Abstract
Purpose
Obstructive sleep apnea (OSA) is a complex sleep disorder associated with autonomic and sympathetic dysregulation. To the contrary, catestatin, an endogenous pleiotropic peptide cleaved from chromogranin A, is known for its inhibitory effects on catecholamine release and sympathetic activity. The aims of the study were to determine catestatin serum levels among male OSA patients compared to healthy control subjects and to explore associations of catestatin with anthropometric, polysomnographic, and lipid profile parameters.
Methods
Seventy-eight male OSA patients aged 50.3 ± 8.8 years and 51 age/sex/BMI-matched control subjects aged 50.4 ± 7.8 years were enrolled in the study. Catestatin serum levels were determined by an enzyme-linked immunosorbent assay (ELISA).
Results
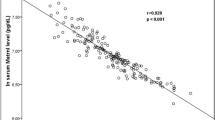
Catestatin serum levels were significantly higher among OSA patients compared to control subjects (2.9 ± 1.2 vs. 1.5 ± 1.1 ng/mL, p < 0.001). Serum catestatin levels significantly correlated with apnea-hypopnea index (AHI) among non-obese OSA subjects (r = 0.466, p = 0.016; β = 0.448, p = 0.026), while in whole OSA population, catestatin levels significantly correlated with neck circumference (r = 0.318, p < 0.001; β = 0.384, p < 0.001) and high-density lipoprotein (HDL) cholesterol (r = − 0.320, p < 0.001; β = − 0.344, p < 0.001). In multivariate-adjusted regression model, serum catestatin was significant and independent predictor of OSA status (OR 4.98, 95% CI 2.17–11.47, p < 0.001).
Conclusions
Catestatin serum levels are significantly increased in male OSA population and positively correlate with disease severity in non-obese patients. OSA status is independently predicted by catestatin levels; however, this finding is restricted to patients with moderate-to-severe disease. Further studies are necessary to elucidate the mechanistic role of catestatin in the complex pathophysiology of OSA.

Similar content being viewed by others
References
Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RD, Somers VK, Lavie L, Pépin J-L (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 1:15015. https://doi.org/10.1038/nrdp.2015.15
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008, Circulation) Sleep Apnea and Cardiovascular Disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement From the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In Collaboration With the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). 118(10):1080–1111. https://doi.org/10.1161/CIRCULATIONAHA.107.189375
Galic T, Bozic J, Ivkovic N, Gunjaca G, Ticinovic TK, Dogas Z (2016) Effects of mandibular advancement device treatment on arterial stiffness and glucose metabolism in patients with mild to moderate obstructive sleep apnea: a prospective 1 year study. Sleep Breath 20(1):69–77. https://doi.org/10.1007/s11325-015-1186-y
Kent BD, McNicholas WT, Ryan S (2015) Insulin resistance, glucose intolerance and diabetes mellitus in obstructive sleep apnoea. J Thorac Dis 7(8):1343–1357. https://doi.org/10.3978/j.issn.2072-1439.2015.08.11
Bozic J, Galic T, Supe-Domic D, Ivkovic N, Ticinovic Kurir T, Valic Z, Lesko J, Dogas Z (2016) Morning cortisol levels and glucose metabolism parameters in moderate and severe obstructive sleep apnea patients. Endocrine 53(3):730–739. https://doi.org/10.1007/s12020-016-0925-6
Adedayo AM, Olafiranye O, Smith D, Hill A, Zizi F, Brown C, Jean-Louis G (2014) Obstructive sleep apnea and dyslipidemia: evidence and underlying mechanism. Sleep Breath 18(1):13–18. https://doi.org/10.1007/s11325-012-0760-9
Nadeem R, Singh M, Nida M, Waheed I, Khan A, Ahmed S, Naseem J, Champeau D (2014) Effect of obstructive sleep apnea hypopnea syndrome on lipid profile: a meta-regression analysis. J Clin Sleep Med 10(5):475–489. https://doi.org/10.5664/jcsm.3690
Galic T, Bozic J, Pecotic R, Ivkovic N, Valic M, Dogas Z (2016) Improvement of cognitive and psychomotor performance in patients with mild to moderate obstructive sleep apnea treated with mandibular advancement device: a prospective 1-year study. J Clin Sleep Med 12(2):177–186. https://doi.org/10.5664/jcsm.5480
