Abstract
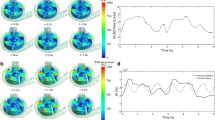
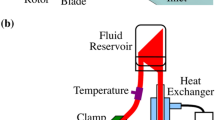
Until recent years, it was almost beyond remedy to save the life of end-stage heart failure patients without considering a heart transplant. This is while the need for healthy organs has always far exceeded donations. However, the evolution of VAD technology has certainly changed the management of these patients. Today, blood pumps are designed either pulsatile flow or continuous flow, each of which has its own concerns and limitations. For instance, pulsatile pumps are mostly voluminous and hardly can be used for children. On the other hand, the flow generated by continuous-flow pumps is in contrast with pulsatile flow of the natural heart. In this project, having used computational fluid dynamics, we studied the possibility of generating pulsatile blood flow via a continuous-flow blood pump by adjusting the rotational speed of the pump with two distinct patterns (sinusoidal and trapezoidal), both of which have been proposed and set based on physiological needs and blood flow waveform of the natural heart. An important feature of this study is setting the outlet pressure of the pump similar to the physiological conditions of a patient with heart failure, and since these axial pumps are sensitive to outlet pressures, more secure and reliable results of their performance are achieved. Our results show a slight superiority of a sinusoidal pattern compared to a trapezoidal one with the potential to achieve an adequate pulsatile flow by precisely controlling the rotational speed.















Similar content being viewed by others
References
Agarwal S, High KM (2012) Newer-generation ventricular assist devices. Best Pract Res Clin Anaesthesiol 26:117–130
ANSYS CFX-solver theory guide (2009) ANSYS, Inc., Canonsburg, PA
Apel J, Paul R, Klaus S, Siess T, Reul H (2001) Assessment of hemolysis related quantities in a microaxial blood pump by computational fluid dynamics. Artif Organs 25:341–347
Arora D, Behr M, Pasquali M (2006) Hemolysis estimation in a centrifugal blood pump using a tensor-based measure. Artif Organs 30:539–547
Boyle AJ, Ascheim DD, Russo MJ, Kormos RL, John R, Naka Y, Gelijns AC, Hong KN, Teuteberg JJ (2011) Clinical outcomes for continuous-flow left ventricular assist device patients stratified by pre-operative INTERMACS classification. J Heart Lung Transplant 30:402–407
Burgreen GW, Antaki JF, Griffith BP (1996) A design improvement strategy for axial blood pumps using computational fluid dynamics. ASAIO J 42:M354–M359
Centrigugal LVAS (2016). Evaheart Inc., Houston, TX
Chan W, Wong Y, Ding Y, Chua L, Yu S (2002) Numerical investigation of the effect of blade geometry on blood trauma in a centrifugal blood pump. Artif Organs 26:785–793
Cheng A, Williamitis CA, Slaughter MS (2014) Comparison of continuous-flow and pulsatile-flow left ventricular assist devices: is there an advantage to pulsatility? Ann Cardiothorac Surg 3:573
Corbett SC, Ajdari A, Coskun AU, Nayeb-Hashemi H (2010) Effect of pulsatile blood flow on thrombosis potential with a step wall transition. ASAIO J 56:290–295
Dexter EU, Aluri S, Radcliffe RR, Zhu H, Carlson DD, Heilman TE, Chandran KB, Richenbacher WE (1999) In vivo demonstration of cavitation potential of a mechanical heart valve. ASAIO J 45:436–441
Feller ED, Sorensen EN, Haddad M, Pierson RN, Johnson FL, Brown JM, Griffith BP (2007) Clinical outcomes are similar in pulsatile and nonpulsatile left ventricular assist device recipients. Ann Thorac Surg 83:1082–1088
Frazier O, Khalil HA, Benkowski RJ, Cohn WE (2010) Optimization of axial-pump pressure sensitivity for a continuous-flow total artificial heart. J Heart Lung Transplant 29:687–691
Hayward CS, Salamonsen R, Keogh AM, Woodard J, Ayre P, Prichard R, Walker R, Kotlyar E, Macdonald PS, Jansz P (2011) Effect of alteration in pump speed on pump output and left ventricular filling with continuous-flow left ventricular assist device. ASAIO J 57:495–500
HeartMate I (2012) LVAS operating manual. Thoratec Corporation, Pleasanton, CA, 171:e7
Heuser G, Opitz R (1980) A Couette viscometer for short time shearing of blood. Biorheology 17:17
Kato TS, Chokshi A, Singh P, Khawaja T, Cheema F, Akashi H, Shahzad K, Iwata S, Homma S, Takayama H (2011) Effects of continuous-versus pulsatile-flow left ventricular assist devices on myocardial unloading and remodeling. Circ Heart Fail 4:546
Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson L, Miller M, Young JB (2012) Long-term mechanical circulatory support (destination therapy): on track to compete with heart transplantation? J Thorac Cardiovasc Surg 144:584–603
Kirklin JK, Naftel DC, Kormos RL, Stevenson LW, Pagani FD, Miller MA, Baldwin JT, Young JB (2013) Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J Heart Lung Transplant 32:141–156
Klotz S, Deng MC, Stypmann J, Roetker J, Wilhelm MJ, Hammel D, Scheld HH, Schmid C (2004) Left ventricular pressure and volume unloading during pulsatile versus nonpulsatile left ventricular assist device support. Ann Thorac Surg 77:143–149
Laskey W, Kussmaul W (1987) Arterial wave reflection in heart failure. Circulation 75:711–722
Margulies KB, Rame JE (2011) Adaptations to pulsatile versus nonpulsatile ventricular assist device support. Circ Heart Fail 4:535–537
Miyazoe Y, Sawairi T, Ito K, Konishi Y, Yamane T, Nishida M, Asztalos B, Masuzawa T, Tsukiya T, Endo S, Taenaka Y (1999) Computational fluid dynamics to establish the design process of a centrifugal blood pump: second report. Artif Organs 23:762–768
Moazami N, Dembitsky W, Adamson R, Steffen R, Soltesz E, Starling R, Fukamachi K (2015) Does pulsatility matter in the era of continuous-flow blood pumps? J Heart Lung Transplant 34:999–1004
Murphy SL, Xu J, Kochanek KD (2013) Deaths: final data for 2010. Natl Vital Stat Rep 61:1–118
Park SJ, Tector A, Piccioni W, Raines E, Gelijns A, Moskowitz A, Rose E, Holman W, Furukawa S, Frazier OH (2005) Left ventricular assist devices as destination therapy: a new look at survival. J Thorac Cardiovasc Surg 129:9–17
Pirbodaghi T, Axiak S, Weber A, Gempp T, Vandenberghe S (2012) Pulsatile control of rotary blood pumps: does the modulation waveform matter? J Thorac Cardiovasc Surg 144:970–977
Prosi M, Perktold K, Schima H (2007) Effect of continuous arterial blood flow in patients with rotary cardiac assist device on the washout of a stenosis wake in the carotid bifurcation: a computer simulation study. J Biomech 40:2236–2243
Sansone F, Zingarelli E, Flocco R, Dato GMA, Parisi F, Punta G, Forsennati PG, Bardi GL, del Ponte S, Patanè F (2012) Pulsed or continuous flow in long-term assist devices: a debated topic. Transplant Rev 26:241–245
Schmid C, Tjan TD, Etz C, Schmidt C, Wenzelburger F, Wilhelm M, Rothenburger M, Drees G, Scheld HH (2005) First clinical experience with the Incor left ventricular assist device. J Heart Lung Transplant 24:1188–1194
Shahraki ZH, Oscuii HN (2014) Numerical investigation of three patterns of motion in an electromagnetic pulsatile VAD. ASAIO J 60:304–310
Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, Sun B, Tatooles AJ, Delgado RM III, Long JW (2009) Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med 361:2241–2251
Soucy KG, Koenig SC, Giridharan GA, Sobieski MA, Slaughter MS (2013) Rotary pumps and diminished pulsatility: do we need a pulse? ASAIO J 59:355–366
Untaroiu A (2006) LEV-VAD2 Axial Flow blood pump optimized flow path design by means of computational fluid dynamics. University of Virginia, USA
White FM, Corfield I (1991) Viscous fluid flow, vol 3. McGraw-Hill, New York
Wieselthaler GM, Schima H, Hiesmayr M, Pacher R, Laufer G, Noon GP, DeBakey M, Wolner E (2000) First clinical experience with the DeBakey VAD continuous-axial-flow pump for bridge to transplantation. Circulation 101:356–359
Qian Y, Bertram CD (2000) Computational fluid dynamics analysis of hydrodynamic bearings of the VentrAssist rotary blood pump. Artif Organs 24:488–491
Yano T, Sekine K, Mitoh A, Mitamura Y, Okamoto E, Kim DW, Nishimura I, Murabayashi S, Yozu R (2003) An estimation method of hemolysis within an axial flow blood pump by computational fluid dynamics analysis. Artif Organs 27:920–925
Acknowledgments
The authors would like to acknowledge the help of the members of Computational Biomechanical Laboratory of Sahand University of Technology for their collaboration and without them the project would not be possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Nammakie, E., Niroomand-Oscuii, H., Koochaki, M. et al. Computational fluid dynamics-based study of possibility of generating pulsatile blood flow via a continuous-flow VAD. Med Biol Eng Comput 55, 167–178 (2017). https://doi.org/10.1007/s11517-016-1523-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-016-1523-8