ABSTRACT
Purpose
To develop a computational model for optimisation of low corneal permeability, which is a key feature in ocular drug development.
Methods
We have used multivariate analysis to build corneal permeability models based on a structurally diverse set of 58 drug-like compounds.
Results
According to the models, the most important parameters for permeability are logD at physiologically relevant pH and the number of hydrogen bonds that can be formed. Combining these descriptors resulted in models with Q 2 and R 2 values ranging from 0.77 to 0.79. The predictive capability of the models was verified by estimating the corneal permeability of an external data set of 11 compounds and by using predicted permeability values to calculate the aqueous humour concentrations in the steady-state of seven compounds. The predicted values correlated well with experimental values.
Conclusion
The developed models are useful in early drug development to predict the corneal permeability and steady-state drug concentration in aqueous humor without experimental data.



Similar content being viewed by others
Abbreviations
- Css :
-
steady-state concentration
- HBA:
-
number of hydrogen bond acceptors
- HBD:
-
number of hydrogen bond donors
- HBtot :
-
total number of putative hydrogen bonds, i.e. HBD + HBA
- logP:
-
the logarithm of the octanol-water partition coefficient of the neutral form
- logperm :
-
the logarithm of the corneal permeability
- logD7.0, logD7.4 and logD8.0 :
-
the logarithm of the octanol-water partition coefficient at pH 7.0, 7.4 and 8.0, respectively
- MV:
-
molecular volume
- MW:
-
molecular weight
- PCA:
-
principal component analysis
- PLS:
-
partial least squares
- PSA:
-
polar surface area
- QSPR:
-
quantitative structure-property relationship
- RMSE:
-
root mean squared error
- RMSEP:
-
root mean squared error of prediction
- VIP:
-
variable importance in the projection
REFERENCES
Maurice DM, Mishima S. In: Sears ML, editor. Ocular pharmacokinetics. Berlin-Heidelberg: Springer Verlag; 1984. p. 16–119.
Schoenwald RD, Ward RL. Relationship between steroid permeability across excised rabbit cornea and octanol-water partition coefficients. J Pharm Sci. 1978;67:786–8.
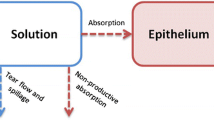
Urtti A, Salminen L. Minimizing systemic absorption of topically administered ophthalmic drugs. Surv Ophthalmol. 1993;37:435–56.
Huang HS, Schoenwald RD, Lach JL. Corneal penetration behavior of beta-blocking agents II: assessment of barrier contributions. J Pharm Sci. 1983;72:1272–9.
Toropainen E, Ranta VP, Talvitie A, Suhonen P, Urtti A. Culture model of human corneal epithelium for prediction of ocular drug absorption. Invest Ophthalmol Vis Sci. 2001;42:2942–8.
Toropainen E, Ranta VP, Vellonen KS, Palmgren J, Talvitie A, Laavola M et al. Paracellular and passive transcellular permeability in immortalized human corneal epithelial cell culture model. Eur J Pharm Sci. 2003;20:99–106.
Linnankoski J, Ranta VP, Yliperttula M, Urtti A. Passive oral drug absorption can be predicted more reliably by experimental than computational models—fact or myth. Eur J Pharm Sci. 2008;34:129–39.
Linnankoski J, Makela JM, Ranta VP, Urtti A, Yliperttula M. Computational prediction of oral drug absorption based on absorption rate constants in humans. J Med Chem. 2006;49:3674–81.
Winiwarter S, Bonham NM, Ax F, Hallberg A, Lennernas H, Karlen A. Correlation of human jejunal permeability (in vivo) of drugs with experimentally and theoretically derived parameters. A multivariate data analysis approach. J Med Chem. 1998;41:4939–49.
Moss GP, Dearden JC, Patel H, Cronin MT. Quantitative structure-permeability relationships (QSPRs) for percutaneous absorption. Toxicol In Vitro. 2002;16:299–317.
Yoshida F, Topliss JG. Unified model for the corneal permeability of related and diverse compounds with respect to their physicochemical properties. J Pharm Sci. 1996;85:819–23.
Fu XC, Liang WQ. A simple model for the prediction of corneal permeability. Int J Pharm. 2002;232:193–7.
Schoenwald RD, Huang HS. Corneal penetration behavior of beta-blocking agents I: physiochemical factors. J Pharm Sci. 1983;72:1266–72.
Li Y, Liu J, Pan D, Hopfinger AJ. A study of the relationship between cornea permeability and eye irritation using membrane-interaction QSAR analysis. Toxicol Sci. 2005;88:434–46.
Edwards A, Prausnitz MR. Predicted permeability of the cornea to topical drugs. Pharm Res. 2001;18:1497–508.
