Abstract
Background
Women with chronic health conditions benefit from reproductive planning and access to highly effective contraception.
Objective
To determine the prevalence of and relationship between chronic health conditions and use of highly effective contraception among reproductive-age women.
Design
Retrospective cohort study using electronic health records.
Participants
We identified all women 16–49 years who accessed care in the two largest health systems in the US Intermountain West between January 2010 and December 2014.
Main Measures
We employed administrative codes to identify highly effective contraception and flag chronic health conditions listed in the US Medical Eligibility Criteria for Contraceptive Use (US MEC) and known to increase risk of adverse pregnancy outcomes. We described use of highly effective contraception by demographics and chronic conditions. We used multinomial logistic regression to relate demographic and disease status to contraceptive use.
Key Results
Of 741,612 women assessed, 32.4% had at least one chronic health condition and 7.3% had two or more chronic conditions. Overall, 7.6% of women with a chronic health condition used highly effective contraception vs. 5.1% of women without a chronic condition. Women with chronic conditions were more likely to rely on public health insurance. The proportion of women using long-acting reversible contraception did not increase with chronic condition number (5.8% with 1 condition vs. 3.2% with 5 or more). In regression models adjusted for age, race, ethnicity, and payer, women with chronic conditions were more likely than those without chronic conditions to use highly effective contraception (aRR 1.4; 95% CI 1.4–1.5). Public insurance coverage was associated with both use of long-acting reversible contraception (aRR 2.2; 95% CI 2.1–2.3) and permanent contraception (aRR 2.9; 95% CI 2.7–3.1).
Conclusions
Nearly a third of reproductive-age women in a regional health system have one or more chronic health condition. Public insurance increases the likelihood that women with a chronic health condition use highly effective contraception.
Similar content being viewed by others
INTRODUCTION
In the United States (U.S.), the prevalence of chronic health conditions and multi-morbidity are increasing, in part due to high rates of obesity and increased longevity for individuals with chronic conditions.1 This change in overall prevalence, along with the increasing age at first childbirth, contributes to maternal morbidity and mortality.2,3,4,5 Even when well controlled, maternal chronic health conditions can increase the risk of adverse outcomes during pregnancy.4, 6 Nearly half of all pregnancies in the U.S. are unintended.7 Pregnancy intention is an independent risk factor for preterm birth, low-birth-weight infants, and other adverse physical and mental childhood health outcomes.8,9,10,11 Consistent and correct use of contraception effectively prevents unintended pregnancy and allows women to optimize their health prior to pregnancy.7 Unfortunately, women with chronic health conditions have greater risk for unintended pregnancy than healthy women,12 in addition to increased risk of adverse maternal and neonatal outcomes related to their condition.13 Contraceptive safety is a central concern for women and medical providers. The Centers for Disease Control published valuable practice guidelines called the U.S. Medical Eligibility Criteria for Contraceptive Use (US MEC) to support healthcare providers in making the safest recommendations of contraceptive methods for women with specific medical or reproductive characteristics. The US MEC lists over 200 health condition and ranks the safety of use of estrogen-based methods (pills, patches, or rings), short-acting progestin-only methods (pills or injectable), and long-acting reversible contraceptives (LARC), such as intrauterine devices (IUDs) and contraceptive implants. LARC methods are the most effective (e.g., < 1% failure rate vs. 8% failure with pills) and safest contraceptives for the majority of women, as they are not estrogen-based.14 The US MEC recommends LARC as first-line reversible contraceptives for women with chronic health conditions in which an unintended pregnancy would pose unacceptable risks.14 Alternatively, for women who do not desire future fertility, permanent contraceptive (PC) options have included tubal ligation (< 1% failure rate) and hysteroscopic sterilization.
Reproductive-age women are more likely to seek routine care from a general medical provider than from an obstetrician gynecologist.15 Unfortunately, many women with chronic health conditions receive misinformation regarding contraceptive safety. Limited attention to the reproductive health needs of women with chronic conditions16 may lead to disease-related disparities in LARC and PC use.17, 18
A recent study of commercially insured women estimated that 12.1% of U.S. reproductive-age women had at least one of the chronic conditions listed by the US MEC for which LARC is recommended, yet use of either LARC or PC was low.18 As contraceptive access can be more challenging for women without commercial insurance, we sought to determine the prevalence of and relationship between chronic health conditions and use of LARC and PC among reproductive-age women in a regional, mixed-payer health system.
