Abstract
Dose adjustment of direct oral anticoagulants (DOACs) is not required in the setting of acute PE treatment according to the manufacturer’s labelling, beyond the contraindication in severe renal insufficiency. We designed a prospective, multicenter cohort study to investigate the impact of prescription of non-recommended DOAC doses on 6-month adverse events. The primary endpoint was a composite of all-cause death, recurrent VTE, major bleeding, and chronic thromboembolic pulmonary hypertension (CTEPH). In total, among 656 patients discharged with DOACs between 09/2012 and 10/2016, 28 (4.3%) were not treated with a recommended DOAC dose. All the non-recommended DOAC dose prescriptions were under-dosed according to the drug labelling. After multivariate adjustment, age > 70 years, a history of coronary artery disease, creatinine clearance < 50 mL/min and concomitant aspirin therapy were independently associated with non-recommended DOAC dose prescription (C-statistic: 0.82; Hosmer Lemeshow test: 0.50). The primary composite endpoint occurred in 7/28 patients (25.0%) in the non-recommended dose group and in 38/628 patients (6.1%) in the recommended dose group, yielding a relative risk of 3.19 in the non-recommended dose group (95% CI 1.16–8.70; p < 0.001). The higher primary endpoint rate observed in the non-recommended dose group was driven by a significantly higher rate of major bleeding (7.1 vs. 1.4%; p = 0.008), with a non-significant trend toward a higher rate of death (7.1 vs. 2.2%; p = 0.23), recurrent VTE (3.6 vs. 1.4%; p = 0.31), and CTEPH (7.1 vs. 1.6%; p = 0.32). In conclusion, empiric dose reduction of DOACs was associated with 6-month adverse events in our real-life registry.
Similar content being viewed by others
Highlights
-
Dose adjustment of direct oral anticoagulants (DOACs) is not required in the setting of acute pulmonary embolism (PE) treatment according to the manufacturer’s labelling
-
Very few data exist currently on the rate and clinical implications of non-recommended DOAC dose prescription in real-like practice
-
Among 656 patients discharge with DOACs, the rate of inappropriate DOAC dose prescription was 4.3% (n = 28) in our study
-
The rate of the primary endpoint of all-cause death, recurrent venous thromboembolism, major bleeding, and chronic venous thromboembolism was significantly higher in the non-recommended DOAC dose group (25% vs. 6.1%, respectively, p < 0.001), mainly driven by an excess of bleeding
-
Implementation of further strategies, such as correcting bleeding risk factors, or implanting an IVC filter in patients with a very high bleeding risk, might be safer than reducing the DOAC dose
Introduction
Pulmonary embolism (PE) is a relatively common disease, with an incidence ranging from 60 to 112 per 100,000 inhabitants of the United States [1], and is the third leading cardiovascular cause of death [2]. The mainstay treatment is anticoagulation, adapted to patient contraindications, to prevent early death and recurrent venous thromboembolism (VTE) [3]. For over 5 decades, PE antithrombotic treatment strategy included the use of a parenteral anticoagulant in combination with a vitamin K antagonist (VKA) until the target International Normalized Ratio of 2.0–3.0 was reached. The results of randomized trials using direct oral anticoagulants (DOACs) for the treatment of acute PE indicate that these agents are non-inferior in terms of efficacy at preventing recurrence of VTE and also safer, particularly in terms of major bleeding, than the conventional heparin/VKA regimen [4,5,6,7]. The 2016 ACCP guidelines recommend henceforth DOACs rather than VKA to treat acute VTE [3].
Contrary to stroke prevention in atrial fibrillation (AF) [8], dose adjustment is not required in the setting of acute PE treatment according to the manufacturer’s labelling, beyond the contraindication in patients with a creatinine clearance (CrCl) < 30 mL/min. In PE studies, the patients rate with criteria for reducing dosage according to AF treatment labelling range from 10 to 15% for patients aged > 75 years and was 7.9% for patients with renal function impairment (i.e., CrCl 30–45 mL/min) [4, 6]. The frequency of prescription of non-recommended DOAC doses, and its impact on outcomes, is poorly described in real-life practice [9,10,11,12].
Therefore, the present study aimed to investigate patterns of prescription of non-recommended DOAC doses for the treatment of acute PE, and the associated risk of 6-month adverse events.
