ABSTRACT
BACKGROUND
There is growing evidence that even small and solo primary care practices can successfully transition to full Patient Centered Medical Home (PCMH) status when provided with support, including practice redesign, care managers, and a revised payment plan. Less is known about the quality and efficiency outcomes associated with this transition.
OBJECTIVE
Test quality and efficiency outcomes associated with 2-year transition to PCMH status among physicians in intervention versus control practices.
DESIGN
Randomized Controlled Trial.
PARTICIPANTS
Eighteen intervention practices with 43 physicians and 14 control practices with 24 physicians; all from adult primary care practices.
INTERVENTIONS
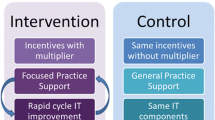
Modeled on 2008 NCQA PPC®-PCMH™, intervention practices received 18 months of tailored practice redesign support; 2 years of revised payment, including up to $2.50 per member per month (PMPM) for achieving quality targets and up to $2.50 PMPM for PPC-PCMH recognition; and 18 months of embedded care management support. Controls received yearly participation payments.
MAIN MEASURES
Eleven clinical quality indicators from the 2009 HEDIS process and health outcomes measures derived from patient claims data; Ten efficiency indicators based on Thomson Reuter efficiency indexes and Emergency Department (ED) Visit Ratios; and a panel of costs of care measures.
KEY RESULTS
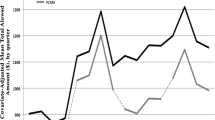
Compared to control physicians, intervention physicians significantly improved TWO of 11 quality indicators: hypertensive blood pressure control over 2 years (intervention +23 percentage points, control –2 percentage points, p = 0.02) and breast cancer screening over 3 years (intervention +3.5 percentage points, control −0.4 percentage points, p = 0.03). Compared to control physicians, intervention physicians significantly improved ONE of ten efficiency indicators: number of care episodes resulting in ED visits was reduced (intervention −0.7 percentage points, control + 0.5 percentage points, p = 0.002), with 3.8 fewer ED visits per year, saving approximately $1,900 in ED costs per physician, per year. There were no significant cost-savings on any of the pre-specified costs of care measures.
CONCLUSIONS
In a randomized trial, we observed that some indicators of quality and efficiency of care in general adult primary care practices transitioning to PCMH status can be significantly, but modestly, improved over 2 years, although most indicators did not improve and there were no cost-savings compared with control practices. For the most part, quality and efficiency of care provided in unsupported control practices remained unchanged or worsened during the trial.


Similar content being viewed by others
REFERENCES
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affair. 2008;27(3):759–69.
Barr MS. The need to test the patient-centered medical home. JAMA. 2008;300(7):834–5.
Peikes D, Zutshi A, Genevro J, Smith K, Parchman M, Meyers D. Early Evidence on the Patient-Centered Medical Home. Final Report. Rockville (MD): Agency for Healthcare Research and Quality; 2012 Feb. Contract No.: HHSA290200900019I/HHSA29032002T and HHSA290200900019I/HHSA29032005T. Sponsored by: Agency for Healthcare Research and Quality.
Counsell SR, Callahan CM, Tu W, Stump TW, Arling GW. Cost analysis of the geriatric resources for assessment and care of elders management intervention. J Am Geriatr Soc. 2009;57(8):1420–6.
Hughes SL, Weaver FM, Giobbie-Hurder A, et al. Effectiveness of team-managed home-based primary care. JAMA. 2000;284(22):2877–85.
Boult C, Reider L, Leff B, et al. The effect of guided care teams on the use of health services: results from a cluster-randomized controlled trial. Arch Intern Med. 2011;171(5):460–6.
Unützer J, Katon WJ, Fan MY, et al. Long-term cost effects of collaborative care for late-life depression. Am J Manag Care. 2008;14(2):95–100.
Steele GD, Haynes JA, Davis DE, et al. How Geisinger’s advanced medical home model argues the case for rapid-cycle innovation. Health Affair. 2010;29(11):2047–53.
Bielaszka-DuVernay C. The ‘GRACE’ model: in-home assessments lead to better care for dual eligibles. Health Affair. 2011;30(3):431–4.
Counsell SR, Callahan CM, Clark DO, et al. Geriatric care management for low-income seniors: a randomized controlled trial. JAMA. 2007;298(22):2623–33.
Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomized trial for depressed elderly patients in primary care. BMJ. 2006;332(7536):259–62.
Dorr DA, Wilcox AB, Brunker CP, Burdon RE, Donnelly SM. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. J Am Geriatr Soc. 2008;56(12):2195–202.
National Committee for Quality Assurance. Standards and Guidelines for Physician Practice Connections—Patient-Centered Medical Home Version. 2008 [cited 2013 February 4]. Available from: URL: http://www.usafp.org/PCMH-Files/NCQA-Files/PCMH_Overview_Apr01.pdf.