METHODS
We conducted a retrospective cohort study utilizing the University of Utah Health Care (UUHC) and Intermountain Healthcare (IHC) Data Warehouses. The Utah Population Database (UPDB) served to aggregate all inpatient, outpatient, and ambulatory surgery billing codes across institutions. UUHC and IHC provide care to > 85% of the state population and are regional, tertiary care centers for the Intermountain West, which accounts for ~ 10% of the U.S. land mass. The UUHC and IHC Institutional Review Boards approved this study.
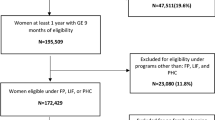
We included all women, ages 16–49 years, with any encounter type at either UUHC or IHC occurring between January 2010 and December 2014. The study group included women with one or more chronic health condition known to increase the risk of adverse outcomes in the setting of an unintended pregnancy14 and conditions that are more prevalent among reproductive-age women than in men and can be impacted by pregnancy, such as depression, asthma, obesity, and autoimmune diseases.5 The investigative team identified chronic health conditions via International Classification of Diseases, Ninth Revision (ICD-9) codes. We included chronic condition diagnoses that occurred at any time from 1996 to 2014 (based on data warehouse limitations), but contact with the health system in 2010–2014 was required for study eligibility. No minimum number of visits was required for inclusion, except in defining the study population with chronic disease. Study subjects identified as chronic-condition prevalent cases must have the same diagnosis coded at least twice, with a minimum interval of 30 days, to avoid false positives from coding error. We confirmed first date of diagnosis whenever possible, especially for chronic conditions associated with time (e.g., bariatric surgery or solid organ transplant within the past 2 years). We completed a manual chart review on a random sample of 2% of the study group to narrow or refine specific diagnosis codes for final cohort inclusion. For example, chart reviews found the code listed for bariatric surgery was also used for other, non-weight loss indications. In response, we required both an obesity code and the surgical procedure code to identify the bariatric surgery cohort.
We used ICD-9 and Current Procedural Terminology (CPT®) codes for IUD and contraceptive implant device insertion, surveillance, removal, and exchange, as well as related device orders and current and historical medication records to identify LARC use within the 5-year2010–2014 capture frame. We considered LARC “use” as an outcome, rather than limiting to “insertion.” Differing LARC devices are FDA approved for use for 3–12 years and may be managed at other facilities or family planning clinics; thus, all events related to care may not be captured within a health system, due to insurance changes or lack of coverage. CPT® codes flagged tubal sterilization and hysterectomy procedures, including procedure dates at any time from 1996 to 2014. While recognizing that hysterectomy is not done for contraceptive purposes, we identified these women as no longer at risk for unintended pregnancy.19 Women with a code for sterilization or hysterectomy were excluded from the LARC cohort when analyzed separately, even if they received a LARC method post-procedure for non-contraceptive benefits.
We summarized descriptive characteristics with frequencies and proportions and conducted chi-square tests for comparisons within groups, stratifying by presence or absence of chronic health conditions. We used multinomial logistic regression to relate demographic and disease status to LARC use, sterilization, and hysterectomy. We report relative-risk ratios with robust standard errors in the adjusted models, controlling for age, insurance, race, and ethnicity. We set the significance threshold at p < 0.05, flagged the level of on each variable, and defined them in the table footnote. We used Stata 15 to conduct all analyses.
RESULTS
A total of 741,612 reproductive-age women accessed care at UUHC and/or IHC between 2010 and 2014. Of these women, 32.4% (n = 240,483) had at least one chronic health condition (Table 1). Women with chronic conditions had greater likelihood of being older, non-Hispanic, and White and having public insurance. Women with chronic health conditions had greater likelihood of having a hysterectomy (1.2 vs. 0.4%, p < 0.001) or tubal sterilization (2.2 vs. 1.1%, p < 0.001), compared to healthy women. Women with a chronic condition were more likely to use an IUD (4.9% vs 3.7%, p < 0.001) and contraceptive implant (0.5% vs 0.3%, p < 0.001) than women without chronic conditions.
