Abstract
Objective
Postoperative complications strongly impact the postoperative course and long-term outcome of patients who underwent liver resection for colorectal liver metastases (CRLM). Among them, infectious complications play a relevant role. The aim of this study was to evaluate if infectious complications still impact overall and disease-free survival after liver resection for CRLM once patients were matched with a propensity score matching analysis based on Fong’s criteria.
Methods
A total of 2281 hepatectomies were analyzed from a multicentric retrospective cohort of hepatectomies. Patients were matched with a 1:3 propensity score analysis in order to compare patients with (INF+) and without (INF−) postoperative infectious complications.
Results
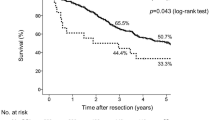
Major resection (OR = 1.69 (1.01–2.89), p = 0.05) and operative time (OR = 1.1 (1.1–1.3), p = 0.05) were identified as risk factors of infectious complications. After propensity score matching, infectious complications are associated with overall survival (OS), with 1-, 3-, 5-year OS at 94, 81, and 66% in INF− and 92, 66, and 57% in INF+ respectively (p = 0.01). Disease-free survival (DFS) was also different with regard to 1-, 3-, 5-year survival at 65, 41, and 22% in R0 vs. 50, 28, and 17% in INF+ (p = 0.007).
Conclusion
Infectious complications are associated with decreased overall and disease-free survival rates.





Similar content being viewed by others
References
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):309-318-321.
Laurent C, Sa Cunha A, Couderc P, Rullier E, Saric J. Influence of postoperative morbidity on long-term survival following liver resection for colorectal metastases. Br J Surg [Internet]. 2003 Sep [cited 2016 Jul 29];90(9):1131–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12945082
Adam R, de Gramont A, Figueras J, Kokudo N, Kunstlinger F, Loyer E, et al. Managing synchronous liver metastases from colorectal cancer: a multidisciplinary international consensus. Cancer Treat Rev [Internet]. 2015; Available from: http://linkinghub.elsevier.com/retrieve/pii/S0305737215001280
Memeo R, De Blasi V, Adam R, Goéré D, Azoulay D, Ayav A, et al. Parenchymal-sparing hepatectomies (PSH) for bilobar colorectal liver metastases are associated with a lower morbidity and similar oncological results: a propensity score matching analysis. 2016;781–90. Available from: http://www.elsevier.com/authorsrights
Hallet J, Sa Cunha A, Cherqui D, Gayet B, Goéré D, Bachellier P, et al. Laparoscopic compared to open repeat hepatectomy for colorectal liver metastases: a multi-institutional propensity-matched analysis of short- and long-term outcomes. World J Surg [Internet]. 2017 Jul 17 [cited 2017 Jul 28]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/28717911
Rizk NP1, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, Brennan MF RV. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg. 2004;Jan(198(1)):42–50.
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg [Internet]. 2005 Sep [cited 2016 Jul 30];242(3):326–41-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16135919
Farid SG, Aldouri A, Morris-Stiff G, Khan AZ, Toogood GJ, Lodge JPA, et al. Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg [Internet]. 2010 Jan [cited 2016 Jul 30];251(1):91–100. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19858702
Ito H, Are C, Gonen M, D’Angelica M, Dematteo RP, Kemeny NE, et al. Effect of postoperative morbidity on long-term survival after hepatic resection for metastatic colorectal cancer. Ann Surg [Internet]. 2008 Jun [cited 2016 Jul 30];247(6):994–1002. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18520227
Memeo R, de Blasi V, Adam R, Goéré D, Piardi T, Lermite E, et al. Margin status is still an important prognostic factor in hepatectomies for colorectal liver metastases: a propensity score matching analysis. World J Surg. 2017;
Andalib A, Ramana-Kumar A V, Bartlett G, Franco EL, Ferri LE. Influence of postoperative infectious complications on long-term survival of lung cancer patients: a population-based cohort study. J Thorac Oncol. 2013;8(5):554–61.
Doughtie CA, Edwards JD, Philips P, Agle SC, Scoggins CR, McMasters KM, et al. Infectious complications in combined colon resection and ablation of colorectal liver metastases. Am J Surg [Internet]. 2015;210(6):1185–91. Available from: https://doi.org/10.1016/j.amjsurg.2015.07.012
Haruki K, Shiba H, Fujiwara Y, Furukawa K, Wakiyama S, Ogawa M, et al. Negative impact of surgical site infection on long-term outcomes after hepatic resection for colorectal liver metastases. Anticancer Res [Internet]. 2013;33(4):1697–703. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23564818
Ruan DY, Lin ZX, Li Y, Jiang N, Li X, Wu DH, et al. Poor oncologic outcomes of hepatocellular carcinoma patients with intra-abdominal infection after hepatectomy. World J Gastroenterol. 2015;21(18):5598–606.
