Abstract
Background
Advances in the surgical management of hepatocellular carcinoma (HCC) have expanded the indications for curative hepatectomy, including more extensive liver resections. The purpose of this study was to examine long-term survival trends for patients treated with major hepatectomy for HCC.
Patients and Methods
Clinicopathologic data for 1,115 patients with HCC who underwent hepatectomy between 1981 and 2008 at five hepatobiliary centers in France, China, and the USA were assessed. In addition to other performance metrics, outcomes were evaluated using resection of ≥4 liver segments as a novel definition of major hepatectomy.
Results
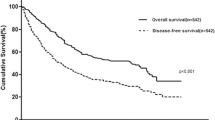
Major hepatectomy was performed in 539 patients. In the major hepatectomy group, median tumor size was 10 cm (range: 1–27 cm) and 22 % of the patients had bilateral lesions. The TNM Stage distribution included 29 % Stage I, 31 % Stage II, 38 % Stage III, and 2 % Stage IV. The postoperative histologic examination indicated that chronic liver disease was present in 35 % of the patients and tumor microvascular invasion was identified in 60 % of the patients. The 90-day postoperative mortality rate was 4 %. After a median follow-up time of 63 months, the 5-year overall survival rate was 40 %. Patients treated with right hepatectomy (n = 332) and those requiring extended hepatectomy (n = 207) had similar 90-day postoperative mortality rates (4 % and 4 %, respectively, p = 0.976) and 5-year overall survival rates (42 % and 36 %, respectively, p = 0.523). Postoperative mortality and overall survival rates after major hepatectomy were similar among the participating countries (p > 0.1) and improved over time with 5-year survival rates of 30 %, 40 %, and 51 % for the years 1981–1989, 1990–1999, and the most recent era of 2000–2008, respectively (p = 0.004). In multivariate analysis, factors that were significantly associated with worse survivals included AFP level >1,000 ng/mL, tumor size >5 cm, presence of major vascular invasion, presence of extrahepatic metastases, positive surgical margins, and earlier time period in which the major hepatectomy was performed.
Conclusions
This multinational, long-term HCC survival analysis indicates that expansion of surgical indications to include major hepatectomy is justified by the significant improvement in outcomes over the past three decades observed in both the East and the West.



Similar content being viewed by others
References
Ercolani G, Grazi GL, Ravaioli M, et al. Liver resection for hepatocellular carcinoma on cirrhosis: univariate and multivariate analysis of risk factors for intrahepatic recurrence. Ann Surg 2003; 237:536–543.
Poon RT, Fan ST, Lo CM, et al. Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 2001; 234:63–70.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334:693–699.
Livraghi T, Meloni F, Di Stasi M, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology 2008; 47:82–89.
Poon RT, Fan ST, Lo CM, et al. Extended hepatic resection for hepatocellular carcinoma in patients with cirrhosis: is it justified? Ann Surg 2002; 236:602–611.
Chik BH, Liu CL, Fan ST, et al. Tumor size and operative risks of extended right-sided hepatic resection for hepatocellular carcinoma: implication for preoperative portal vein embolization. Arch Surg 2007; 142:63–69.
Akai H, Kiryu S, Matsuda I, et al. Detection of hepatocellular carcinoma by Gd-EOB-DTPA-enhanced liver MRI: Comparison with triple phase 64 detector row helical CT. Eur J Radiol 2010.
Aloia TA, Zorzi D, Abdalla EK, et al. Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Ann Surg 2005; 242:172–177.
Donadon M, Abdalla EK, Vauthey JN. Liver hanging maneuver for large or recurrent right upper quadrant tumors. J Am Coll Surg 2007; 204:329–333.
Ishizawa T, Mise Y, Aoki T, et al. Surgical technique: new advances for expanding indications and increasing safety in liver resection for HCC: the Eastern perspective. J Hepatobiliary Pancreat Sci 2010; 17:389–393.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 2005; 12:351–355.