Troger J, Theurl M, Kirchmair R, Pasqua T, Tota B, Angelone T, Cerra MC, Nowosielski Y, Matzler R, Troger J, Gayen JR, Trudeau V, Corti A, Helle KB (2017) Granin-derived peptides. Prog Neurobiol 154:37–61. https://doi.org/10.1016/j.pneurobio.2017.04.003
Mahata SK, O'Connor DT, Mahata M, Yoo SH, Taupenot L, Wu H, Gill BM, Parmer RJ (1997) Novel autocrine feedback control of catecholamine release. A discrete chromogranin a fragment is a noncompetitive nicotinic cholinergic antagonist. J Clin Invest 100(6):1623–1633. https://doi.org/10.1172/jci119686
Mahata SK, Mahata M, Fung MM, O'Connor DT (2010) Catestatin: a multifunctional peptide from chromogranin A. Regul Pept 162(1–3):33–43. https://doi.org/10.1016/j.regpep.2010.01.006
Kojima M, Ozawa N, Mori Y, Takahashi Y, Watanabe-Kominato K, Shirai R, Watanabe R, Sato K, Matsuyama TA, Ishibashi-Ueda H, Koba S, Kobayashi Y, Hirano T, Watanabe T (2018) Catestatin prevents macrophage-driven atherosclerosis but not arterial injury-induced neointimal hyperplasia. Thromb Haemost 118(1):182–194. https://doi.org/10.1160/th17-05-0349
Durakoglugil ME, Ayaz T, Kocaman SA, Kirbas A, Durakoglugil T, Erdogan T, Cetin M, Sahin OZ, Cicek Y (2015) The relationship of plasma catestatin concentrations with metabolic and vascular parameters in untreated hypertensive patients: influence on high-density lipoprotein cholesterol. Anatol J Cardiol 15(7):577–585. https://doi.org/10.5152/akd.2014.5536
Bandyopadhyay GK, Mahata SK (2017) Chromogranin A regulation of obesity and peripheral insulin sensitivity. Front Endocrinol (Lausanne) 8:20. https://doi.org/10.3389/fendo.2017.00020
O'Connor DT, Kailasam MT, Kennedy BP, Ziegler MG, Yanaihara N, Parmer RJ (2002) Early decline in the catecholamine release-inhibitory peptide catestatin in humans at genetic risk of hypertension. J Hypertens 20(7):1335–1345
Li J, Thorne LN, Punjabi NM, Sun CK, Schwartz AR, Smith PL, Marino RL, Rodriguez A, Hubbard WC, O'Donnell CP, Polotsky VY (2005) Intermittent hypoxia induces hyperlipidemia in lean mice. Circ Res 97(7):698–706. https://doi.org/10.1161/01.RES.0000183879.60089.a9
Li J, Grigoryev DN, Ye SQ, Thorne L, Schwartz AR, Smith PL, O'Donnell CP, Polotsky VY (2005) Chronic intermittent hypoxia upregulates genes of lipid biosynthesis in obese mice. J Appl Physiol (1985) 99(5):1643–1648. https://doi.org/10.1152/japplphysiol.00522.2005
Qian Y, Yi H, Zou J, Meng L, Tang X, Zhu H, Yu D, Zhou H, Su K, Guan J, Yin S (2016) Independent association between sleep fragmentation and dyslipidemia in patients with obstructive sleep apnea. Sci Rep 6:26089. https://doi.org/10.1038/srep26089
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G (2013) Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol 62(7):569–576. https://doi.org/10.1016/j.jacc.2013.05.045
Kim J, Lee S, Bhattacharjee R, Khalyfa A, Kheirandish-Gozal L, Gozal D (2010) Leukocyte telomere length and plasma catestatin and myeloid-related protein 8/14 concentrations in children with obstructive sleep apnea. Chest 138(1):91–99. https://doi.org/10.1378/chest.09-2832
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Bassetti CL, Đogaš Z, Peigneux P (2014) European Sleep Research Society (ESRS) European sleep medicine textbook. European Sleep Research Society
Chung F, Abdullah HR, Liao P (2016) STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest 149(3):631–638. https://doi.org/10.1378/chest.15-0903
Pecotic R, Dodig IP, Valic M, Ivkovic N, Dogas Z (2012) The evaluation of the Croatian version of the Epworth sleepiness scale and STOP questionnaire as screening tools for obstructive sleep apnea syndrome. Sleep Breath 16(3):793–802
Fischer J, Dogas Z, Bassetti CL, Berg S, Grote L, Jennum P, Levy P, Mihaicuta S, Nobili L, Riemann D, Puertas Cuesta FJ, Raschke F, Skene DJ, Stanley N, Pevernagie D (2012) Standard procedures for adults in accredited sleep medicine centres in Europe. J Sleep Res 21(4):357–368. https://doi.org/10.1111/j.1365-2869.2011.00987.x
