Abstract
Background
Obesity is associated with physical inactivity and impaired health-related quality of life (HRQoL). We aim to test the hypothesis that Roux-en-Y gastric bypass (RYGB) followed by supervised physical training improves physical activity (PA) levels and HRQoL.
Methods
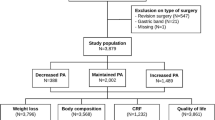
Sixty patients, qualified for RYGB, were at 6 months post-surgery randomized to 26 weeks of a supervised physical training intervention (INT) or to a control (CON) group. PA was assessed by accelerometry and using the questionnaire RPAQ. HRQoL was measured by the SF-36 questionnaire. All assessments were performed pre-surgery and 6, 12, and 24 months post-surgery.
Results
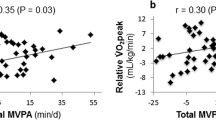
RYGB did not improve objectively or self-reported PA, but improved all domains of SF-36 (all p < 0.01). Objectively measured light PA, moderate to vigorous PA, and step counts tended to increase in INT compared to CON 12 months after RYGB (0.05 < p < 0.09), but the effects failed to persist. The SF-36 domain “general health” increased in INT compared to CON 24 months after RYGB (p = 0.041).
Conclusion
RYGB improves HRQoL, but does not increase PA. Supervised physical training intervention improves general health 24 months after RYGB and tends to improve certain domains of PA right after the intervention period, but fails to increase the patients’ overall PA level over time. Clinical Trial Registration Registered at ClinicalTrials.gov—no. NCT01690728.



Similar content being viewed by others
References
Pi-Sunyer, F. X. (1999). Comorbidities of overweight and obesity: Current evidence and research issues. Medicine & Science in Sports & Exercise, 31(11 Suppl), S602–S608.
Fontaine, K. R., & Barofsky, I. (2001). Obesity and health-related quality of life. Obesity Reviews, 2(3), 173–182.
Afshin, A., Forouzanfar, M. H., Reitsma, M. B., Sur, P., Estep, K., Lee, A., et al. (2017). Health effects of overweight and obesity in 195 countries over 25 years. The New England Journal of Medicine, 377(1), 13–27. https://doi.org/10.1056/NEJMoa1614362.
Sjöström, L., Narbro, K., Sjöström, C. D., Karason, K., Larsson, B., Wedel, H., et al. (2007). Effects of bariatric surgery on mortality in Swedish obese subjects. The New England Journal of Medicine, 357, 741–752. https://doi.org/10.1056/NEJMoa066254.
Sjöström, L. (2008). Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. International Journal of Obesity, 32(Suppl 7), S93–S97. https://doi.org/10.1038/ijo.2008.244.
Karlsson, J., Taft, C., Ryden, A., Sjostrom, L., & Sullivan, M. (2007). Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: The SOS intervention study. International Journal of Obesity (London), 31(8), 1248–1261. https://doi.org/10.1038/sj.ijo.0803573.
Hansen, B. H., Holme, I., Anderssen, S. A., & Kolle, E. (2013). Patterns of objectively measured physical activity in normal weight, overweight, and obese individuals (20–85 years): A cross-sectional study. PLoS ONE, 8(1), e53044. https://doi.org/10.1371/journal.pone.0053044.
Bond, D. S., Jakicic, J. M., Vithiananthan, S., Thomas, J. G., Leahey, T. M., Sax, H. C., et al. (2010). Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surgery for Obesity and Related Diseases, 6(1), 72–78. https://doi.org/10.1016/j.soard.2009.08.012.
Kesaniemi, Y. K., Danforth, E. Jr., Jensen, M. D., Kopelman, P. G., Lefebvre, P., & Reeder, B. A. (2001). Dose-response issues concerning physical activity and health: An evidence-based symposium. Medicine & Science in Sports & Exercise, 33(6 Suppl), S351–S358.
Haskell, W. L., Lee, I. M., Pate, R. R., Powell, K. E., Blair, S. N., Franklin, B. A., et al. (2007). Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation, 116(9), 1081–1093. https://doi.org/10.1161/CIRCULATIONAHA.107.185649.
Karmali, S., Brar, B., Shi, X., Sharma, A. M., de Gara, C., & Birch, D. W. (2013). Weight recidivism post-bariatric surgery: A systematic review. Obesity Surgery, 23(11), 1922–1933. https://doi.org/10.1007/s11695-013-1070-4.
