Abstract
Background
As more adults undergo surgical fixation of clavicle fractures with improved outcomes, interest is renewed in managing clavicle fractures in adolescents. The medial clavicular physis does not fuse until 23 to 25 years of age, but studies report minimal clavicular growth during adolescence—studies that employed cross-sectional methodologies, which cannot not capture growth in patients over time. The assumption that clavicle length at each stage is uniform, as is the final overall length, may not be accurate if the age groups studied comprise various ethnicities, socioeconomic status, or height.
Questions/Purposes
We sought to quantify longitudinal clavicular growth on serial radiographs in adolescents and young adults. Our hypothesis was that substantial clavicular growth would be seen beyond the age of 12 years.
Methods
We conducted a longitudinal case series of non-syndromic patients in a single orthopedic clinic and analyzed serial radiographic images of the clavicles. For ethical reasons, only patients with non-neuromuscular scoliosis and kyphosis (in whom the existing standard of care includes serial thoracic radiographs) were considered for inclusion. Patients ages 10 to 25 years old were included in the study if three or more serial thoracic radiographs over a minimum 5 years were available that captured the entire length of at least one non-rotated clavicle. Three types of radiographs were included for analysis: digital low-dose-radiation stereoradiographic (EOS Imaging, Paris, France), non-EOS digital, and non-EOS printed. The overall longitudinal growth, yearly growth, and the yearly growth percentage were calculated for each clavicle.
Results
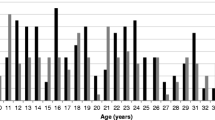
Fifty-seven patients (22 male and 35 female) met the inclusion criteria. In male patients, at ages 12 to 15 years, the clavicular growth was 4.9 mm/year, or 4%/year; at ages 16 to 19 years, growth was 3.2 mm/year, or 2.4%/year; and at ages 20 to 25 years, growth was 1.7 mm/year, or 1.1%/year. In female patients, at ages 12 to 15 years, growth was 4.7 mm/year, or 4%/year; at 16 to 19 years, growth was 2.2 mm/year, or 1.7%/year; and at ages 20 to 25 years, growth was 0.2 mm/year or 0.1%/year. We could not detect the age of terminal growth in either sex because growth was ongoing in most patients in the oldest group.
Conclusion
We found substantial clavicular growth potential after age 18 years, when growth is thought to be nearly finished, as well as remodeling potential even up to age 25 years. Further research is needed, but our findings suggest that strategies for managing clavicle fracture in adults may not be applied universally to adolescents and young adults.





Similar content being viewed by others
References
Abraham E. Remodeling potential of long bones following angular osteotomies. J Pediatr Orthop. 1989;9(1):37–43.
Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013;33(5):544–550.
Black S, Scheuer L. Age changes in the clavicle: from the early neonatal period to skeletal maturity. Int J Osteoarchaeol. 1996;6(5):425–434.
Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1–10.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284.
Glaser DA, Doan J, Newton PO. Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976). 2012;37(16):1391–1397.
Heyworth BE, Kocher MS. Shoulder instability in the young athlete. Instr Course Lect. 2013;62:435–444.
Heyworth B, Suppan C, Kocher M. Change in the volume of operative treatment of clavicle fractures in children and adolescents: national trends and practice patterns. American Orthopaedic Society for Sports Medicine; 2014.
Jit I, Kulkarni M. Times of appearance and fusion of epiphysis at the medial end of the clavicle. Indian J Med Res. 1976;64(5):773–782.
Li Y, Donohue KS, Robbins CB, et al. Reliability of radiographic assessments of adolescent midshaft clavicle fractures by the FACTS Multicenter Study Group. J Orthop Trauma. 2017;31(9):479–484.
Matsumura N, Ikegami H, Nakamichi N, et al. Effect of shortening deformity of the clavicle on scapular kinematics: a cadaveric study. Am J Sports Med. 2010;38(5):1000–1006.
McGraw MA, Mehlman CT, Lindsell CJ, Kirby CL. Postnatal growth of the clavicle: birth to 18 years of age. J Pediatr Orthop. 2009;29(8):937–943.
McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675–684.
Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851–855.
Melhem E, Assi A, El Rachkidi R, Ghanem I. EOS® biplanar X-ray imaging: concept, developments, benefits, and limitations. J Child Orthop. 2016;10(1):1–14.
Pandya NK, Namdari S, Hosalkar HS. Displaced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20(8):498–505.
Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg. Am. 2013;95(13):1159–1165.
Shah RR, Kinder J, Peelman J, Moen TC, Sarwark J. Pediatric clavicle and acromioclavicular injuries. J Pediatr Orthop. 2010;30:S69–S72.
Suppan CA, Bae DS, Donohue KS, Miller PE, Kocher MS, Heyworth BE. Trends in the volume of operative treatment of midshaft clavicle fractures in children and adolescents: a retrospective, 12-year, single-institution analysis. J Pediatr Orthop. B. 2016;25(4):305–309.
Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30(4):307–312.
Wallace ME, Hoffman EB. Remodelling of angular deformity after femoral shaft fractures in children. J. Bone Joint Surg. Br. 1992;74(5):765–769.
Wilkins KE. Principles of fracture remodeling in children. Injury. 2005;36 Suppl 1:A3–A11.
Yang S, Werner BC, Gwathmey FW Jr. Treatment trends in adolescent clavicle fractures. J Pediatr Orthop. 2015;35(3):229–233.
Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD, Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504–507.
Funding
This study was supported by Rady Children’s Hospital, San Diego, Division of Orthopedics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tracey Bastrom, MS, declares no conflicts of interest. Jessica L. Hughes, MD, reports personal fees or other material support from Depuy Synthes, Medical Device Business Services, Axogen, Stryker, Globus Medical, and Sanofi-Aventis, outside the submitted work. Peter O. Newton, MD, reports personal fees or other material support from Nuvasive, Zimmer Biomet, K2M, Medtronic USA, Merck Sharp & Dohme Corp., Globus Medical, Ethicon, and Depuy Synthes, outside the submitted work. Peter D. Fabricant, MD, MPH, reports personal fees or other material or nonfinancial support from Smith & Nephew, Medical Device Business Services, and Arthrex, and personal fees and board membership from Clinical Orthopedics and Related Research, Pediatric Orthopedic Society of North America, Pediatric Research in Sports Medicine Society, and Research in OsteoChondritis of the Knee (ROCK), outside the submitted work. Andrew T. Pennock, MD, reports personal fees or other material support from Stryker, Sportstek Medical, Orthopediatrics, Smith & Nephew; personal fees and board membership from American Orthopedic Society for Sports Medicine and Pediatric Orthopedic Society of North America; and stock or stock options from Imagen, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was obtained from all patients for being included in this study.
Required Author Forms:
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: Level IV: Retrospective case series
Rights and permissions
About this article
Cite this article
Hughes, J.L., Newton, P.O., Bastrom, T. et al. The Clavicle Continues to Grow During Adolescence and Early Adulthood. HSS Jrnl 16 (Suppl 2), 372–377 (2020). https://doi.org/10.1007/s11420-020-09754-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-020-09754-8