Hayashi T, Yoshikawa T, Aoyama T, Hasegawa S, Yamada T, Tsuchida K, et al. Impact of infectious complications on gastric cancer recurrence. Gastric Cancer. 2015;18(2):368–74.
Artinyan A, Orcutt ST, Anaya D A, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: A study of 12,075 patients. Ann Surg [Internet]. 2014;0(0):1–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25185465
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg [Internet]. 2005 Sep [cited 2016 Jul 29];242(3):326–41-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16135919
Hirai T, Yamashita Y, Mukaida H, Kuwahara M, Inoue H, Toge T. Poor prognosis in esophageal cancer patients with postoperative complications. Surg Today [Internet]. 1998 [cited 2016 Jul 29];28(6):576–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9681604
Lin J-K, Yueh T-C, Chang S-C, Lin C-C, Lan Y-T, Wang H-S, et al. The influence of fecal diversion and anastomotic leakage on survival after resection of rectal cancer. J Gastrointest Surg [Internet]. 2011 Dec [cited 2016 Jul 29];15(12):2251–61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22002413
Eberhardt JM, Kiran RP, Lavery IC. The impact of anastomotic leak and intra-abdominal abscess on cancer-related outcomes after resection for colorectal cancer: a case control study. Dis Colon Rectum [Internet]. 2009 Mar [cited 2016 Jul 29];52(3):380–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19333035
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg [Internet]. 2011 May [cited 2016 Jul 29];253(5):890–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21394013
Menetrier-Caux C, Montmain G, Dieu MC, Bain C, Favrot MC, Caux C, et al. Inhibition of the differentiation of dendritic cells from CD34(+) progenitors by tumor cells: role of interleukin-6 and macrophage colony-stimulating factor. Blood [Internet]. 1998 Dec 15 [cited 2016 Jul 29];92(12):4778–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9845545
Panis Y, Ribeiro J, Chrétien Y, Nordlinger B. Dormant liver metastases: an experimental study. Br J Surg [Internet]. 1992 Mar [cited 2016 Jul 30];79(3):221–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1555087
Xavier P, Belo L, Beires J, Rebelo I, Martinez-de-Oliveira J, Lunet N, et al. Serum levels of VEGF and TNF-alpha and their association with C-reactive protein in patients with endometriosis. Arch Gynecol Obstet [Internet]. 2006 Jan [cited 2016 Jul 30];273(4):227–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16208475
Tanigawa N, Amaya H, Matsumura M, Shimomatsuya T. Correlation between expression of vascular endothelial growth factor and tumor vascularity, and patient outcome in human gastric carcinoma. J Clin Oncol [Internet]. 1997 Feb [cited 2016 Jul 30];15(2):826–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9053510
Fondevila C, Metges JP, Fuster J, Grau JJ, Palacín A, Castells A, et al. p53 and VEGF expression are independent predictors of tumour recurrence and survival following curative resection of gastric cancer. Br J Cancer [Internet]. 2004 Jan 12 [cited 2016 Jul 30];90(1):206–15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14710231
Gruttadauria S, Saint Georges Chaumet M, Pagano D, Marsh JW, Bartoccelli C, Cintorino D, et al. Impact of blood transfusion on early outcome of liver resection for colorectal hepatic metastases. J Surg Oncol [Internet]. 2011 Feb [cited 2016 Jul 30];103(2):140–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21259247
Lundy J, Ford CM. Surgery, trauma and immune suppression. Evolving the mechanism. Ann Surg [Internet]. 1983 Apr [cited 2016 Jul 30];197(4):434–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6219640
Pessaux P, Regimbeau J-M, Dondéro F, Plasse M, Mantz J, Belghiti J. Randomized clinical trial evaluating the need for routine nasogastric decompression after elective hepatic resection. Br J Surg. 2007;94(3):297–303.
Wong-Lun-Hing EM, van Woerden V, Lodewick TM, et al. Abandoning Prophylactic Abdominal Drainage after Hepatic Surgery: 10 Years of No-Drain Policy in an Enhanced Recovery after Surgery Environment. Dig Surg. 2017;34(5):411–420.