Dahiya D, Wu TJ, Lee CF, et al. Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: a 20-year experience. Surgery 2010; 147:676–685.
Capussotti L, Muratore A, Massucco P, et al. Major liver resections for hepatocellular carcinoma on cirrhosis: early and long-term outcomes. Liver Transpl 2004; 10:S64-68.
Ng KK, Vauthey JN, Pawlik TM, et al. Is hepatic resection for large or multinodular hepatocellular carcinoma justified? Results from a multi-institutional database. Ann Surg Oncol 2005; 12:364–373.
Wei AC, Tung-Ping Poon R, Fan ST, et al. Risk factors for perioperative morbidity and mortality after extended hepatectomy for hepatocellular carcinoma. Br J Surg 2003; 90:33–41.
Melendez J, Ferri E, Zwillman M, et al. Extended hepatic resection: a 6-year retrospective study of risk factors for perioperative mortality. J Am Coll Surg 2001; 192:47–53.
Zhou L, Rui JA, Wang SB, et al. Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J Surg 2007; 31:1782–1787.
Torzilli G, Makuuchi M, Inoue K, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg 1999; 134:984–992.
Fan ST, Mau Lo C, Poon RT, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma: a 20-year experience. Ann Surg 2011; 253:745–758.
Imamura H, Seyama Y, Kokudo N, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg 2003; 138:1198–1206.
Miyoshi A, Takahashi T, Otsuka T, et al. Efficacy of major hepatectomy for large hepatocellular carcinoma. Hepatogastroenterology 2009; 56:768–772.
Bismuth H. Surgical Anatomy and Anatomical Surgery of the Liver. World J Surg 1982; 6:3–9.
Vauthey JN, Chaoui A, Do KA, et al. Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery 2000; 127:512–519.
Kishi Y, Abdalla EK, Chun YS, et al. Three Hundred and One Consecutive Extended Right Hepatectomies: Evaluation of Outcome Based on Systematic Liver Volumetry. Ann Surg 2009.
Abdalla EK, Adam R, Bilchik AJ, et al. Improving resectability of hepatic colorectal metastases: Expert consensus statement. Ann Surg Oncol 2006; 13:1271–1280.
Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973; 60:646–649.
Zorzi D, Laurent A, Pawlik TM, et al. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg 2007; 94:274–286.
Leevy CM, Smith F, Longueville J, et al. Indocyanine green clearance as a test for hepatic function. Evaluation by dichromatic ear densitometry. JAMA 1967; 200:236–240.
Vauthey JN, Lauwers GY, Esnaola NF, et al. Simplified staging for hepatocellular carcinoma. J Clin Oncol 2002; 20:1527–1536.
Couinaud C. Le foie; études anatomiques et chirurgicales. Paris: Masson & Cie 1957.
Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 1954; 7:462–503.
Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol 1995; 22:696–699.
Ishizawa T, Hasegawa K, Aoki T, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 2008; 134:1908–1916.
Halazun KJ, Al-Mukhtar A, Aldouri A, et al. Right hepatic trisectionectomy for hepatobiliary diseases. Ann Surg 2007; 246:1065–1074.
Abdalla EK, Denys A, Chevalier P, et al. Total and segmental liver volume variations: implications for liver surgery. Surgery 2004; 135:404–410.
Mullen JT, Ribero D, Reddy SK, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg 2007; 204:854–862.
Kishi Y, Abdalla EK, Chun YS, et al. Three Hundred and One Consecutive Extended Right Hepatectomies: Evaluation of Outcome Based on Systematic Liver Volumetry. Ann Surg 2009; 250:540–548.
Esnaola NF, Mirza N, Lauwers GY, et al. Comparison of clinicopathologic characteristics and outcomes after resection in patients with hepatocellular carcinoma treated in the United States, France, and Japan. Ann Surg 2003; 238:711–719.
Kubota K, Makuuchi M, Kusaka K, et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology 1997; 26:1176–1181.
Azoulay D, Castaing D, Krissat J, et al. Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg 2000; 232:665–672.