Materials and methods
Study design
We designed a prospective, observational study, based on a multicenter registry including 11 departments in 5 centers, and covering 7 different clinical specialties [cardiology (n = 5 departments), vascular medicine (n = 1), internal medicine/geriatrics (n = 1), respiratory diseases (n = 1), oncology (n = 1), critical care (n = 1), and orthopedic surgery (n = 1)] in the region of Burgundy Franche Comte, France. For this study, only patients treated with DOACs were considered. The study period encompassed September 2012 through April 2017. We chose September 2012 as the starting point of this study, corresponding to the launch date of rivaroxaban, the first DOAC to be approved on the French market for the dedicated indication of acute PE treatment. Apixaban was authorized in this indication from April 2015 onwards.
Inclusion criteria were all patients aged 18 years or older with confirmed PE by computed tomography pulmonary angiography (CTPA), or ventilation–perfusion (V–Q) scan, discharge from hospital with a DOAC therapy. Patients were considered to receive the recommended therapy if DOACs were prescribed as follows: rivaroxaban 15 mg twice daily for 21 days (initial dosing) and then 20 mg once daily (long-term dosing); or apixaban 10 mg twice daily for 7 days and then 5 mg twice daily (rivaroxaban and apixaban were the only DOACs available on the French market in the indication of PE treatment at the time of this study).
Data collection
The study was conducted in accordance with the Declaration of Helsinki. Institutional Review Board approval was obtained. Informed consent was obtained from each study participant.
Patients were identified by requests to the hospital informatics database (Programme de Médicalisation des Systèmes d’Information, PMSI) using the International Classification of Disease (ICD-10) PE diagnosis codes (code I260 and I269) [13]. Research physicians performed a review of medical records at each site and abstracted data using a standard data collection form. Technicians entered data into a dedicated database for de-identification of personal information and for partial data validation. The research technicians were also asked to ensure that recruitment was consecutive.
Baseline characteristics including socio-demographic data, clinical data, imaging findings, and biological data were recorded prospectively. In-hospital adverse events including death, causes of death, recurrent VTE and bleeding were also recorded. Six months after the diagnosis of PE, patients returned to the hospital for a follow-up visit to record clinical status, anticoagulation treatments and outcomes (i.e., death, cause of death, recurrent VTE, and bleeding since hospital discharge). If the patient failed to attend the hospital visit, the following sequential procedure was followed: telephone interview with the patient or the patient’s family, consultation of the hospitalization records since discharge, telephone contact with the patient’s general practitioner or other treating physician, and finally, consultation of the national death registry. Six-month follow-up was 100% complete.
Clinical endpoint and definitions of outcomes
The primary endpoint was a composite of death from any cause, recurrent VTE, major bleeding, and chronic thromboembolic pulmonary hypertension (CTEPH). Prespecified secondary endpoints included each component of the primary end point (i.e., all-cause death, recurrent VTE, major bleeding, and CTEPH). All adverse events were adjudicated by an independent committee.
Recurrent VTE includes PE confirmed by visualization of new filling defects on V–Q scan or CTPA scan, or diagnosis of DVT on compression ultrasonography. Bleeding events were classified according to the International Society of Thrombosis and Haemostasis criteria for major bleeding [14]. CTEPH was defined according to the European Society of Cardiology (ESC) guidelines with a mean pulmonary artery pressure ≥ 25 mmHg with pulmonary arterial wedge pressure ≤ 15 mmHg on cardiac catheterization, and pulmonary artery obstruction seen by V–Q scan or CTPA [15].
Statistical analysis
Normally-distributed variables are expressed as mean ± SD and categorical variables as number and percentage (%). Unadjusted differences were compared using the Chi square test for categorical variables and Student’s t test for continuous variables. Predictors of non-recommended DOAC dose prescription were identified using multivariate logistic regression, including all baseline characteristics with a p value < 0.10 by univariate analysis. Results are reported as odds ratios (OR) with associated 95% confidence interval (CI) and p value. We compared follow-up outcomes between recommended and non-recommended DOAC dose groups by constructing a multivariate Cox models adjusted for any baseline characteristics and in-hospital course with a p value < 0.10 by univariate analysis. Results are reported as hazard ratios (HR) with associated 95% CI and p value. The Kaplan–Meier method was used to draw survival curves at 6 months. All multivariate models included site of care as a random effect to account for patient clustering within sites. Statistical tests were two-sided and considered significant if they yielded a p value < 0.05. Analyses were performed using SAS, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
In total, 1155 patients were admitted to the participating hospitals with an objectively confirmed diagnosis of acute PE between 09/2012 and 04/2017. Overall, 71 patients (6.1%) died during the hospital stay. Among the survivors, 656 patients (60.5%) were treated with DOACs [rivaroxaban: 614 patients (93.6%), apixaban 42 patients (6.4%)] and composed the study population.
