Abstract
Background
The treatment of postoperative pain is a challenge after posterior spinal fusions. Pain management using predominantly opioids is often associated with multiple adverse effects, while multimodal postoperative analgesia may provide adequate pain relief with fewer opioid side effects.
Questions/Purposes
The purpose of this review is to determine whether addition of 150 mg pregabalin daily would reduce narcotic requirements and improve outcomes after posterior lumbar fusion (PLF).
Methods
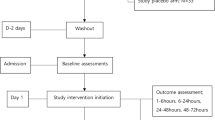
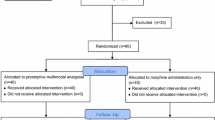
The method used is a randomized, controlled trial of elective PLF patients who received pregabalin or placebo. With institutional review board (IRB) approval, 86 patients undergoing elective posterior lumbar fusion, ASA I–III, were randomized to receive either a placebo or pregabalin after obtaining written informed consent. Both arms, i.e., placebo and pregabalin, consisted of 43 patients each.
The 86 patients for elective PLF were randomly assigned to receive 150 mg of pregabalin 1 h before surgery and then 150 mg daily, or a placebo tablet. All patients received a similar general anesthetic and in the post-anesthesia care unit (PACU), started on intravenous (IV) patient-controlled analgesia (PCA) of hydromorphone (0.2 mg/ml). Postoperative pain was assessed daily until discharge using a Numerical Rating Scale (NRS) at rest and with physical therapy (PT). Patients were also assessed twice daily for level of sedation and nausea and/or vomiting and expected PT milestones. All narcotics (IV, oral) were documented.
Results
Demographics and operative time between groups were similar. PCA hydromorphone administration and oral narcotic intake were not statistically different between the two groups. However, an increased incidence of nausea and vomiting in the placebo group reached statistical significance (p < 0.05). In addition, there was no statistical difference between groups with respect to achieving PT milestones and hospital discharge day.
Conclusion
After PLF, patients receiving pregabalin 150 mg/day did not have reduced IV narcotic usage, improved PT milestones, or reduced length of hospital stay. We were unable to demonstrate an analgesic advantage to prescribing pregabalin to patients undergoing lumbar spinal fusions.


Similar content being viewed by others
References
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97:534–40, table of contents.
Buvanendran A, Kroin JS, Della Valle CJ, Kari M, Moric M, Tuman KJ. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesth Analg. 2010; 110:199–207. https://doi.org/10.1213/ANE.0b013e3181c4273a.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014; 112:991–1004. https://doi.org/10.1093/bja/aeu137.
Gajraj NM. Pregabalin for pain management. Pain Pract. 2005; 5:95–102.
Gajraj NM. Pregabalin: its pharmacology and use in pain management. Anesth Analg. 2007; 105:1805–15.
Gianesello L, Pavoni V, Barboni E, Galeotti I, Nella A. Perioperative pregabalin for postoperative pain control and quality of life after major spinal surgery. J Neurosurg Anesthesiol. 2012; 24:121–6.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Khurana G, Jindal P, Sharma JP, Bansal KK. Postoperative pain and long-term functional outcome after administration of gabapentin and pregabalin in patients undergoing spinal surgery. Spine (Phila Pa 1976). 2014; 39:E363–8. https://doi.org/10.1097/BRS.0000000000000185.
Kim JC, Choi YS, Kim KN, Shim JK, Lee JY, Kwak YL. Effective dose of peri-operative oral pregabalin as an adjunct to multimodal analgesic regimen in lumbar spinal fusion surgery. Spine (Phila Pa 1976). 2011; 36:428–33. https://doi.org/10.1097/BRS.0b013e3181d26708.
Li Q, Zhang Z, Cai Z. High-dose ketorolac affects adult spinal fusion: a meta-analysis of the effect of perioperative nonsteroidal anti-inflammatory drugs on spinal fusion. Spine (Phila Pa 1976). 2011; 36:E461–8. https://doi.org/10.1097/BRS.0b013e3181dfd163.
Mathiesen O, Dahl B, Thomsen BA, Kitter B, Sonne N, Dahl JB et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J. 2013; 22:2089–96. https://doi.org/10.1007/s00586-013-2826-1.
Mathiesen O, Jacobsen LS, Holm HE, Randall S, Adamiec-Malmstroem L, Graungaard BK et al. Pregabalin and dexamethasone for postoperative pain control: a randomized controlled study in hip arthroplasty. Br J Anaesth. 2008; 101:535–41. https://doi.org/10.1093/bja/aen215.
Singla NK, Chelly JE, Lionberger DR, Gimbel J, Sanin L, Sporn J et al. Pregabalin for the treatment of postoperative pain: results from three controlled trials using different surgical models. J Pain Res. 2015; 8:9–20. https://doi.org/10.2147/JPR.S67841.
Tiippana EM, Hamunen K, Kontinen VK, Kalso E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg. 2007; 104:1545–56, table of contents. https://doi.org/10.1213/01.ane.0000261517.27532.80.
Urban MK, Yadeau JT, Lipnitsky JY. Ketamine as an adjunct to postoperative pain management in opioid tolerant patients after spinal fusions: A prospecitve randomized trial. HSS J 2008;4(1)62–65. https://doi.org/10.1007/s11420-007-9069-9.
White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005; 101:S5–22.
White PF. Multimodal analgesia: its role in preventing postoperative pain. Curr Opin Investig Drugs. 2008; 9:76–82.
White PF, Kehlet H. Improving postoperative pain management: what are the unresolved issues? Anesthesiology. 2010; 112:220–5. https://doi.org/10.1097/ALN.0b013e3181c6316e.
Yu L, Ran B, Li M, Shi Z. Gabapentin and pregabalin in the management of postoperative pain after lumbar spinal surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976). 2013; 38:1947–52. https://doi.org/10.1097/BRS.0b013e3182a69b90.
Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Br J Anaesth. 2011; 106:454–62. https://doi.org/10.1093/bja/aer027.
Acknowledgements
We would like to thank Kara Fields, MS, for assistance with data analysis and creating Fig. 2.
Funding
This study was funded by Hospital for Special Surgery Anesthesiology Department Research and Education Fund, New York, NY. REDCap, used to record physical therapy milestone data, was funded by the CTSC grant (grant number UL1 TR000457-06) from the National Center for Advancing Translational Sciences, National Institutes of Health, Bethesda, MD. Pfizer (New York, NY) provided the placebo and pregabalin medications.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Michael K. Urban, MD, PhD; Kristy M. Labib, MD; Shane C. Reid, MBS, BA; Amanda K. Goon, BA; and Valeria Rotundo have declared that they have no conflict of interest. Frank P. Cammisa Jr., MD reports royalties for patent with NuVasive. Federico P. Girardi, MD reports royalties paid for patents with DePuy Spine, LANX, Inc., NuVasive, and Ortho Development Corp., outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: Level II: Randomized Controlled Trial.
Work performed at Hospital for Special Surgery, New York, NY.
Rights and permissions
About this article
Cite this article
Urban, M.K., Labib, K.M., Reid, S.C. et al. Pregabalin Did Not Improve Pain Management After Spinal Fusions. HSS Jrnl 14, 41–46 (2018). https://doi.org/10.1007/s11420-017-9584-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-017-9584-2