Abstract
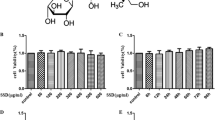
Maresin 1 is a novel pro-resolving mediator derived from docosahexaenoic acid (DHA), with potent anti-inflammation effects against several animal models, including brain ischemia, sepsis, and lung fibrosis. However, its effect against motor neuron cell death is still not investigated. Therefore, we investigated the effects of maresin 1 on several stress-induced motor neuron cell death. Maresin 1 suppressed combinatorial stress which was evoked by superoxide dismutase 1 (SOD1)G93A and serum-free, -induced motor neuron cells death in a concentration-dependent manner, and had a stronger neuroprotective effective than DHA. Maresin 1 also had neuroprotective effects against transactivation response DNA-binding protein (TDP)-43A315T and serum-free stress, H2O2, and tunicamycin-induced cell death. Maresin 1 reduced the reactive oxygen species (ROS) production caused by SOD1G93A or TDP-43A315T. Moreover, maresin 1 suppressed the NF-κB activation induced by SOD1G93A and serum-free stress. These data indicate that maresin 1 has motor neuron protective effects against several stresses by reduction of ROS production or attenuation of the NF-κB activation. Maresin 1 also had neuroprotective effects against H2O2, and tunicamycin-induced cell death in a concentration-dependent manner. Finally, maresin 1 ameliorated the motor function deficits of spinal muscular atrophy model in which endoplasmic reticulum stress was upregulated. Thus, maresin 1 may be beneficial to protect against motor neuron diseases.





Similar content being viewed by others
References
Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, Moussignac RL (2002) Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med 196:1025–1037
Bahety P, Tan YM, Hong Y, Zhang L, Chan EC, Ee PL (2014) Metabotyping of docosahexaenoic acid-treated Alzheimer’s disease cell model. PloS ONE 9:e90123
Hong SH, Khoutorova L, Bazan NG, Belayev L (2015) Docosahexaenoic acid improves behavior and attenuates blood-brain barrier injury induced by focal cerebral ischemia in rats. Exp Transl Stroke Med 7:3
Barrett EC, McBurney MI, Ciappio ED (2014) Omega-3 fatty acid supplementation as a potential therapeutic aid for the recovery from mild traumatic brain injury/concussion. Adv Nutr 5:268–277
Yip PK, Pizzasegola C, Gladman S, Biggio ML, Marino M, Jayasinghe M, Ullah F, Dyall SC, Malaspina A, Bendotti C, Michael-Titus A (2013) The omega-3 fatty acid eicosapentaenoic acid accelerates disease progression in a model of amyotrophic lateral sclerosis. PloS ONE 8:e61626
Fitzgerald KC, O’Reilly EJ, Falcone GJ, McCullough ML, Park Y, Kolonel LN, Ascherio A (2014) Dietary omega-3 polyunsaturated fatty acid intake and risk for amyotrophic lateral sclerosis. JAMA Neurol 71:1102–1110
Seki H, Tani Y, Arita M (2009) Omega-3 PUFA derived anti-inflammatory lipid mediator resolvin E1. Prostaglandins Other Lipid Mediat 89:126–130
Zhao Y, Calon F, Julien C, Winkler JW, Petasis NA, Lukiw WJ, Bazan NG (2011) Docosahexaenoic acid-derived neuroprotectin D1 induces neuronal survival via secretase- and PPARgamma-mediated mechanisms in Alzheimer’s disease models. PloS ONE 6:e15816
Nordgren TM, Bauer CD, Heires AJ, Poole JA, Wyatt TA, West WW, Romberger DJ (2015) Maresin-1 reduces airway inflammation associated with acute and repetitive exposures to organic dust. Transl Res 166:57–69
