Abstract
Purpose
Although bilevel positive airway pressure (Bilevel PAP) therapy is usually used for overlap syndrome (OS), there is still a portion of OS patients in whom Bilevel PAP therapy could not simultaneously eliminate residual apnea events and hypercapnia. The current study was expected to explore whether auto-trilevel positive airway pressure (auto-trilevel PAP) therapy with auto-adjusting end expiratory positive airway pressure (EEPAP) can serve as a better alternative for these patients.
Methods
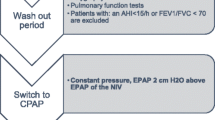
From January of 2014 to June of 2016, 32 hypercapnic OS patients with stable chronic obstructive pulmonary diseases (COPD) and moderate-to-severe obstructive sleep apnea syndrome (OSAS) were recruited. Three variable modes of positive airway pressure (PAP) from the ventilator (Prisma25ST, Weinmann Inc., Germany) were applicated for 8 h per night. We performed the design of each mode at each night with an interval of two nights with no PAP treatment as a washout period among different modes. In Bilevel-1 mode (Bilevel-1), the expiratory positive airway pressure (EPAP) delivered from Bilevel PAP was always set as the lowest PAP for abolishment of snoring. For each patient, the inspiratory positive airway pressure (IPAP) was constantly set the same as the minimal pressure for keeping end-tidal CO2 (ETCO2) ≤45 mmHg for all three modes. However, the EPAP issued by Bilevel PAP in Bilevel-2 mode (Bilevel-2) was kept 3 cmH2O higher than that in Bilevel-1. In auto-trilevel mode (auto-trilevel) with auto-trilevel PAP, the initial part of EPAP was fixed at the same PAP as that in Bilevel-1 while the EEPAP was automatically regulated to rise at a range of ≤4 cmH2O based on nasal airflow wave changes. Comparisons were made for parameters before and during or following treatment as well as among different PAP therapy modes. The following parameters were compared such as nocturnal apnea hypopnea index (AHI), minimal SpO2 (minSpO2), arousal index, sleep structure and efficiency, morning PaCO2, and daytime Epworth Sleepiness Scale (ESS).
Results
Compared with the parameters before PAP therapies, during each mode of PAP treatment, significant reduction was detected in nocturnal AHI, arousal index, morning PaCO2, and daytime ESS while significant elevation was revealed in nocturnal minSpO2 and sleep efficiency (all P < 0.01). Comparison among three PAP modes indicated that under the same IPAP, the auto-trilevel PAP mode could result in the lowest arousal index, daytime ESS, and the highest sleep efficiency. Compared with Bilevel-1, it was detected that (a) AHI was lower but minSpO2 was higher in both Bilevel-2 and auto-trilevel (all P < 0.05) and (b) morning PaCO2 showed no statistical difference from that in auto-trilevel but displayed higher in Bilevel-2 (P < 0.05). Compared with Bilevel-2, in auto-trilevel, both AHI and minSpO2 showed no obvious changes (all P > 0.05) except with a lower morning PaCO2 (P < 0.05).
Conclusion
Auto-trilevel PAP therapy was superior over conventional Bilevel PAP therapy for hypercapnic OS patients with their OSAS moderate to severe, since auto-trilevel PAP was more efficacious in synchronous elimination of residual obstructive apnea events and CO2 retention as well as in obtaining a better sleep quality and milder daytime drowsiness.