The baseline characteristics of the study population are shown in Table 1. Mean age was 63.6 ± 17.9 years, 46.9% were males. Twenty patients (3.0%) had high-risk PE, 143 (21.8%) had intermediate-high-risk PE, 188 (28.6%) had intermediate-low-risk PE, and 305 (46.5%) had low-risk PE as defined by the ESC guidelines [16]. A total of 628 patients (95.7%) were treated with the recommended DOAC dose, and 28 patients (4.3%) had non-recommended DOAC dosing. Patients with and without the recommended DOAC dose differed significantly in terms of pre-existing medical conditions, and in relevant clinical, echographic and laboratory parameters (Table 1). Patients with non-recommended DOAC dose were significantly older, and more frequently presented coronary artery disease (CAD) and severe renal insufficiency as defined by a creatinine clearance below 30 mL/min. New York Heart Association functional status and arterial oxyhemoglobin saturation were also poorer in this group of patients. Creatinine clearance was lower and there was more frequent right ventricular dysfunction at admission in the non-recommended DOAC dose group. These findings resulted in a significantly higher sPESI score in the group of patients treated with non-recommended DOAC dose (Table 1). The rate of prior bleeding did not differ between both groups.
During the hospital course, reperfusion therapy including thrombolysis and surgical embolectomy, and extracorporeal membrane oxygenation and inferior vena cava filter implantation were not significantly different between recommended and non-recommended DOACs dose groups; in-hospital adverse events were also similar (Table 2).
At discharge, all the non-recommended DOAC dose prescriptions were under-dosed, as compared to the drug labelling. Five patients on rivaroxaban (0.8%) and seven patients on apixaban (16.6%) did not receive any recommended initial dose. Among the five patients who did not receive an initial dose of rivaroxaban, four were directly treated with the appropriate long-term dose (i.e., rivaroxaban 20 mg once daily) and one patient received a lower long-term dose (i.e., 15 mg once daily). Among the seven patients who did not received an initial dose of apixaban four patients received directly a non-recommended dose (i.e., 2.5 mg twice daily) and three patients received a recommended long-term dose (i.e., 5 mg twice daily). Regarding the long-term dose, 17 patients on rivaroxaban (2.7%) were prescribed 15 mg once daily, including one patient who did not receive an initial dose of rivaroxaban; 4 patients (9.5%) who initially did not receive an initial dose, were also treated with a non-recommended long-term dose of 2.5 mg twice daily. The rate of concomitant antiplatelet prescription was higher in the non-recommended DOAC dose group as compared to the recommended group (Table 2).
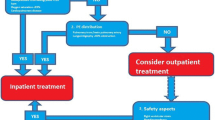
By multivariate analysis, age > 70 years (OR 2.9; 95% CI 1.2–7.4), a history of CAD (OR 2.7; 95% CI 1.05–6.7), creatinine clearance < 50 mL/min (OR 2.5; 95% CI 1.05–6.1), and concomitant aspirin therapy (OR 4.1; 95% CI 1.2–13.5) were independent factors associated with non-recommended DOAC prescription (C-statistic: 0.82; Hosmer Lemeshow test: 0.50) (Fig. 1).
Time from PE diagnosis to follow-up was 171 ± 11 days in the compliant group and 168 ± 9 days in the non-compliant group (p = 0.87). During the 6 months of follow up, 16 patients died: 1 disseminated cancer, 1 fatal PE, 1 major bleeding, 5 cardiovascular deaths and 8 from other causes. Ten patients presented recurrent VTE; 11 patients had one or more major bleeding events (4 intracranial, 3 gastrointestinal, 3 muscular, 2 pericardial and 1 urological); 12 patients presented CTEPH.