Epstein L, Kristo D, Strollo P Jr, Friedman N, Malhotra A, Patil S, Ramar K, Rogers R, Schwab R, Weaver E (2009) Adult obstructive sleep apnea task force of the American Academy of sleep medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5(3):263–276
Narkiewicz K, Somers VK (2003) Sympathetic nerve activity in obstructive sleep apnoea. Acta Physiol Scand 177(3):385–390. https://doi.org/10.1046/j.1365-201X.2003.01091.x
Mahata SK, Kiranmayi M, Mahapatra NR (2018) Catestatin: a master regulator of cardiovascular functions. Curr Med Chem 25(11):1352–1374. https://doi.org/10.2174/0929867324666170425100416
Meng L, Ye XJ, Ding WH, Yang Y, Di BB, Liu L, Huo Y (2011) Plasma catecholamine release-inhibitory peptide catestatin in patients with essential hypertension. J Cardiovasc Med (Hagerstown) 12(9):643–647. https://doi.org/10.2459/JCM.0b013e328346c142
Schillaci G, De Vuono S, Pucci G (2011) An endogenous brake on the sympathetic nervous system: the emerging role of catestatin in hypertension. J Cardiovasc Med (Hagerstown) 12(9):609–612. https://doi.org/10.2459/JCM.0b013e328348d925
Liu L, Ding W, Li R, Ye X, Zhao J, Jiang J, Meng L, Wang J, Chu S, Han X, Peng F (2013) Plasma levels and diagnostic value of catestatin in patients with heart failure. Peptides 46:20–25. https://doi.org/10.1016/j.peptides.2013.05.003
Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK (2010) Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 137(3):711–719. https://doi.org/10.1378/chest.09-0360
Ernst G, Bosio M, Salvado A, Dibur E, Nigro C, Borsini E (2016) Difference between apnea-hypopnea index (AHI) and oxygen desaturation index (ODI): proportional increase associated with degree of obesity. Sleep Breath 20(4):1175–1183. https://doi.org/10.1007/s11325-016-1330-3
Bandyopadhyay GK, Vu CU, Gentile S, Lee H, Biswas N, Chi NW, O'Connor DT, Mahata SK (2012) Catestatin (chromogranin A(352-372)) and novel effects on mobilization of fat from adipose tissue through regulation of adrenergic and leptin signaling. J Biol Chem 287(27):23141–23151. https://doi.org/10.1074/jbc.M111.335877
Gaede AH, Pilowsky PM (2012) Catestatin, a chromogranin A-derived peptide, is sympathoinhibitory and attenuates sympathetic barosensitivity and the chemoreflex in rat CVLM. Am J Physiol Regul Integr Comp Physiol 302(3):R365–R372. https://doi.org/10.1152/ajpregu.00409.2011
Smith JC, Ellenberger HH, Ballanyi K, Richter DW, Feldman JL (1991) Pre-Botzinger complex: a brainstem region that may generate respiratory rhythm in mammals. Science 254(5032):726–729
Gaede AH, Pilowsky PM (2010) Catestatin in rat RVLM is sympathoexcitatory, increases barosensitivity, and attenuates chemosensitivity and the somatosympathetic reflex. Am J Physiol Regul Integr Comp Physiol 299(6):R1538–R1545. https://doi.org/10.1152/ajpregu.00335.2010
Tan KC, Chow WS, Lam JC, Lam B, Wong WK, Tam S, Ip MS (2006) HDL dysfunction in obstructive sleep apnea. Atherosclerosis 184(2):377–382. https://doi.org/10.1016/j.atherosclerosis.2005.04.024
Kawano Y, Tamura A, Kadota J (2012) Association between the severity of obstructive sleep apnea and the ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol. Metabolism 61(2):186–192. https://doi.org/10.1016/j.metabol.2011.06.004
Verghese PB, Arrese EL, Soulages JL (2007) Stimulation of lipolysis enhances the rate of cholesterol efflux to HDL in adipocytes. Mol Cell Biochem 302(1–2):241–248. https://doi.org/10.1007/s11010-007-9447-0
Acknowledgements
We would like to thank Natalija Ivkovic, M.Sc. (Sleep Medicine Center), for her important contribution in conducting sleep assessment studies.
Funding
The Croatian Science Foundation provided financial support in the form of grant to principal investigator Prof. Zoran Dogas (Project no. 5935). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Borovac, J.A., Dogas, Z., Supe-Domic, D. et al. Catestatin serum levels are increased in male patients with obstructive sleep apnea. Sleep Breath 23, 473–481 (2019). https://doi.org/10.1007/s11325-018-1703-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1703-x