Gong J, Liu H, Wu J, Qi H, Wu ZY, Shu HQ, Li HB, Chen L, Wang YX, Li B, Tang M, Ji YD, Yuan SY, Yao SL, Shang Y (2015) Maresin 1 prevents lipopolysaccharide-induced neutrophil survival and accelerates resolution of acute lung injury. Shock 44:371–380
Xian W, Wu Y, Xiong W, Li L, Li T, Pan S, Song L, Hu L, Pei L, Yao S, Shang Y (2016) The pro-resolving lipid mediator Maresin 1 protects against cerebral ischemia/reperfusion injury by attenuating the pro-inflammatory response. Biochem Biophys Res Commun 472:175–181
Bunton-Stasyshyn RK, Saccon RA, Fratta P, Fisher EM (2015) SOD1 function and its implications for amyotrophic lateral sclerosis pathology: new and renascent themes. Neuroscientist 21:519–529
Rakhit R, Chakrabartty A (2006) Structure, folding, and misfolding of Cu, Zn superoxide dismutase in amyotrophic lateral sclerosis. Biochim Biophys Acta 1762:1025–1037
Ayala YM, Pantano S, D’Ambrogio A, Buratti E, Brindisi A, Marchetti C, Romano M, Baralle FE (2005) Human, Drosophila, and C. elegans TDP43: nucleic acid binding properties and splicing regulatory function. J Mol Biol 348:575–588
Guo W, Chen Y, Zhou X, Kar A, Ray P, Chen X, Rao EJ, Yang M, Ye H, Zhu L, Liu J, Xu M, Yang Y, Wang C, Zhang D, Bigio EH, Mesulam M, Shen Y, Xu Q, Fushimi K, Wu JY (2011) An ALS-associated mutation affecting TDP-43 enhances protein aggregation, fibril formation and neurotoxicity. Nat Struct Mol Biol 18:822–830
Alami NH, Smith RB, Carrasco MA, Williams LA, Winborn CS, Han SS, Kiskinis E, Winborn B, Freibaum BD, Kanagaraj A, Clare AJ, Badders NM, Bilican B, Chaum E, Chandran S, Shaw CE, Eggan KC, Maniatis T, Taylor JP (2014) Axonal transport of TDP-43 mRNA granules is impaired by ALS-causing mutations. Neuron 81:536–543
Estes PS, Boehringer A, Zwick R, Tang JE, Grigsby B, Zarnescu DC (2011) Wild-type and A315T mutant TDP-43 exert differential neurotoxicity in a Drosophila model of ALS. Hum Mol Genet 20:2308–2321
Correia AS, Patel P, Dutta K, Julien JP (2015) Inflammation induces TDP-43 mislocalization and aggregation. PloS ONE 10:e0140248
Liu Y, Hao W, Dawson A, Liu S, Fassbender K (2009) Expression of amyotrophic lateral sclerosis-linked SOD1 mutant increases the neurotoxic potential of microglia via TLR2. J Biol Chem 284:3691–3699
Coovert DD, Le TT, McAndrew PE, Strasswimmer J, Crawford TO, Mendell JR, Coulson SE, Androphy EJ, Prior TW, Burghes AH (1997) The survival motor neuron protein in spinal muscular atrophy. Hum Mol Genet 6:1205–1214
Ono Y, Tanaka H, Takata M, Nagahara Y, Noda Y, Tsuruma K, Shimazawa M, Hozumi I, Hara H (2014) SA4503, a sigma-1 receptor agonist, suppresses motor neuron damage in in vitro and in vivo amyotrophic lateral sclerosis models. Neurosci Lett 559:174–178
Zhang T, Baehr W, Fu Y (2012) Chemical chaperone TUDCA preserves cone photoreceptors in a mouse model of Leber congenital amaurosis. Investig Ophthalmol Vis Sci 53:3349–3356
Ando S, Funato M, Ohuchi K, Kameyama T, Inagaki S, Seki J, Kawase C, Tsuruma K, Shimazawa M, Kaneko H, Hara H (2017) Edaravone is a candidate agent for spinal muscular atrophy: in vitro analysis using a human induced pluripotent stem cells-derived disease model. Eur J Pharmacol 814:161–168
Rojas F, Cortes N, Abarzua S, Dyrda A, van Zundert B (2014) Astrocytes expressing mutant SOD1 and TDP43 trigger motoneuron death that is mediated via sodium channels and nitroxidative stress. Front Cell Neurosci 8:24
Li RC, Morris MW, Lee SK, Pouranfar F, Wang Y, Gozal D (2008) Neuroglobin protects PC12 cells against oxidative stress. Brain Res 1190:159–166