Fifield J, Dauser Forrest D, Martin-Peele M, Burleson JA, Goyzueta J, Fujimoto M, Gillespie W. A Randomized, Controlled Trial of Implementing the Patient-Centered Medical Home Model in Solo and Small Practices. JGIM 2012; Online First 07 September 2012, doi: 10.1007/s11606-012-2197-z.
Bitton A, Martin C, Landon BE. A nationwide survey of patient centered medical home demonstration projects. JGIM. 2010;25(6):584–92.
Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol 1994; Suppl 12:70–5.
Gawande A. Medical Report: the Hot Spotters. The New Yorker 2011 January 24 [cited 2013 February 4]. Available from: URL: http://www.newyorker.com/reporting/2011/01/24/110124fa_fact_gawande.
Robert Wood Johnson Foundation. Expanding “Hot spotting” to New Communities. Princeton (NJ): Robert Wood Johnson Foundation; 1 January 2012 [cited 2013 February 4]. Available from: URL: http://www.rwjf.org/content/dam/farm/meetings_and_conferences/speeches_and_presentations/2012/rwjf72538.
National Committee for Quality Assurance (US). HEDIS 2009. Washington: Technical Specifications. 2008;2.
National Committee for Quality Assurance. Quality Compass 2012. Available at: URL: http://www.ncqa.org/tabid/177/Default.aspx. Accessed February 4, 2013.
Rosenthal MB, Abrams MK, Bitton A, Patient-Centered Medical Home Evaluators’ Collaborative. Recommended Core Measures for Evaluating the Patient-Centered Medical Home: Cost, Utilization, and Clinical Quality [data brief]. New York: Commonwealth Fund; 2012 May. Publication No. 1601,12.
Meyers D, Peikes D, Dale S, Lundquist E, Genevro J. Improving Evaluations of the Medical Home. Rockville (MD): Agency for Healthcare Research and Quality; 2011 Sept. AHRQ Publication No. 11-0091.
Thomson Healthcare. MEG—Medical Episode Grouper™ [manual]. New York (NY): Thomson Healthcare; 2007.
Lyons K, Sayer A. Longitudinal dyad models in family research. J Marriage Fam. 2005;67(4):1048–60.
Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31(3):437–48.
Barnett R, Marshall N, Raudenbush S, Brennan R. Gender and the relationship between job experiences and psychological distress: a study of dual-earner couples. J Pers Soc Psychol. 1993;64(5):794–806.
Raudenbush S, Brennan R, Barnett R. A multivariate hierarchical model for studying psychological change within married couples. J Fam Psychol. 1995;9(2):161–74.
Sheskin DJ. Handbook of Parametric and Nonparametric Statistical Procedures. 3rd ed. Boca Raton (FL): Chapman & Hall; 2004.
Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. Boston (MA): Pearson; 2007.
Raudenbush S, Bryk A, Congdon R. HLM 6 for Windows [computer program]. Skokie (IL): Scientific Software International, Inc; 2004.
Raudenbush SW, Bryk AS. Hierarchical Linear Models. Thousand Oaks (CA): Sage Publications, Inc; 2002.
Hox J. Multilevel Analysis: Techniques and Applications. 2nd ed. New York (NY): Routledge; 2010:233–56.
Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA. Community care of North Carolina: improving care through community health networks. Ann Fam Med. 2008;6(4):361–7.
Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for physicians. Health Affair. 2010;29(5):835–43.
Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7(3):254–60.
Solberg LI, Asche SE, Fontaine P, Flottemesch TJ, Anderson LH. Trends in quality during medical home transformation. Ann Fam Med. 2011;9(6):515–21.
Milstein A, Gilbertson E. American medical home runs: four real-life examples of primary care practices that show a better way to substantial savings. Health Affair. 2009;28(5):1317–26.
Nelson EC, Batalden PB, Godfrey MM, eds. Quality by Design: A Clinical Microsystems Approach. San Francisco (CA): Jossey-Bass; 2007.
Villagra VG. Accelerating the adoption of medical homes in connecticut: a chronic-care support system modeled after public utilities. Conn Med. 2012;76(3):173–8.
Asch DA, Muller RW, Volpp KG. Automated hovering in health care—watching the 5,000 hours. N Engl J Med. 2012;367(1):1–3.
Acknowledgements
The Commonwealth Fund supported the independent evaluation of this demonstration by the Ethel Donaghue Center for Translating Research into Practice and Policy (TRIPP Center) at the University of Connecticut Health Center from 1 December 2007 through 31 March 2010. EmblemHealth has provided continued evaluation support for the purposes of data analysis, 1 March 2011 through 31 May 2011 and 1 September 2011 to 31 December 2013. The full trial protocol can be accessed by contacting EmblemHealth.
Conflict of Interest
Judith Fifield, PhD, reports having received two honoraria from Zimmer in the last 3 years. All other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fifield, J., Forrest, D.D., Burleson, J.A. et al. Quality and Efficiency in Small Practices Transitioning to Patient Centered Medical Homes: A Randomized Trial. J GEN INTERN MED 28, 778–786 (2013). https://doi.org/10.1007/s11606-013-2386-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2386-4