of the Primary Immunodeficiency Committee of the American Academy of Allergy, Asthma and Immunology. J Allergy Clin Immunol. 2006;117(4 Suppl):S525-553.
Abolhassani H, Sagvand BT, Shokuhfar T, Mirminachi B, Rezaei N, Aghamohammadi A. A review on guidelines for management and treatment of common variable immunodeficiency. Expert Rev Clin Immunol. 2013;9(6):561-574; quiz 575.
Tiraboschi J, Ray S, Patel K, et al. The impact of immunoglobulin in acute HIV infection on the HIV reservoir: a randomized controlled trial. HIV Med. 2017;18(10):777-781.
Balugo-Lopez V, Hernandez Garcia de la Barrera E, Sastre J. Resolution of Common Variable Immunodeficiency After HIV Infection. J Investig Allergol Clin Immunol. 2016;26(5):333-334.
Jolles S, Tyrer M, Johnson M, Webster D. Long term recovery of IgG and IgM production during HIV infection in a patient with common variable immunodeficiency (CVID). J Clin Pathol. 2001;54(9):713-715.
Wright JJ, Birx DL, Wagner DK, Waldmann TA, Blaese RM, Fleisher TA. Normalization of antibody responsiveness in a patient with common variable hypogammaglobulinemia and HIV infection. The New England journal of medicine. 1987;317(24):1516-1520.
Morell A, Barandun S, Locher G. HTLV-III seroconversion in a homosexual patient with common variable immunodeficiency. The New England journal of medicine. 1986;315(7):456-457.
Webster AD, Lever A, Spickett G, Beattie R, North M, Thorpe R. Recovery of antibody production after HIV infection in 'common' variable hypogammaglobulinaemia. Clin Exp Immunol. 1989;77(3):309-313.
Acknowledgements
The authors thank Dr. Anthony Montanaro, for his resource and guidance for immunologic questions and issues, and critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gollapudi, D., O’Donnell, M., NeSmith, M. et al. Recurrent Sinopulmonary Infections in a Patient Whose HIV Masked Common Variable Immunodeficiency. J GEN INTERN MED 35, 341–344 (2020). https://doi.org/10.1007/s11606-019-05435-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05435-3