Abstract
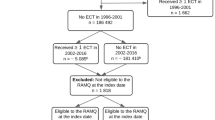
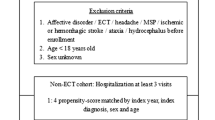
This study sought to examine the association between homelessness and receipt of electroconvulsive therapy (ECT) among older Medicare beneficiaries with homelessness. Among individuals with major depressive disorder who were older (age 65+) Medicare beneficiaries (2014–2015 data), we compared clinical and sociodemographic characteristics among those who were homeless and received ECT, those who were not homeless and received ECT, those who were homeless and did not receive ECT, and those who were domiciled and did not receive ECT. The unadjusted rate of ECT use among older homeless individuals with depression (1.46%) was higher than the rate of ECT use among older non-homeless individuals with depression (0.41%). Among all individuals receiving ECT, homeless individuals started as inpatients at a greater rate (94.0% v. 72.6%) and transitioned to outpatient ECT at a lower rate (23.8% v. 44.5%) compared to their domiciled counterparts. The individuals in the ECT/homeless group had more psychiatric comorbidities compared to all other groups. After adjusting for significant covariates, homelessness was associated with a lower odds ratio (0.74, 95% CI 0.55–0.99) of receiving ECT. Our data suggest that ECT can be provided to homeless individuals at rates comparable to domiciled individuals. The psychosocial support typically required for an ECT course may prove difficult for homeless patients in the outpatient setting, which may be an area for further development.
Similar content being viewed by others
References
Tsai J. Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health (Oxf). 2018;40(1):65–74. https://doi.org/10.1093/pubmed/fdx034.
Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12): e225. https://doi.org/10.1371/journal.pmed.0050225.
Smartt C, Prince M, Frissa S, Eaton J, Fekadu A, Hanlon C. Homelessness and severe mental illness in low- and middle-income countries: scoping review. B J Psych Open. 2019;5(4): e57. https://doi.org/10.1192/bjo.2019.32.
Adams J, Rosenheck R, Gee L, Seibyl CL, Kushel M. Hospitalized younger: a comparison of a national sample of homeless and housed inpatient veterans. J Health Care Poor Underserved. 2007;18(1):173–84. https://doi.org/10.1353/hpu.2007.0000.
Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–84. https://doi.org/10.2105/ajph.92.5.778.
Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs Emergency Departments. Am J Public Health. 2013;103 Suppl 2(Suppl 2):S225–31. https://doi.org/10.2105/ajph.2013.301307.
Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481–98. https://doi.org/10.1111/sltb.12369.
Tsai J, Cao X. Association between suicide attempts and homelessness in a population-based sample of US veterans and non-veterans. J Epidemiol Community Health. 2019;73(4):346–52. https://doi.org/10.1136/jech-2018-211065.
Bommersbach TJ, Stefanovics EA, Rhee TG, Tsai J, Rosenheck RA. Suicide Attempts and Homelessness: Timing of Attempts Among Recently Homeless, Past Homeless, and Never Homeless Adults. Psychiatr Serv. 2020:appips 202000073.
Schoeyen HK, Kessler U, Andreassen OA, Auestad BH, Bergsholm P, Malt UF, et al. Treatment-resistant bipolar depression: a randomized controlled trial of electroconvulsive therapy versus algorithm-based pharmacological treatment. Am J Psychiatry. 2015;172(1):41–51. https://doi.org/10.1176/appi.ajp.2014.13111517.
Kellner CH, Husain MM, Knapp RG, McCall WV, Petrides G, Rudorfer MV, et al. Right Unilateral Ultrabrief Pulse ECT in Geriatric Depression: Phase 1 of the PRIDE Study. Am J Psychiatry. 2016;173(11):1101–9. https://doi.org/10.1176/appi.ajp.2016.15081101.
Petrides G, Malur C, Braga RJ, Bailine SH, Schooler NR, Malhotra AK, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am J Psychiatry. 2015;172(1):52–8. https://doi.org/10.1176/appi.ajp.2014.13060787.
Kellner CH, Fink M, Knapp R, Petrides G, Husain M, Rummans T, et al. Relief of expressed suicidal intent by ECT: a consortium for research in ECT study. Am J Psychiatry. 2005;162(5):977–82. https://doi.org/10.1176/appi.ajp.162.5.977.
Wilkinson ST, Kitay BM, Harper A, Rhee TG, Sint K, Ghosh A, et al. Examining barriers to the implementation of electroconvulsive therapy (ECT): results from a nation-wide survey of ECT practitioners Psychiatric services (Washington, D.C.). 2021;72(7):752-757.
Tsai J, Huang M, Rosenheck RA, Wilkinson S. A Randomized Controlled Trial of Video Psychoeducation for Electroconvulsive Therapy in the United States. Psychiatric services (Washington, D.C.). 2020:appips201900448. https://doi.org/10.1176/appi.ps.201900448.
Rhee TG, Olfson M, Sint K, Wilkinson ST. Characterization of the Quality of Electroconvulsive Therapy Among Older Medicare Beneficiaries. J clin psychiatry. 2020;81(4):19m13186.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33. https://doi.org/10.1097/MLR.0b013e31819432e5.
Wilkinson ST, Agbese E, Leslie DL, Rosenheck RA. Identifying Recipients of Electroconvulsive Therapy: Data From Privately Insured Americans. Psychiatric services (Washington, D.C.). 2018:appips201700364. https://doi.org/10.1176/appi.ps.201700364.
Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA. Use of ECT for the inpatient treatment of recurrent major depression. Am J Psychiatry. 1998;155(1):22–9. https://doi.org/10.1176/ajp.155.1.22.
Peterson R, Gundlapalli AV, Metraux S, Carter ME, Palmer M, Redd A, et al. Identifying Homelessness among Veterans Using VA Administrative Data: Opportunities to Expand Detection Criteria. PLoS One. 2015;10(7): e0132664. https://doi.org/10.1371/journal.pone.0132664.
Kuhn R, Culhane DP. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: Results from the analysis of administrative data. Am J Community Psychol. 1998;26(2):207–32.
Acknowledgements
This work was funded by the Veterans Health Administration National Center on Homelessness among Veterans. Dr. Wilkinson also acknowledges funding support from the Yale Department of Psychiatry. The funding agency had no role on this intellectual contribution from the study conception to journal publication. The views here belong to the authors alone and do not represent the views of any agency of the federal government.
Author information
Authors and Affiliations
Contributions
formulated research questions: all authors; design study: all authors; analyzing data: TGR; writing article: STW; revising article: all authors.
Corresponding author
Ethics declarations
Human Subjects Protection and Informed Consent
The study procedures for this secondary analysis of restricted data were approved by the Institutional Review Board (HIC #2000022916) at Yale School of Medicine. Informed consent was not deemed necessary by the IRB.
Conflicts of Interest
Dr. Wilkinson has received contract funding from Janssen, Sage Therapeutics, and Oui Therapeutics for the conduct of clinical trials administered through Yale University. He has received consulting fees from Janssen, Oui Therapeutics, Sage Therapeutics, and Biohaven Pharmaceuticals. The other authors have no conflicts to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilkinson, S.T., Rhee, T.G. & Tsai, J. Utilization of Electroconvulsive Therapy for Older Homeless Adults Covered by Medicare. Psychiatr Q 92, 1825–1837 (2021). https://doi.org/10.1007/s11126-021-09946-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-021-09946-3