Imamura H, Seyama Y, Makuuchi M, et al. Sequential transcatheter arterial chemoembolization and portal vein embolization for hepatocellular carcinoma: the university of Tokyo experience. Semin Intervent Radiol 2008; 25:146–154.
Yoo H, Kim JH, Ko GY, et al. Sequential Transcatheter Arterial Chemoembolization and Portal Vein Embolization versus Portal Vein Embolization Only before Major Hepatectomy for Patients with Hepatocellular Carcinoma. Ann Surg Oncol 2011; 18:1251–1257.
Ogata S, Belghiti J, Farges O, et al. Sequential arterial and portal vein embolizations before right hepatectomy in patients with cirrhosis and hepatocellular carcinoma. Br J Surg 2006; 93:1091–1098.
Choti MA, Geschwind JF. Preoperative Sequential TACE and PVE to Increase Resectability in the Cirrhotic Patient With HCC. Gastrointest Cancer Res 2008; 2:47–48.
Hwang S, Lee SG, Ko GY, et al. Sequential preoperative ipsilateral hepatic vein embolization after portal vein embolization to induce further liver regeneration in patients with hepatobiliary malignancy. Ann Surg 2009; 249:608–616.
Farges O, Malassagne B, Flejou JF, et al. Risk of major liver resection in patients with underlying chronic liver disease: a reappraisal. Ann Surg 1999; 229:210–215.
Sotiropoulos GC, Druhe N, Sgourakis G, et al. Liver transplantation, liver resection, and transarterial chemoembolization for hepatocellular carcinoma in cirrhosis: which is the best oncological approach? Dig Dis Sci 2009; 54:2264–2273.
Ruzzenente A, Capra F, Pachera S, et al. Is liver resection justified in advanced hepatocellular carcinoma? Results of an observational study in 464 patients. J Gastrointest Surg 2009; 13:1313–1320.
Ribero D, Abdalla EK, Madoff DC, et al. Portal vein embolization before major hepatectomy and its effects on regeneration, resectability and outcome. Br J Surg 2007; 94:1386–1394.
Farges O, Belghiti J, Kianmanesh R, et al. Portal vein embolization before right hepatectomy—Prospective clinical trial. Ann Surg 2003; 237:208–217.
AJCC Cancer Staging Manual Seventh Edition. New York: Springer, 2010.
Varotti G, Ramacciato G, Ercolani G, et al. Comparison between the fifth and sixth editions of the AJCC/UICC TNM staging systems for hepatocellular carcinoma: multicentric study on 393 cirrhotic resected patients. Eur J Surg Oncol 2005; 31:760–767.
Lei HJ, Chau GY, Lui WY, et al. Prognostic value and clinical relevance of the 6th edition 2002 American Joint Committee on Cancer staging system in patients with resectable hepatocellular carcinoma. J Am Coll Surg 2006; 203:426–435.
Vauthey JN, Ribero D, Abdalla EK, et al. Outcomes of liver transplantation in 490 patients with hepatocellular carcinoma: validation of a uniform staging after surgical treatment. J Am Coll Surg 2007; 204:1016–1027.
Pawlik TM, Poon RT, Abdalla EK, et al. Critical appraisal of the clinical and pathologic predictors of survival after resection of large hepatocellular carcinoma. Arch Surg 2005; 140:450–457.
Acknowledgments
The authors thank Stephanie Deming and Ruth J. Haynes for their assistance with manuscript preparation.
Funding sources
This study was supported, in part, by the National Institutes of Health through MD Anderson's Cancer Center Support Grant, CA016672.
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Discussant
Dr. Sharon Weber (Madison, WI): The authors are to be congratulated for this outstanding multi-institutional study. The improvements in overall survival and 90-day mortality over time are very encouraging, particularly since this is such a difficult patient population due to the large tumor size and underlying liver dysfunction.