The primary composite endpoint occurred in 7 patients (25%) in the non-recommended dose group and in 38 patients (6.1%) in the recommended dose group (OR 3.19; 95% CI 1.16–8.70; p = 0.02) (Table 3). The corresponding Kaplan–Meier curves representing 6-month event free survival estimates are shown in Fig. 2. The higher primary endpoint rate observed in the non-recommended dose group was driven by a significantly higher rate of major bleeding (7.1 vs. 1.4%; p = 0.008), and a non-significant trend toward higher rate of death (7.1 vs. 2.2%, p = 0.23), recurrent VTE (3.6 vs. 1.4%, p = 0.31), and CTEPH (7.1 vs. 1.6%, p = 0.32) (Table 3).
Discussion
The present study, from a prospective multicenter multidisciplinary registry, indicates that 4.3% of patients treated with DOACs for the treatment of acute PE did not receive an appropriate dose at discharge. Older age, CAD on aspirin, and renal function impairment were factors associated with off-label DOAC dose prescription by providers. The rate of adverse events at 6 months after PE diagnosis was significantly higher in the group of patients inappropriately treated with DOACs as compared to those who received a DOAC dose in line with the manufacturer’s labeling. This higher rate of adverse events was driven by a significantly higher rate of major bleeding and by numerically albeit non-significantly higher rates of death, recurrent VTE, and CTEPH.
The rate of non-recommended DOAC dose prescription observed in our study was lower than previously reported, namely from 10 to 18% in other PE studies [9, 11, 12]. In the setting of AF, data from a large U.S. administrative database showed that 43% of patients with a renal indication for DOAC dose reduction were potentially overdosed and 13.3% of patients with no renal indication for DOAC dose reduction were potentially underdosed [17]. The inappropriate-low-dose rates ranged between 19.7 and 26.7% based on the CrCl, age, and weight criteria for dose adaptation in a registry including 1689 AF patients treated with DOACs [18].
Our results regarding outcomes in the non-recommended DOAC dose group are in line with those recently reported from the RIETE registry including 1511 patients, with an 18% prescription rate of off-label DOAC doses. In this registry, the authors showed a significantly increased rate of recurrent VTE (HR 10.5; 95% CI 1.28–85.9) associated with a numerically but non-significantly higher rate of bleeding and death in inappropriate DOAC dose patients [9]. Tran et al. reported likewise in 26 of 261 PE patients inappropriately treated with DOACs (10%), no death, 3 recurrent VTE (11.5%), 3 major bleeding (11.5%), and 3 clinically relevant non-major bleeding (11.5%) [11]. Regarding the relationship between non-recommended DOAC dose according to manufacturer’s labelling and outcomes in the setting of AF, Yao et al. observed an increased risk of bleeding in patients with renal impairment and no reduction of the DOAC dose (HR 2.19; 95% CI 1.07–4.46) and an increased risk of stroke in patients with normal renal function who received a reduced DOAC dose (HR 4.87; 95% CI 1.30–18.26) [17].
The factors we identified as related to prescription of off-label DOAC doses (old age, renal function impairment, concomitant antiplatelet therapy) are well known to increase the risk of bleeding. In the study that developed the HAS–BLED score, old age was significantly related to high bleeding risk (OR 2.66, 95% CI 1.33–5.32), as was renal function impairment (OR 2.86; 95% CI 1.33–6.18) [19]. Aspirin use was shown to be a risk factor for major bleeding in association with warfarin (HR 1.83; 95% CI 1.72–1.96) [20]. Our findings emphasize the provider’s concerns about DOAC prescription and bleeding risk, at least in some cases. However, we observed that attempts to limit the effect of DOAC by reducing the dose did not lead to a reduction in the adjusted risk of bleeding. Rather, treatable bleeding risk factors such as concomitant antiplatelet therapy should be identified and corrected, and as a last resort, refraining from prescribing anticoagulants and implanting an inferior vena cava (IVC) filter in very high bleeding risk patients could be alternative options [21]. The prescription of VKA rather than DOACs to reduce the risk of bleeding is likely an inappropriate strategy. In pivotal randomized trials of DOACs versus VKA for the treatment of acute PE, DOACs were associated with significantly less bleeding [4,5,6,7]. Moreover, DOACs were safer than VKA with respect to intracranial hemorrhage in patients receiving concomitant antiplatelet therapy in a recently published meta-analysis (HR 0.38; 95% CI 0.26–0.56) [22].