Similar content being viewed by others
References
Borukhov I, Rizzolo D (2016) Overlap syndrome: obstructive sleep apnea and chronic obstructive pulmonary disease. JAAPA 29:18–22
Tsai SC (2016) Chronic obstructive pulmonary disease and sleep related disorders. Curr Opin Pulm Med
McNicholas WT (2016) Chronic obstructive pulmonary disease and obstructive sleep apnoea-the overlap syndrome. J Thorac Dis 8:236–242
Lacedonia D, Carpagnano GE, Aliani M, Sabato R, Foschino Barbaro MP et al (2013) Daytime PaO2 in OSAS, COPD and the combination of the two (overlap syndrome). Respir Med 107:310–316
Shiina K, Tomiyama H, Takata Y, Yoshida M, Kato K, Nishihata Y et al (2012) Overlap syndrome: additive effects of COPD on the cardiovascular damages in patients with OSA. Respir Med 106:1335–1341
Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR (2010) Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med 182:325–331
Mansukhani MP, Kolla BP, Olson EJ, Ramar K, Morgenthaler TI (2014) Bilevel positive airway pressure for obstructive sleep apnea. Expert Rev Med Devices 11:283–294
Murphy PB, Arbane G, Ramsay M, Suh ES, Mandal S et al (2015) Safety and efficacy of auto-titrating noninvasive ventilation in COPD and obstructive sleep apnoea overlap syndrome. Eur Respir J 46:548–551
Zhang XW, Cai W, Jin F, Zhang YQ, Zhang XL (2011) Effect of bi-level positive airway pressure ventilator on the heart function and vascular endothelial function of patients with the overlap syndrome. Zhonghua Jie He He Hu Xi Za Zhi 34:17–20
Verbraecken J (2014) From CPAP to trilevel adaptive servo ventilation in chronic heart failure—have we got the magic bullet? Sleep Med 15:846–848
Oldenburg O, Bitter T, Wellmann B, Fischbach T, Efken C, Schmidt A et al (2012) Trilevel adaptive servoventilation for the treatment of central and mixed sleep apnea in chronic heart failure patients. Sleep Med 14:422–427
Heinzer R, White DP, Malhotra A, Lo YL, Dover L, Stevenson KE et al (2008) Effect of expiratory positive airway pressure on sleep disordered breathing. Sleep 31:429–432
Braga CW, Chen Q, Burschtin OE, Rapoport DM, Ayappa I (2011) Changes in lung volume and upper airway using MRI during application of nasal expiratory positive airway pressure in patients with sleep-disordered breathing. J Appl Physiol 111:1400–1409
Morrell MJ, Arabi Y, Zahn B, Badr MS (1998) Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 158:1974–1981
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Celli BR, MacNee W, ATS/ERS task force (2004) Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 23:932–946
Teschler H, Döhring J, Wang YM, Berthon-Jones M (2001) Adaptive pressure support servo-ventilation: a novel treatment for Cheyne-Stokes respiration in heart failure. Am J Respir Crit Care Med 164:614–619
Zhang XL, Yin KS, Li XL, Jia EZ, Su M (2006) Efficacy of adaptive servoventilation in patients with congestive heart failure and Cheyne-Stokes respiration. Chin Med J 119:622–627
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Sanders MH, Newman AB, Haggerty CL, Redline S, Lebowitz M, Samet J et al (2003) Sleep and sleep-disordered breathing in adults with predominantly mild obstructive airway disease. Am J Respir Crit Care Med 167:7–14
Murphy PB, Arbane G, Ramsay M, Suh ES, Mandal S, Jayaram D et al (2015) Safety and efficacy of auto-titrating noninvasive ventilation in COPD and obstructive sleep apnoea overlap syndrome. Eur Respir J 46:548–551
Kouns A, Phillips B (2011) New developments in the management of chronic obstructive pulmonary disease and the overlap syndrome. Curr Treat Options Neurol 13:488–495
De Backer L, Vos W, Dieriks B, Daems D, Verhulst S, Vinchurkar S et al (2011) The effects of long-term noninvasive ventilation in hypercapnic COPD patients: a randomized controlled pilot study. Int J Chron Obstruct Pulmon Dis 6:615–624
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study involving human participants were in accordance with the ethical standards of Patient Ethics and Research Committee of the First Affiliated Hospital of Nanjing Medical University and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The 333 high level personnel training program in Jiangsu Province (BRA-2014131) provided financial support in the form of ventilator application training, and the key research and development program of Huai’an (social development HAS201611) provided financial support in the form of necessary equipment for this study. The sponsors had no role in the design or conduct of this research.
Rights and permissions
About this article
Cite this article
Su, M., Huai, D., Cao, J. et al. Auto-trilevel versus bilevel positive airway pressure ventilation for hypercapnic overlap syndrome patients. Sleep Breath 22, 65–70 (2018). https://doi.org/10.1007/s11325-017-1529-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1529-y