Depression was the most common chronic condition, impacting 15% of women of reproductive age. LARC and PC use varied by chronic health condition. Of all chronic health conditions, women with malignant liver tumors had the lowest proportion of either LARC or PC use (3.0% combined). Those with thrombogenic mutations had the highest proportion of LARC use (9.5%) and PC (3.6%). Women with breast cancer had the lowest proportion of LARC use (2.3%) (Table 2).
Multi-morbidity impacted 7.3% of the cohort and prevalence increased with age: 5.0% of those under 35 years had two or more health conditions, compared to 10.8% of those aged 35–49 years. As the number of chronic health conditions increased, public payer reliance increased. As the number of chronic conditions increased, the proportion of women using LARC decreased, from 5.8% of women with one condition down to 3.2% of women with five or more conditions. LARC use, sterilization, and hysterectomy were all associated with one or more chronic condition, compared to healthy women in models controlling for age, race, ethnicity, and payer, but the strength of association did not increase with multi-morbidity burden. (Table 3)
After adjusting for age, race, ethnicity, and payer type, we found women with a chronic health condition were more likely to use LARC (aRR 1.4; 95% CI 1.4–1.5), or have had a hysterectomy (aRR 2.1; 95% CI 2.0–2.3) or permanent contraception (aRR 1.7; 95% CI 1.7–1.8) compared to women without a chronic condition. Women without insurance were less likely to use highly effective contraception, whether or not they had a chronic condition (Table 4).
DISCUSSION
This 5-year cross-sectional study of two large health systems found that nearly 1/3 of reproductive-age female patients had one or more chronic health conditions that could increase risk of adverse pregnancy outcomes, especially in the setting of an unintended pregnancy. Potentially further increasing health and pregnancy risks,20 7.3% of reproductive-age women had multiple chronic conditions. However, only 7.6% of women with a chronic health condition were using highly effective contraception. These findings are similar to a prior study of commercially insured US women, which reported that 12.1% of women of reproductive age had one or more chronic condition, and that few were using LARC and PC.18
In addition, we found that public insurance was an important predictor of use of highly effective contraception, particularly among women with multiple chronic conditions. As implementation of the Patient Protection and Affordable Care Act (ACA) of 2010 and subsequent Medicaid expansion vary by state, opportunities remain in many states to improve consistent public funding for comprehensive contraceptive services. As it is estimated that 45% of all U.S. births are publicly funded,21 national efforts to improve preconception health and reduce maternal mortality need to remain focused on health insurance coverage that allows access to the full range of contraception for U.S. women of reproductive age.
Limitations of this study include our inability to control for number of visits or provider type or standardize the period of observation for each individual. Further, we relied on structured billing data to identify chronic conditions and LARC use or PC procedures. Although we focused on LARC and PC because they are typically more effective than short-acting contraceptives, we recognize that with many chronic conditions these are safe and reasonable options. We attempted to minimize false positives through manual chart reviews to validate codes and requiring recurrent codes > 30 days apart to meet criteria for a condition, but it is possible that some women identified as having no chronic conditions received care for a chronic condition in other settings. In particular, diagnoses with relapsing and remitting courses, such as asthma, may have been missed. We also could not capture disease severity. Although this 5-year study captured all healthcare visits at two large institutions, we lack data from free-standing family planning clinics where contraceptive services may have occurred. We opted to define our outcome as LARC “use,” rather than limiting to insertions, which precludes direct comparison with studies using LARC insertion as an outcome.
In conclusion, many women of reproductive age are burdened by chronic health conditions, yet relatively few are using highly effective contraception. As primary care providers care for many women with chronic conditions, efforts to ensure effective reproductive planning and prompt access to contraceptive services are needed. Our findings also highlight the importance of public insurance that allows women with chronic conditions to access comprehensive reproductive health services.
References
Ward BW, Schiller JS. Prevalence of Multiple Chronic Conditions Among US Adults: Estimates From the National Health Interview Survey, 2010. Preventing Chronic Disease. 2013;10:E65.
Kim SY, Dietz PM, England L, Morrow B, Callaghan WM. Trends in pre-pregnancy obesity in nine states, 1993-2003. Obesity. 2007;15(4):986-93.
Martin JA, Hamilton BE, Sutton PD, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67(1):1-55.
Berg CJ, Mackay AP, Qin C, Callaghan WM. Overview of maternal morbidity during hospitalization for labor and delivery in the United States: 1993-1997 and 2001-2005. Obstet Gynecol. 2009;113(5):1075-81.