In total, our results underscore the difficulty of providing treatment in compliance with guidelines and manufacturer’s drug labeling,and present an important opportunity for multidisciplinary quality improvement to improve patient safety. The implementation of an on-site multidisciplinary pulmonary embolism response team, which engages multiple specialists to deliver evidence-based, organized, and efficient care to PE patients, could improve compliance with PE guidelines and patient safety [23].
Strength and limitations
This study was based on a large prospective multicenter registry. The outcomes were adjudicated, and follow-up was 100% complete. Moreover, we actively recruited patients through a range of possible ports of entry of such patients into the hospital, in a range of different medical specialties likely to encounter patients with PE.
However, our study has some limitations that deserve to be underlined. We do not have any individual data regarding the reasons motivating provider’s decisions to prescribe a treatment that was not in accordance with the drug labelling. The rate of inappropriate DOAC dose prescription was low and the event rates were low in our registry; therefore, the findings should be viewed as hypothesis-generating and need to be confirmed by future studies.
Conclusion
To conclude, the rate of empiric dose reduction of DOACs was low in our real-life registry but was associated with 6-month adverse events, especially in high-risk bleeding patients. Implementation of further strategies, such as correcting bleeding risk factors, or implanting an IVC filter in patients with a very high-risk of bleeding, could be safer than reduction of the DOAC dose. More robust data are warranted to confirm these results.
References
Wiener RS, Schwartz LM, Woloshin S (2011) Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med 171(9):831–837. https://doi.org/10.1001/archinternmed.2011.178
Goldhaber SZ, Bounameaux H (2012) Pulmonary embolism and deep vein thrombosis. Lancet 379(9828):1835–1846. https://doi.org/10.1016/S0140-6736(11)61904-1
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores L (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149(2):315–352. https://doi.org/10.1016/j.chest.2015.11.026
Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, Porcari A, Raskob GE, Weitz JI, Investigators A-E (2013) Apixaban for extended treatment of venous thromboembolism. N Engl J Med 368(8):699–708. https://doi.org/10.1056/NEJMoa1207541
Hokusai VTEI., Buller HR, Decousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH, Raskob GE, Schellong SM, Schwocho L, Segers A, Shi M, Verhamme P, Wells P (2013) Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 369(15):1406–1415. https://doi.org/10.1056/NEJMoa1306638
Investigators E-P, Buller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, Minar E, Chlumsky J, Verhamme P, Wells P, Agnelli G, Cohen A, Berkowitz SD, Bounameaux H, Davidson BL, Misselwitz F, Gallus AS, Raskob GE, Schellong S, Segers A (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366(14):1287–1297. https://doi.org/10.1056/NEJMoa1113572
Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ, Group R-CS (2009) Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 361(24):2342–2352. https://doi.org/10.1056/NEJMoa0906598
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383(9921):955–962. https://doi.org/10.1016/S0140-6736(13)62343-0
Trujillo-Santos J, Di Micco P, Dentali F, Douketis J, Diaz-Peromingo JA, Nunez MJ, Canas I, Mastroiacovo D, Saraiva de Sousa M, Monreal M, Investigators R (2017) Real-life treatment of venous thromboembolism with direct oral anticoagulants: the influence of recommended dosing and regimens. Thromb Haemost 117(2):382–389. https://doi.org/10.1160/TH16-07-0494
Barra ME, Fanikos J, Connors JM, Sylvester KW, Piazza G, Goldhaber SZ (2016) Evaluation of dose-reduced direct oral anticoagulant therapy. Am J Med 129(11):1198–1204. https://doi.org/10.1016/j.amjmed.2016.05.041
Tran E, Duckett A, Fisher S, Bohm N (2017) Appropriateness of direct oral anticoagulant dosing for venous thromboembolism treatment. J Thromb Thrombolysis 43(4):505–513. https://doi.org/10.1007/s11239-017-1487-z
Tellor KB, Patel S, Armbruster AL, Daly MW (2015) Evaluation of the appropriateness of dosing, indication and safety of rivaroxaban in a community hospital. J Clin Pharm Ther 40(4):447–451. https://doi.org/10.1111/jcpt.12288
