ABSTRACT
BACKGROUND
Failure to follow up microbiology results pending at the time of hospital discharge can delay diagnosis and treatment of important infections, harm patients, and increase the risk of litigation. Current systems to track pending tests are often inadequate.
OBJECTIVE
To design, implement, and evaluate an automated system to improve follow-up of microbiology results that return after hospitalized patients are discharged.
DESIGN
Cluster randomized controlled trial.
SUBJECTS
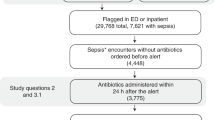
Inpatient and outpatient physicians caring for adult patients hospitalized at a large academic hospital from February 2009 to June 2010 with positive and untreated or undertreated blood, urine, sputum, or cerebral spinal fluid cultures returning post-discharge.
INTERVENTION
An automated e-mail-based system alerting inpatient and outpatient physicians to positive post-discharge culture results not adequately treated with an antibiotic at the time of discharge.
MAIN MEASURES
Our primary outcome was documented follow-up of results within 3 days. Secondary outcomes included physician awareness and assessment of result urgency, impact on clinical assessments and plans, and preferred alerting scenarios.
KEY RESULTS
We evaluated the follow-up of 157 post-discharge microbiology results from patients of 121 physicians. We found documented follow-up in 27/97 (28%) results in the intervention group and 8/60 (13%) in the control group [aOR 3.2, (95% CI 1.3-8.4); p = 0.01]. Of all inpatient physician respondents, 32/82 (39%) were previously aware of the results, 45/77 (58%) felt the results changed their assessments and plans, 43/77 (56%) felt the results required urgent action, and 67/70 (96%) preferred alerts for current or broader scenarios.
CONCLUSION
Our alerting system improved the proportion of important post-discharge microbiology results with documented follow-up, though the proportion remained low. The alerts were well received and may be expanded in the future.



Similar content being viewed by others
References
Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143:121–8.
Were MC, Li X, Kesterson J, et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24:1002–6.
El-Kareh R, Roy CL, Brodsky G, Perencevich M, Poon EG. Incidence and predictors of microbiology results returning post-discharge and requiring follow-up. J Hosp Med 2011.
Wilson JW, Marshall WF, Estes LL. Detecting delayed microbiology results after hospital discharge: improving patient safety through an automated medical informatics tool. Mayo Clin Proc. 2011;86:1181–5.
Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145:488–96.
Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49:196–205.
Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102–12.
Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487–94.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41.
van Walraven C, Seth R, Laupacis A. Dissemination of discharge summaries. Not reaching follow-up physicians. Can Fam Physician. 2002;48:737–42.
Walz SE, Smith M, Cox E, Sattin J, Kind AJ. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. J Gen Intern Med 2010.
Dalal AK, Poon EG, Karson AS, Gandhi TK, Roy CL. Lessons learned from implementation of a computerized application for pending tests at hospital discharge. J Hosp Med. 2011;6:16–21.
Poon EG, Gandhi TK, Sequist TD, Murff HJ, Karson AS, Bates DW. “I wish I had seen this test result earlier!”: Dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004;164:2223–8.
Singh H, Wilson L, Reis B, Sawhney MK, Espadas D, Sittig DF. Ten strategies to improve management of abnormal test result alerts in the electronic health record. J Patient Saf. 2010;6:121–3.
Singh H, Wilson L, Petersen LA, et al. Improving follow-up of abnormal cancer screens using electronic health records: trust but verify test result communication. BMC Med Inform Decis Mak. 2009;9:49.
Poon EG, Wang SJ, Gandhi TK, Bates DW, Kuperman GJ. Design and implementation of a comprehensive outpatient Results Manager. J Biomed Inform. 2003;36:80–91.
Ferris TG, Johnson SA, Co JP, et al. Electronic results management in pediatric ambulatory care: qualitative assessment. Pediatrics. 2009;123(Suppl 2):S85–91.
Wahls TL, Cram PM. The frequency of missed test results and associated treatment delays in a highly computerized health system. BMC Fam Pract. 2007;8:32.
Graumlich JF, Novotny NL, Stephen Nace G, et al. Patient readmissions, emergency visits, and adverse events after software-assisted discharge from hospital: cluster randomized trial. J Hosp Med. 2009;4:E11–9.
Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10:523–30.
Campbell MK, Mollison J, Steen N, Grimshaw JM, Eccles M. Analysis of cluster randomized trials in primary care: a practical approach. Fam Pract. 2000;17:192–6.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in US hospitals. N Engl J Med. 2009;360:1628–38.
Wang SJ, Kuperman GJ, Ohno-Machado L, Onderdonk A, Sandige H, Bates DW. Using electronic data to predict the probability of true bacteremia from positive blood cultures. Proc AMIA Symp 2000; 893–7.
Acknowledgements
This study was supported by grants from CRICO/RMF, Cambridge, MA, and the National Library of Medicine (2T15 LM 007092-17). The funding agencies played no role in the conduct of the study, collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. Dr. El-Kareh had full access to all the data in the study and takes responsibility for the integrity and the accuracy of the data analysis.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by grants from CRICO/RMF and the National Library of Medicine (2T15 LM 07092-17), and was presented at the 34th Annual Meeting of the Society of General Internal Medicine on May 5, 2011 in Phoenix, AZ.
Rights and permissions
About this article
Cite this article
El-Kareh, R., Roy, C., Williams, D.H. et al. Impact of Automated Alerts on Follow-Up of Post-Discharge Microbiology Results: A Cluster Randomized Controlled Trial. J GEN INTERN MED 27, 1243–1250 (2012). https://doi.org/10.1007/s11606-012-1986-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-1986-8