Duffel MW, Ing IS, Segarra TM, Dixson JA, Barfknecht CF, Schoenwald RD. N-Substituted sulfonamide carbonic anhydrase inhibitors with topical effects on intraocular pressure. J Med Chem. 1986;29:1488–94.
Maren TH, Jankowska L, Sanyal G, Edelhauser HF. The transcorneal permeability of sulfonamide carbonic anhydrase inhibitors and their effect on aqueous humor secretion. Exp Eye Res. 1983;36:457–79.
Wang W, Sasaki H, Chien DS, Lee VH. Lipophilicity influence on conjunctival drug penetration in the pigmented rabbit: a comparison with corneal penetration. Curr Eye Res. 1991;10:571–9.
Chiang CH, Schoenwald RD. Ocular pharmacokinetic models of clonidine-3H hydrochloride. J Pharmacokin Biopharm. 1986;14:175–211.
Chiang CH, Schoenwald RD, Huang HS. Corneal permeability of adrenergic agents potentially useful in glaucoma. J Taiwan Pharmaceut Assoc. 1986;38:67–84.
Schoenwald RD, Houseman JA. Disposition of cyclo-phosphamide in the rabbit and human cornea. Biopharm Drug Dispos. 1982;3:231–41.
Eller MG, Schoenwald RD, Dixson JA, Segarra T, Barfknecht CF. Topical carbonic anhydrase inhibitors. III: optimization model for corneal penetration of ethoxzolamide analogues. J Pharm Sci. 1985;74:155–60.
Wu NC, Chiang CH, Lee AR. Studies of carbonic anhydrase inhibitors: physicochemical properties and bioactivities of new thiadiazole derivatives. J Ocul Pharmacol. 1993;9:97–108.
Jankowska L, Bar-Ilan A, Maren TH. The relations between ionic and nonionic diffusion of sulfonamides across the rabbit cornea. Invest Ophthal Vis Sci. 1986;27:29–37.
Advanced Chemistry Developement, Toronto, Canada.
Bolton EE, Wang Y, Thiessen PA, Bryant SH. PubChem: integrated platform of small molecules and biological activities. Annu Rep Comput Chem. 2008;4:217–41.
Umetrics AB, Box 7960, SE-90719 Umeå, Sweden. Simca-P. 10.5.
Wold S. In: van de Waterbeemd H, editor. PLS for multivariate linear modeling. Weinheim: VCH; 1995. p. 195–218.
Rao CS, Schoenwald RD, Barfknecht CF, Laban SL. Biopharmaceutical evaluation of ibufenac, ibuprofen, and their hydroxyethoxy analogs in the rabbit eye. J Pharmacokinet Biopharm. 1992;20:357–88.
Schoenwald RD, Chien DS. Ocular absorption and disposition of phenylephrine and phenylephrine oxazolidine. Biopharm Drug Dispos. 1988;9:527–38.
Rusinko A, Hellberg MR, May JA, Owen GR. Use of MDCK cell line to predict corneal penetration of drugs. 2007;11114649.
Worth AP, Cronin MTD. Structure-permeability relationship for transcorneal penetration. ATLA. 2000;28:403–13.
Norinder U, Sjoberg P, Osterberg T. Theoretical calculation and prediction of brain-blood partitioning of organic solutes using MolSurf parametrization and PLS statistics. J Pharm Sci. 1998;87:952–9.
Malkia A, Murtomaki L, Urtti A, Kontturi K. Drug permeation in biomembranes: in vitro and in silico prediction and influence of physicochemical properties. Eur J Pharm Sci. 2004;23:13–47.
Tonjum AM. Movement of horseradish peroxidase in the cornea, sclera and the anterior uvea. Acta Ophthalmol (Copenh). 1977;55:771–80.
Urtti A. Challenges and obstacles of ocular pharmacokinetics and drug delivery. Adv Drug Deliv Rev. 2006;58:1131–5.
Ahmed I, Patton TF. Importance of the noncorneal absorption route in topical ophthalmic drug delivery. Invest Ophthalmol Vis Sci. 1985;26:584–7.
Kawazu K, Oshita A, Nakamura T, Nakashima M, Ichikawa N, Sasaki H. Transport of acebutolol through rabbit corneal epithelium. 2006;29:846–9.
ACKNOWLEDGEMENTS
This work was supported by the Academy of Finland. Heikki Käsnänen is thanked for valuable comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kidron, H., Vellonen, KS., del Amo, E.M. et al. Prediction of the Corneal Permeability of Drug-Like Compounds. Pharm Res 27, 1398–1407 (2010). https://doi.org/10.1007/s11095-010-0132-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-010-0132-8