Tuppin P, de Roquefeuil L, Weill A, Ricordeau P, Merliere Y (2010) French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique 58(4):286–290. https://doi.org/10.1016/j.respe.2010.04.005
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3 (4):692–694. https://doi.org/10.1111/j.1538-7836.2005.01204.x
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M, Aboyans V, Vaz Carneiro A, Achenbach S, Agewall S, Allanore Y, Asteggiano R, Paolo Badano L, Albert Barbera J, Bouvaist H, Bueno H, Byrne RA, Carerj S, Castro G, Erol C, Falk V, Funck-Brentano C, Gorenflo M, Granton J, Iung B, Kiely DG, Kirchhof P, Kjellstrom B, Landmesser U, Lekakis J, Lionis C, Lip GY, Orfanos SE, Park MH, Piepoli MF, Ponikowski P, Revel MP, Rigau D, Rosenkranz S, Voller H, Luis Zamorano J (2016) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37(1):67–119. https://doi.org/10.1093/eurheartj/ehv317
Konstantinides SV (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35(45):3145–3146. https://doi.org/10.1093/eurheartj/ehu393
Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA (2017) Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol 69(23):2779–2790. https://doi.org/10.1016/j.jacc.2017.03.600
Okumura Y, Yokoyama K, Matsumoto N, Tachibana E, Kuronuma K, Oiwa K, Matsumoto M, Kojima T, Hanada S, Nomoto K, Arima K, Takahashi F, Kotani T, Ikeya Y, Fukushima S, Itoh S, Kondo K, Chiku M, Ohno Y, Onikura M, Hirayama A, The SAKURA AF Registry Investigators (2017) Current use of direct oral anticoagulants for atrial fibrillation in Japan: findings from the SAKURA AF Registry. J Arrhythm 33(4):289–296. https://doi.org/10.1016/j.joa.2016.11.003
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138(5):1093–1100. https://doi.org/10.1378/chest.10-0134
Hansen ML, Sorensen R, Clausen MT, Fog-Petersen ML, Raunso J, Gadsboll N, Gislason GH, Folke F, Andersen SS, Schramm TK, Abildstrom SZ, Poulsen HE, Kober L, Torp-Pedersen C (2010) Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med 170(16):1433–1441. https://doi.org/10.1001/archinternmed.2010.271
Muriel A, Jimenez D, Aujesky D, Bertoletti L, Decousus H, Laporte S, Mismetti P, Munoz FJ, Yusen R, Monreal M, Investigators R (2014) Survival effects of inferior vena cava filter in patients with acute symptomatic venous thromboembolism and a significant bleeding risk. J Am Coll Cardiol 63(16):1675–1683. https://doi.org/10.1016/j.jacc.2014.01.058
Bennaghmouch N, de Veer A, Bode K, Mahmoodi BK, Dewilde WJM, Lip GYH, Brueckmann M, Kleine E, Ten Berg JM (2018) Efficacy and safety of the use of non-vitamin K antagonist oral anticoagulants in patients with non-valvular atrial fibrillation and concomitant aspirin therapy: a meta-analysis of randomized trials. Circulation 137(11):1117–1129. https://doi.org/10.1161/CIRCULATIONAHA.117.028513
Dudzinski DM, Piazza G (2016) Multidisciplinary pulmonary embolism response teams. Circulation 133(1):98–103. https://doi.org/10.1161/CIRCULATIONAHA.115.015086
Funding
This study was funded, in part, by a research grant from Bristol-Myers Squibb, Bayer, Boehringer-Ingelheim, and Daiichi Sankyo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Chopard has received research grant support from the French Federation of Cardiology, the Burgundy Franche-Comte region, and Edwards Lifesciences. Dr. Francois Schiele declares research grants from GlaxoSmithKline, St. Jude Medical, Sanofi-Aventis, Servier, Daiichi-Sankyo/Lilly. Dr. Nicolas Meneveau declares receipt of consultancy agreements Bayer Healthcare, BMS-Pfizer. Drs. Serzian, Humbert, Falvo, Morel-Aleton, Bonnet, Napporn, Kalbacher, Obert, Degano, Cappelier, Cottin have no relevant financial disclosures.
Ethical approval
The research involved human participants. The study was conducted in accordance with the Declaration of Helsinki. Institutional Review Board approval was obtained.
Informed consent
Informed consent was obtained from each study participant.
Rights and permissions
About this article
Cite this article
Chopard, R., Serzian, G., Humbert, S. et al. Non-recommended dosing of direct oral anticoagulants in the treatment of acute pulmonary embolism is related to an increased rate of adverse events. J Thromb Thrombolysis 46, 283–291 (2018). https://doi.org/10.1007/s11239-018-1690-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-018-1690-6