Abstract
Objective
To assess the effects of pharmacists giving advice to meet patients’ needs after starting a new medicine for a chronic condition.
Method
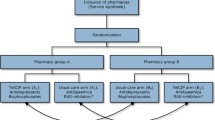
A prospective health technology assessment including a randomised controlled trial of a pharmacist-delivered intervention to improve adherence using a centralised telephone service to patients at home in England. Patients were eligible for recruitment if they were receiving the first prescription for a newly prescribed medication for a chronic condition and were 75 or older or suffering from stroke, cardiovascular disease, asthma, diabetes or rheumatoid arthritis.
Main outcome measures
Incidence of non-adherence, problems with the new medicine, beliefs about the new medicine, safety and usefulness of the interventions.
Results
Five hundred patients consented and were randomised. At 4-week follow-up, non-adherence was significantly lower in the intervention group compared to control (9% vs. 16%, P = 0.032). The number of patients reporting medicine-related problems was significantly lower in the intervention group compared to the control (23% vs. 34%, P = 0.021). Intervention group patients also had more positive beliefs about their new medicine, as shown by their higher score on the “necessity-concerns differential” (5.0 vs. 3.5, P = 0.007). The phone calls took a median of 12 min each. Most advice was judged by experts to be safe and helpful, and patients found it useful.
Conclusion
Overall, these findings show benefits from pharmacists meeting patients’ needs for information and advice on medicines, soon after starting treatment. While a substantially larger trial would be needed to confirm that the effect is real and sustained, these initial findings suggest the service may be safe and useful to patients.
Similar content being viewed by others
References
Smith M. The cost of non-compliance and the capacity of improved compliance to reduce health care expenditures. In: Improving medication compliance. Proceedings of a Symposium held in Washington DC, November 1984. Reston, Virginia: National Pharmaceutical Council, 1985;35-4.
Horne R. Adherence to medication: a review of the existing literature. In: Myers L, Midence K, editors. Adherence to treatment in medical conditions. Amsterdam: Harwood Academic Press; 1998. p 285–310. ISBN: 9057022656.
Lewis A. Noncompliance: A $100 billion problem. Remington Report. 1997;5(4):14-.
McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA 2002;288:2868-9.
Leventhal H, Cameron LD. Behavioral theories and the problem of compliance. Patient Educ Couns 1987;10:117-8.
Horne R, Weinman J. Patients’ beliefs about medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999;47(6):555-7.
Horne R. Treatment perceptions and self-regulation. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. London: Routledge Taylor & Francis Group, 2003. p 138–53. ISBN: 0415297001.
Barber N, Parsons J, Clifford S, Darracott R, Horne R. Patients’ problems with new medication for chronic conditions. Qual Saf Health Care 2004;13(3):172–5.
Ware JE, Sherbourne CD. The MOS 36 item short form health survey (SF-36): Conceptual framework and item selection. Med Care 1992;30:473.
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development of a new method for assessing the cognitive representation of medication. Psychol Health 1999;14:1–24.
Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA 2002;288:2880-.
Haynes RB, Taylor DW, Sackett DL, Gibson ES, Bernholtz CD, Mukherjee J. Can simple clinical measures detect patient non-compliance? Hypertension 1980;2:757-4.
Barber N. Should we consider non-compliance a medical error? Qual Saf Health Care 2002;11:81-.
Dean B, Barber N. Validity and reliability of observational methods for studying medication administration errors. Am J Health-Syst Pharm 2001;58:54-.
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999;47:555-7.
Department of Health. Pharmacy in the future. 2000. Available at: http://www.dh.gov.uk/assetRoot/04/06/82/04/04068204.pdf. (Accessed March 13th 2005).
Department of Health. A Vision for Pharmacy in the New NHS. 2003. [26 pages]. Available at: http://www.dh.gov.uk/assetRoot/04/06/83/56/04068356.pdf. (Accessed March 13th 2005).
Blenkinsopp A, Phelan M, Bourne J, Dakhil N. Extended adherence support by community pharmacists for patients with hypertension: a randomised controlled trial. Int J Pharm Pract 2000;8:165-5.
Goodyer LI, Miskelly F, Milligan P. Does encouraging good compliance improve patients’ clinical condition in heart failure? Br J Clin Pharmacol 1995;49(4):173–6.
Kaplan RM, Simon HJ. Compliance in medical care: reconsideration of self-predictions. Ann Behav Med 1990;12:66–71.
Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA 1992;267:2221-6.
Acknowledgements
We would like to thank the many who helped us: Intervention pharmacists: Helen Smurthwaite, Glen Savage. Expert panel: Imogen Savage, Mike Schachter, Colin Bradley, John Benson, Marie Miller. Statistical advice: Colin Chalmers. This work was undertaken by Professor N Barber and colleagues who received funding from the DHSC London, Research & Development, Responsive Funding Programme. The views expressed in the publication are those of the authors and not necessarily those of the National Health Service or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clifford, S., Barber, N., Elliott, R. et al. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci 28, 165–170 (2006). https://doi.org/10.1007/s11096-006-9026-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-006-9026-6