Ozgur R, Turkan I, Uzilday B, Sekmen AH (2014) Endoplasmic reticulum stress triggers ROS signalling, changes the redox state, and regulates the antioxidant defence of Arabidopsis thaliana. J Exp Bot 65:1377–1390
Kinsella S, Konig HG, Prehn JH (2016) Bid promotes K63-linked polyubiquitination of tumor necrosis factor receptor associated factor 6 (TRAF6) and sensitizes to mutant SOD1-induced proinflammatory signaling in microglia. eNeuro https://doi.org/10.1523/ENEURO.0099-15.2016
Lee M, Lee NY, Chung KS, Cheon SY, Lee KT, An HJ (2017) Roxatidine attenuates mast cell-mediated allergic inflammation via inhibition of NF-kappaB and p38 MAPK activation. Sci Rep 7:41721
Baichwal VR, Baeuerle PA (1997) Activate NF-kappa B or die? Curr Biol CB 7:R94-96
Ng SY, Soh BS, Rodriguez-Muela N, Hendrickson DG, Price F, Rinn JL, Rubin LL (2015) Genome-wide RNA-Seq of human motor neurons implicates selective ER stress activation in spinal muscular atrophy. Cell Stem Cell 17:569–584
Serhan CN, Yang R, Martinod K, Kasuga K, Pillai PS, Porter TF, Oh SF, Spite M (2009) Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J Exp Med 206:15–23
Chattopadhyay M, Valentine JS (2009) Aggregation of copper-zinc superoxide dismutase in familial and sporadic ALS. Antioxid redox Signal 11:1603–1614
Borchelt DR, Lee MK, Slunt HS, Guarnieri M, Xu ZS, Wong PC, Brown RH Jr, Price DL, Sisodia SS, Cleveland DW (1994) Superoxide dismutase 1 with mutations linked to familial amyotrophic lateral sclerosis possesses significant activity. Proc Natl Acad Sci USA 91:8292–8296
Yamagishi S, Koyama Y, Katayama T, Taniguchi M, Hitomi J, Kato M, Aoki M, Itoyama Y, Kato S, Tohyama M (2007) An in vitro model for Lewy body-like hyaline inclusion/astrocytic hyaline inclusion: induction by ER stress with an ALS-linked SOD1 mutation. PloS ONE 2:e1030
Hensley K, Mhatre M, Mou S, Pye QN, Stewart C, West M, Williamson KS (2006) On the relation of oxidative stress to neuroinflammation: lessons learned from the G93A-SOD1 mouse model of amyotrophic lateral sclerosis. Antioxid Redox Signal 8:2075–2087
Gitcho MA, Baloh RH, Chakraverty S, Mayo K, Norton JB, Levitch D, Hatanpaa KJ, White CL 3rd, Bigio EH, Caselli R, Baker M, Al-Lozi MT, Morris JC, Pestronk A, Rademakers R, Goate AM, Cairns NJ (2008) TDP-43 A315T mutation in familial motor neuron disease. Ann Neurol 63:535–538
Finelli MJ, Liu KX, Wu Y, Oliver PL, Davies KE (2015) Oxr1 improves pathogenic cellular features of ALS-associated FUS and TDP-43 mutations. Hum Mol Genet 24:3529–3544
Wang X, Zhou S, Ding X, Ma M, Zhang J, Zhou Y, Wu E, Teng J (2015) Activation of ER stress and autophagy induced by TDP-43 A315T as pathogenic mechanism and the corresponding histological changes in skin as potential biomarker for ALS with the mutation. Int J Biol Sci 11:1140–1149
Cleveland DW, Rothstein JD (2001) From Charcot to Lou Gehrig: deciphering selective motor neuron death in ALS. Nat Rev Neurosci 2:806–819
van Zundert B, Izaurieta P, Fritz E, Alvarez FJ (2012) Early pathogenesis in the adult-onset neurodegenerative disease amyotrophic lateral sclerosis. J Cell Biochem 113:3301–3312
Pasinelli P, Brown RH (2006) Molecular biology of amyotrophic lateral sclerosis: insights from genetics. Nat Rev Neurosci 7:710–723
Rindt H, Feng Z, Mazzasette C, Glascock JJ, Valdivia D, Pyles N, Crawford TO, Swoboda KJ, Patitucci TN, Ebert AD, Sumner CJ, Ko CP, Lorson CL (2015) Astrocytes influence the severity of spinal muscular atrophy. Hum Mol Genet 24:4094–4102