Bond, D. S., Jakicic, J. M., Unick, J. L., Vithiananthan, S., Pohl, D., Roye, G. D., et al. (2010). Pre- to postoperative physical activity changes in bariatric surgery patients: Self report vs. objective measures. Obesity (Silver Spring), 18(12), 2395–2397. https://doi.org/10.1038/oby.2010.88.
Tully, M. A., Panter, J., & Ogilvie, D. (2014). Individual characteristics associated with mismatches between self-reported and accelerometer-measured physical activity. PLoS ONE, 9(6), e99636. https://doi.org/10.1371/journal.pone.0099636.
Bond, D. S., Phelan, S., Wolfe, L. G., Evans, R. K., Meador, J. G., Kellum, J. M., et al. (2009). Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring), 17(1), 78–83. https://doi.org/10.1038/oby.2008.501.
Colles, S. L., Dixon, J. B., & O’Brien, P. E. (2008). Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obesity Surgery, 18(7), 833–840. https://doi.org/10.1007/s11695-007-9409-3.
Sjöström, L., Lindroos, A.-K., Peltonen, M., Torgerson, J., Bouchard, C., Carlsson, B., et al. (2004). Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. The New England Journal of Medicine, 351, 2683–2693. https://doi.org/10.1056/NEJMoa035622.
Berglind, D., Willmer, M., Eriksson, U., Thorell, A., Sundbom, M., Udden, J., et al. (2015). Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obesity Surgery, 25(1), 119–125. https://doi.org/10.1007/s11695-014-1331-x.
King, W. C., Chen, J. Y., Bond, D. S., Belle, S. H., Courcoulas, A. P., Patterson, E. J., et al. (2015). Objective assessment of changes in physical activity and sedentary behavior: Pre- through 3 years post-bariatric surgery. Obesity (Silver Spring), 23(6), 1143–1150. https://doi.org/10.1002/oby.21106.
Herring, L. Y., Stevinson, C., Davies, M. J., Biddle, S. J., Sutton, C., Bowrey, D., et al. (2016). Changes in physical activity behaviour and physical function after bariatric surgery: A systematic review and meta-analysis. Obesity Reviews, 17(3), 250–261. https://doi.org/10.1111/obr.12361.
Shah, M., Snell, P. G., Rao, S., Adams-Huet, B., Quittner, C., Livingston, E. H., et al. (2011). High-volume exercise program in obese bariatric surgery patients: A randomized, controlled trial. Obesity (Silver Spring, Md.), 19, 1826–1834. https://doi.org/10.1038/oby.2011.172.
Coen, P. M., Tanner, C. J., Helbling, N. L., Dubis, G. S., Hames, K. C., Xie, H., et al. (2015). Clinical trial demonstrates exercise following bariatric surgery improves insulin sensitivity. The Journal of Clinical Investigation, 125(1), 248–257. https://doi.org/10.1172/JCI78016.
Herring, L. Y., Stevinson, C., Carter, P., Biddle, S. J., Bowrey, D., Sutton, C., et al. (2017). The effects of supervised exercise training 12–24 months after bariatric surgery on physical function and body composition: A randomised controlled trial. International Journal of Obesity (London). https://doi.org/10.1038/ijo.2017.60.
Coleman, K. J., Caparosa, S. L., Nichols, J. F., Fujioka, K., Koebnick, C., McCloskey, K. N., et al. (2017). Understanding the capacity for exercise in post-bariatric patients. Obesity Surgery, 27(1), 51–58. https://doi.org/10.1007/s11695-016-2240-y.
Hassannejad, A., Khalaj, A., Mansournia, M. A., Rajabian Tabesh, M., & Alizadeh, Z. (2017). The effect of aerobic or aerobic-strength exercise on body composition and functional capacity in patients with BMI ≥ 35 after Bariatric Surgery: A Randomized Control Trial. Obesity Surgery. https://doi.org/10.1007/s11695-017-2717-3.
Carnero, E. A., Dubis, G. S., Hames, K. C., Jakicic, J. M., Houmard, J. A., Coen, P. M., et al. (2017). Randomized trial reveals that physical activity and energy expenditure are associated with weight and body composition after RYGB. Obesity (Silver Spring), 25(7), 1206–1216. https://doi.org/10.1002/oby.21864.
Bize, R., Johnson, J. A., & Plotnikoff, R. C. (2007). Physical activity level and health-related quality of life in the general adult population: A systematic review. Preventive Medicine, 45(6), 401–415. https://doi.org/10.1016/j.ypmed.2007.07.017.
Brown, D. W., Balluz, L. S., Heath, G. W., Moriarty, D. G., Ford, E. S., Giles, W. H., et al. (2003). Associations between recommended levels of physical activity and health-related quality of life. Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey. Preventive Medicine, 37(5), 520–528.