Acknowledgments
The authors would like to thank all participating centers for their contribution to this study. Authors would also like to thank Christopher Burel, Iana Shutrova, and Guy Temporal, professional medical proofreaders, for their assistance in revising the manuscript. Contributors: Amiens, CHU Amiens Picardie: Cyril Cosse, Delphine Lignier, Jean Marc Regimbeau; Angers, CHU Angers: Julien Barbieux, Emilie Lermite, Antoine Hamy; Beauvais, CH Beauvais: François Mauvais; Bordeaux, Groupe Hospitalier Saint André: Christophe Laurent; Chambéry, CH Chambéry: Irchid Al Naasan; Créteil, CHU Henri Mondor: Alexis Laurent, Philippe Compagnon; Eaubonne, Hôpital Simone Veil: Mohammed Sbai Idrissi; Epinal, Polyclinique de la Ligne Bleue: Frédéric Martin; Gap, CH des Alpes du Sud: Jérôme Atger; Lyon, Hôpital de la Croix Rousse: Jacques Baulieux, Benjamin Darnis, Jean Yves Mabrut; Lyon, Hôpital Edouard Herriot: Vahan Kepenekian, Julie Perinel, Mustapha Adham; Lyon, CH Lyon Sud: Olivier Glehen; Lyon, Centre Léon Bérard: Michel Rivoire; Marseille, Hôpital de la Conception: Jean Hardwigsen, Anaïs Palen, Yves Patrice Le Treut; Marseille, Institut Paoli-Calmettes: Jean Robert Delpero, Olivier Turrini; Montpellier, Hôpital Saint Eloi: Astrid Herrero, Fabrizio Panaro; Nancy, CHU Brabois: Laurent Bresler; Nancy, Institut de Cancérologie de Lorraine Alexis-Vautrin: Philippe Rauch, François Guillemin, Frédéric Marchal; Nice, Hôpital de l’Archet: Jean Gugenheim, Antonio Iannelli; Kremlin-Bicêtre, CHU Kremlin-Bicêtre: Stéphane Benoist, Antoine Brouquet; Paris, Hôpital Lariboisière: Marc Pocard, Rea Lo Dico; Paris, Institut Mutualiste Montsouris: David Fuks; Paris, Hôpital Saint Antoine: Olivier Scatton, Olivier Soubrane; Paris, Hôpital de la Pitié Salpétrière: Jean-Christophe Vaillant; Reims, Hôpital Robert Debré: Tullio Piardi, Daniel Sommacale, Reza Kianmanesh; La Roche-sur-Yon, Centre Départemental de Vendée: Michel Comy; Strasbourg, Hôpital de Hautepierre: Philippe Bachelier, Elie Oussoultzoglou, Pietro Addeo; Strasbourg, Nouvel Hôpital Civil: Dimitrios Ntourakis, Didier Mutter, Jacques Marescaux; Toulouse, Hôpital Rangueil: Loïc Raoux, Bertrand Suc, Fabrice Muscari; Troyes, Hôpital des Hauts-Clos: Georges ELHOMSY; Villejuif, Hôpital Paul Brousse: Maximiliano Gelli, Denis Castaing, Daniel Cherqui; Gabriella PIttau, Oriana Ciacio, Eric Vibert; Villejuif, Gustave Roussy: Dominique Elias, Fabrizio Vittadello.
Author information
Authors and Affiliations
Consortia
Contributions
RM, VDB, RA, DG, AL, NDA, TP, EL, AH, FN, AS, PP contributed to the conception or design of the work;
RM, VDB, RA, DG contributed to the acquisition, analysis, or interpretation of data for the work;
RM, VDB, RA, DG, AL, NDA, TP, EL, AH, FN, AS, PP contributed to the drafting of the work and revising it critically for important intellectual content;
EL, AH, FN, AS, PP finally approved the version to be published;
Corresponding author
Ethics declarations
Disclosures
The authors have nothing to disclose.
Additional information
Collaborators of the French Surgical Association (Association Française de Chirurgie) Working Group are listed in Appendix 1.
Rights and permissions
About this article
Cite this article
Memeo, R., de Blasi, V., Adam, R. et al. Postoperative Infectious Complications Impact Long-Term Survival in Patients Who Underwent Hepatectomies for Colorectal Liver Metastases: a Propensity Score Matching Analysis. J Gastrointest Surg 22, 2045–2054 (2018). https://doi.org/10.1007/s11605-018-3854-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3854-2