Any HPB surgeon who reads this excellent manuscript will likely want to gain a better understanding of the specific changes that occurred over time to account for these fantastic results, particularly in regard to perioperative management and patient selection, in order to better assess how these factors impacted mortality and long-term outcome.
Specific perioperative parameters that should be included in your analyses include EBL, blood transfusions, use of low CVP anesthesia, and use of the Pringle for liver transection, as these factors have been found to have a significant impact on perioperative mortality and, for some of these factors, also on survival.
In addition, can you help us understand how better assessment of liver reserve may have impacted perioperative mortality? How often was PVE or CT volumetry utilized, and were patients excluded from consideration for resection if they were unable to grow their remnant liver following PVE?
Many other series analyzing long-term results following complex resections for cancer have found a detrimental effect of complications on overall survival. I understand why you did not include that data here, but it would be very useful to assess this in order for us to understand the significance of complications relative to the other negative prognostic indicators you have nicely outlined in the paper. This is particularly relevant, since, to some degree, it is more controllable than tumor-specific factors like AFP level, tumor size, and vascular invasion.
Finally, did the improvement in mortality apply to patients with and without cirrhosis? Attempting to better understand the independent predictors of 90-day mortality are so important for this disease; thus, it would be very useful to include a multivariable analysis of predictors of mortality in the final MS.
Again, congratulations on an excellent paper.
Closing Discussant
Dr. Andreas Andreou: On behalf of the authors, I would like to thank Dr. Weber for her positive comments and interesting questions.
In regard to the inquiry about specific factors that have changed over time and may directly account for improved survival, it is difficult to separate the multiple components. Undoubtedly, there have been contributions in the areas of preoperative imaging, patient selection, surgical techniques, and anesthetic monitoring that have increased the safety of liver resection and contributed to forward progress. However, the design of this large multicenter study, which extended over a long period of time, did not allow for analysis of specific perioperative parameters such as EBL, blood transfusions, and use of low CVP anesthesia.
As our study focused on major hepatectomy, one of the most meaningful advances that occurred over time was likely in the area of evaluating the future liver remnant (FLR). With modern cross-sectional imaging, configuration, contour, and volume of the FLR can now be reliably assessed. More recently, the ability to additionally measure the functional capacity of the FLR, through either the indocyanine green clearance test or via hypertrophic response to portal vein embolization, has significantly impacted patient selection and postoperative liver failure rates. Although each center approached FLR evaluation with a unique strategy, the universal development of FLR assessment is certainly a key factor contributing to their shared successes.
In reference to your excellent question regarding the impact of complications on survival, we have reassessed the 90-day outcomes in this study. Although we do not have sufficient detail regarding specific complications to individually report them, the 90-day survival may act as a useful surrogate to differentiate meaningful complications from recoverable complications. The 90-day postoperative mortality rate for all patients undergoing major hepatectomy was 4 %, and it did not differ between patients who underwent right and those who underwent extended hepatectomy (p = 0.976; Table 1). However, an analysis according to both extent of resection and underlying liver disease showed that whereas fibrosis or cirrhosis did not negatively affect the 90-day mortality of patients undergoing right hepatectomy (p = 0.940), the presence of fibrosis or cirrhosis was associated with worse 90-day mortality rate among patients treated with extended hepatectomy (p = 0.002; Table 4).
Our additional analysis of early outcomes identified major vascular resection and earlier time period for resection as the two independent factors associated with 90-day survival. Interestingly, underlying liver disease in the form of fibrosis or cirrhosis was not a significant factor. Taken together, these data suggest that underlying liver disease has its largest impact when resection requires extended hepatectomy and/or major vascular resection.
Rights and permissions
About this article
Cite this article
Andreou, A., Vauthey, JN., Cherqui, D. et al. Improved Long-Term Survival after Major Resection for Hepatocellular Carcinoma: A Multicenter Analysis Based on a New Definition of Major Hepatectomy. J Gastrointest Surg 17, 66–77 (2013). https://doi.org/10.1007/s11605-012-2005-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2005-4