Mundbjerg, L. H., Stolberg, C. R., Cecere, S., Bladbjerg, E. M., Funch-Jensen, P., Gram, B., et al. (2018). Supervised physical training improves weight loss after Roux-en-Y Gastric Bypass Surgery: A Randomized Controlled Trial. Obesity, 26(5), 828–837. https://doi.org/10.1002/oby.22143. doi.
Tudor-Locke, C., Brashear, M. M., Johnson, W. D., & Katzmarzyk, P. T. (2010). Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. International Journal of Behavioral Nutrition and Physical Activity, 7, 60. https://doi.org/10.1186/1479-5868-7-60.
Besson, H., Brage, S., Jakes, R. W., Ekelund, U., & Wareham, N. J. (2010). Estimating physical activity energy expenditure, sedentary time, and physical activity intensity by self-report in adults. American Journal of Clinical Nutrition, 91, 106–114. https://doi.org/10.3945/ajcn.2009.28432.
Ainsworth, B. E., Haskell, W. L., Leon, A. S., Jacobs, D. R. Jr., Montoye, H. J., Sallis, J. F., et al. (1993). Compendium of physical activities: Classification of energy costs of human physical activities. Medicine & Science in Sports & Exercise, 25(1), 71–80.
Bjorner, J. B., Thunedborg, K., Kristensen, T. S., Modvig, J., & Bech, P. (1998). The Danish SF-36 Health Survey: Translation and preliminary validity studies. Journal of Clinical Epidemiology, 51, 991–999.
Donnelly, J. E., Blair, S. N., Jakicic, J. M., Manore, M. M., Rankin, J. W., & Smith, B. K. (2009). American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise, 41(2), 459–471. https://doi.org/10.1249/MSS.0b013e3181949333.
Bond, D. S., Vithiananthan, S., Thomas, J. G., Trautvetter, J., Unick, J. L., Jakicic, J. M., et al. (2015). Bari-Active: A randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surgery for Obesity and Related Diseases, 11(1), 169–177. https://doi.org/10.1016/j.soard.2014.07.010.
Bond, D. S. (2017). Intervention-related increases in preoperative physical activity are maintained 6-months after Bariatric surgery: Results from the bari-active trial. International Journal of Obesity, 41(3), 467–470. https://doi.org/10.1038/ijo.2016.237.
van den Hoek, D. J., Miller, C. T., Fraser, S. F., Selig, S. E., & Dixon, J. B. (2017). Does exercise training augment improvements in quality of life induced by energy restriction for obese populations? A systematic review. Quality of Life Research. https://doi.org/10.1007/s11136-017-1602-9.
Bond, D. S., Thomas, J. G., King, W. C., Vithiananthan, S., Trautvetter, J., Unick, J. L., et al. (2015). Exercise improves quality of life in bariatric surgery candidates: results from the Bari-Active trial. Obesity (Silver Spring), 23(3), 536–542. https://doi.org/10.1002/oby.20988.
Kolotkin, R. L., Davidson, L. E., Crosby, R. D., Hunt, S. C., & Adams, T. D. (2012). Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surgery for Obesity and Related Diseases, 8(5), 625–633. https://doi.org/10.1016/j.soard.2012.01.011.
Acknowledgements
The authors would like to thank the study participants for their contribution to this study. We would also like to thank the physiotherapists involved in this study, for putting a large amount of effort into the supervised physical training intervention.
Funding
The research was supported by the Department of Regional Health Research, University of Southern Denmark and Hospital of Southwest Jutland, Denmark; the Department of Medicine/Endocrinology, Hospital of Southwest Jutland, Denmark; The Region of Southern Denmark; The Karola Jørgensen Research Foundation; The Edith and Vagn Hedegaard Jensens Foundation; and The Family Hede Nielsens Foundation.
Author information
Authors and Affiliations
Contributions
CRS, LHM, and BG carried out the experiments. CRS analyzed data. All authors were involved in writing the paper and final approval of the submitted and published versions.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was conducted according to the Helsinki Declaration, approved by the local ethics committee (Project-ID: S-20120112), and registered at ClinicalTrials.gov (No. NCT01690728).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Stolberg, C.R., Mundbjerg, L.H., Bladbjerg, EM. et al. Physical training following gastric bypass: effects on physical activity and quality of life—a randomized controlled trial. Qual Life Res 27, 3113–3122 (2018). https://doi.org/10.1007/s11136-018-1938-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1938-9