Hirayama O, Nakamura K, Hamada S, Kobayasi Y (1994) Singlet oxygen quenching ability of naturally occurring carotenoids. Lipids 29:149–150
Marcon R, Bento AF, Dutra RC, Bicca MA, Leite DF, Calixto JB (2013) Maresin 1, a proresolving lipid mediator derived from omega-3 polyunsaturated fatty acids, exerts protective actions in murine models of colitis. J Immunol 191:4288–4298
Li R, Wang Y, Zhao E, Wu K, Li W, Shi L, Wang D, Xie G, Yin Y, Deng M, Zhang P, Tao K (2016) Maresin 1, a proresolving lipid mediator, mitigates carbon tetrachloride-induced liver injury in mice. Oxid Med Cell Longev. https://doi.org/10.1155/2016/9203716
Ni A, Yang T, Mesnard-Hoaglin NA, Gutierrez R, Stubbs EB Jr, McGuire SO, Sanders VM, Jones KJ, Foecking EM, Xin J (2016) Th17 cell response in SOD1G93A mice following motor nerve injury. Mediat Inflamm. https://doi.org/10.1155/2016/6131234
Dang TN, Lim NK, Grubman A, Li QX, Volitakis I, White AR, Crouch PJ (2014) Increased metal content in the TDP-43(A315T) transgenic mouse model of frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Front Aging Neurosci 6:15
Campbell KJ, Rocha S, Perkins ND (2004) Active repression of antiapoptotic gene expression by RelA(p65) NF-kappa B. Mol Cell 13:853–865
Schreck R, Rieber P, Baeuerle PA (1991) Reactive oxygen intermediates as apparently widely used messengers in the activation of the NF-kappa B transcription factor and HIV-1. EMBO J 10:2247–2258
Tam AB, Mercado EL, Hoffmann A, Niwa M (2012) ER stress activates NF-kappaB by integrating functions of basal IKK activity, IRE1 and PERK. PloS ONE 7:e45078
Morgan MJ, Liu ZG (2011) Crosstalk of reactive oxygen species and NF-kappaB signaling. Cell Res 21:103–115
Dong J, Jimi E, Zeiss C, Hayden MS, Ghosh S (2010) Constitutively active NF-kappaB triggers systemic TNFalpha-dependent inflammation and localized TNFalpha-independent inflammatory disease. Genes Dev 24:1709–1717
Oshio T, Kawashima R, Kawamura YI, Hagiwara T, Mizutani N, Okada T, Otsubo T, Inagaki-Ohara K, Matsukawa A, Haga T, Kakuta S, Iwakura Y, Hosokawa S, Dohi T (2014) Chemokine receptor CCR8 is required for lipopolysaccharide-triggered cytokine production in mouse peritoneal macrophages. PloS ONE 9:e94445
Toth VE, Feher A, Nemeth J, Gyertyan I, Zadori ZS, Gyires K (2018) Modulation of central endocannabinoid system results in gastric mucosal protection in the rat. Brain Res Bull 139:224–234
Funding
This work was supported by Ono pharmaceutical Co., Ltd (Osaka, Japan) in this manuscript. This sponsor is involved in the study design and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
YO, MJ, KO: study design, the collection, analysis and interpretation of data, the writing of the report; KT: study design, the collection, analysis and interpretation of data; SO, SY: study design and the decision to submit the article for publication; HH, MS: study design, the collection, analysis and interpretation of data, the writing of the report and the decision to submit the article for publication.
Corresponding authors
Ethics declarations
Conflict of interest
Prof. Hideaki Hara has received a research grant from Ono pharmaceutical Co., Ltd. The other authors declare that have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ohuchi, K., Ono, Y., Joho, M. et al. A Docosahexaenoic Acid-Derived Pro-resolving Agent, Maresin 1, Protects Motor Neuron Cells Death. Neurochem Res 43, 1413–1423 (2018). https://doi.org/10.1007/s11064-018-2556-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-018-2556-1