Rocca WA, Boyd CM, Grossardt BR, et al. Prevalence of multimorbidity in a geographically defined American population: patterns by age, sex, and race/ethnicity. Mayo Clin Proc. 2014;89(10):1336-49.
Howland RE, Angley M, Won SH, Wilcox W, Searing H, Tsao TY. Estimating the Hospital Delivery Costs Associated With Severe Maternal Morbidity in New York City, 2008-2012. Obstet Gynecol. 2018;131(2):242-52.
Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008-2011. N Engl J Med. 2016;374(9):843-52.
Hellerstedt WL, Pirie PL, Lando HA, et al. Differences in preconceptional and prenatal behaviors in women with intended and unintended pregnancies. Am J Pub Health. 1998;88(4):663-6.
Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83-111.
Axinn WG, Barber JS, Thornton A. The long-term impact of parents’ childbearing decisions on children’s self-esteem. Demography. 1998;35(4):435-43.
Barber JS, Axinn WG, Thornton A. Unwanted childbearing, health, and mother-child relationships. J Health Soc Behav. 1999;40(3):231-57.
Chor J, Rankin K, Harwood B, Handler A. Unintended pregnancy and postpartum contraceptive use in women with and without chronic medical disease who experienced a live birth. Contraception. 2011;84(1):57-63.
Chuang CH, Velott DL, Weisman CS. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Mat Child Health J. 2010;14(5):713-9.
Centers for Disease Control U.S. Medically Eligibility Criteria for Contraceptive Use, 2016. Available at: http://www.cdc.gov/mmwr/pdf/rr/rr5904.pdf. Accessed November 8, 2016.
Simon AE, Uddin SFG. Trends in Seeing an Obstetrician-Gynecologist Compared With a General Physician Among U.S. Women, 2000-2015. Obstet Gynecol. 2017;130(4):677-683.
Gawron LM, Goldberger AR, Gawron AJ, Hammond C, Keefer L. Disease-related pregnancy concerns and reproductive planning in women with inflammatory bowel diseases. J Fam Plann Reprod Health Care. 2015;41(4):272-7.
Gawron LM, Redd A, Suo Y, Pettey W, Turok DK, Gundlapalli AV. Long-acting Reversible Contraception Among Homeless Women Veterans With Chronic Health Conditions: A Retrospective Cohort Study. Med Care. 2017;55(S9):S111-S120.
Champaloux SW, Tepper NK, Curtis KM, et al. Contraceptive Use Among Women With Medical Conditions in a Nationwide Privately Insured Population. Obstet Gynecol. 2015;126(6):1151-1159.
Callegari LS, Gray KE, Zephyrin LC, et al. Hysterectomy and Bilateral Salpingo-Oophorectomy: Variations by History of Military Service and Birth Cohort. Gerontologist. 2016;56(S1):S67-77.
Farr A, Lenz-Gebhart A, Einig S, et al. Outcomes and trends of peripartum maternal admission to the intensive care unit. Wien Klin Wochenschr. 2017;129(17-18):605-611.
Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Issues. 2013;23(5):e273-280.
Contributors
Ware Branch, MD; Reed Barney, BA; Vickie Baer, Alison Frasier and Jeff Bennion
Funding
This project is funded by the University of Utah Center for Clinical and Translational Science and the Program in Personalized Health Collaborative Pilot Project Grant. Team members receive support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Research on Women’s Health of the National Institute of Health, LMG via K12HD085816, JNS via K12HD085852, and DKT via K24HD087436.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The UUHC and IHC Institutional Review Boards approved this study.
Conflict of Interest
The authors declare that they do not have a conflict of interest. The University of Utah Department of Obstetrics and Gynecology receives industry funding from Sebela, Femasys, and Medicines360. No industry supported trial data or relationships influenced the collection or analysis of these data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations
Some of this information was presented as a poster and published abstract at the North American Forum on Family Planning in Denver, CO, November 2016.
Rights and permissions
About this article
Cite this article
Gawron, L.M., Sanders, J.N., Sward, K. et al. Multi-morbidity and Highly Effective Contraception in Reproductive-Age Women in the US Intermountain West: a Retrospective Cohort Study. J GEN INTERN MED 35, 637–642 (2020). https://doi.org/10.1007/s11606-019-05425-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05425-5