Abstract
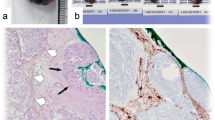
The purpose of this study was to evaluate spontaneous necrosis as a possible isolated factor for progression and recurrence in grade I meningiomas classified according to the current World Health Organization (WHO) classification. Meningiomas are the most frequently reported primary intracranial tumours, accounting for more than 35%. The 2016 WHO classification of central nervous system tumors stratifies meningiomas in grades I (benign), II (atypical), and III (malignant), according to histopathological aspects and the risk of progression or recurrence. Among 110 patients with intracranial meningiomas, 70 were WHO grade I meningiomas with no findings of atypia (G1WON), 15 were WHO grade I with necrosis (G1WN), 21 were WHO grade II (G2), and 4 were WHO grade III (G3). The mean follow-up was 5.9 ± 0.2 years. High performance scale (KPS ≥ 80) was different (p < 0.001) between WHO grade I meningiomas without (81.4%) and with (60%) necrosis. The 5-year mortality rate was 1.4, 6.7 and 5.9% for G1WON, G1WN and G2, respectively, with significant difference (p = 0.011) related to the presence of necrosis. The risk of recurrence was 3.7 times higher in G1WN than in G1WON (p = 0.017), and 4.2 times in G2 (p = 0.010). Progression-free survival (PFS) was clearly higher in patients with G1WON compared to G1WN and G2 (p = 0.002 and p < 0.001, respectively). There was no significant difference in PFS between G1WN and G2 (p = 0.692). Retreatment was also superior in meningioma with necrosis. Our findings provide clear statistical data to consider that patients with benign meningiomas and histologic findings of spontaneous necrosis are at increased risk of progression and recurrence compared to those with benign lesion without atypical features. Statistical analysis curves also suggest that these lesions behave more similarly to those currently classified as WHO grade II meningioma.





Similar content being viewed by others
References
Ostrom QT, Gittleman H, Fulop J et al (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol 17(Suppl 4):iv1–iv62
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO Classification of Tumours of the Central Nervous System. Acta Neuropathol 114(2):97–109. https://doi.org/10.1007/s00401-007-0243-4
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM (1997) Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 21:1455–1465
Backer-Grøndahl T, Moen BH, Torp SH (2012) The histopathological spectrum of human meningiomas. Int J Clin Exp Pathol 5(3):231–242
Jaaskelainen J, Haltia M, Laasonen E, Wahlstrom T, Valtonen S (1985) The growth rate of intracranial meningiomas and its relation to histology. Surg Neurol 24:165–172
Chen WYK, Liu HC (1990) Atypical (anaplastic) meningiorna: relationship between histological features and recurrence-clinicopathological study. Clin Neuropathol 9:74–81
Christensen D, Laursen H, Klinken L (1983) Prediction of recurrence in meningiomas after surgical treatment. Acta Neuropathol 63:130–134
McLean CA, Jolley D, Cukier E, Giles G, Gonzales MF (1993) Atypical and malignant meningiomas: importance of micronecrosis as a prognostic indicator. Histopathology 23:349–353
Ironside JW, Moss TH, Louis DN, Lowe JS, Weller RO (2002) Meningiomas. In: Ironside JW, Moss TH, Louis DN, Lowe JS, Weller RO (eds) Diagnostic pathology of nervous system tumours. Churchill Livingstone, Edinburgh, pp 344–382
Ho DM, Hsu CY, Ting LT, Chiang H (2002) Histopathology and MIB-1 labeling index predicted recurrence of meningiomas: a proposal of diagnostic criteria for patients with atypical meningioma. Cancer 94:1538–1547
Ng HK, Poon WS, Goh K, Chan MS (1996) Histopathology of post-embolized meningiomas. Am J Surg Pathol 20:1224–1230
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Edwards JG, Swinson DE, Jones JL, Muller S, Waller DA, O’Byrne KJ (2003) Tumor necrosis correlates with angiogenesis and is a predictor of poor prognosis in malignant mesothelioma. Chest 124:1916–1923
Fisher ER, Anderson S, Redmond C, Fisher B (1993) Pathologic findings from the national surgical adjuvant breast project protocol B-06. 10-year pathologic and clinical prognostic discriminants. Cancer 71:2507–2514
Lam JS, Shvarts O, Said JW, Pantuck AJ, Seligson DB, Aldridge ME, Bui MH, Liu X, Horvath S, Figlin RA, Belldegrun AS (2005) Clinicopathologic and molecular correlations of necrosis in the primary tumor of patients with renal cell carcinoma. Cancer 103:2517–2525
Swinson DE, Jones JL, Richardson D, Cox G, Edwards JG, O’Byrne KJ (2002) Tumour necrosis is an independent prognostic marker in non-small cell lung cancer: correlation with biological variables. Lung Cancer 37:235–240
Stefansson IM, Salvesen HB, Akslen LA (2006) Vascular proliferation is important for clinical progress of endometrial cancer. Cancer Res 66:3303–3309
Helczynska K, Kronblad A, Jogi A, Nilsson E, Beckman S, Landberg G, Pahlman S (2003) Hypoxia promotes a dedifferentiated phenotype in ductal breast carcinoma in situ. Cancer Res 63:1441–1444
Vakkila J, Lotze MT (2004) Inflammation and necrosis promote tumour growth. Nat Rev Immunol 4:641–648
Sadri N, Zhang PJ (2013) Hypoxia-inducible factors: mediators of cancer progression; prognostic and therapeutic targets in soft tissue sarcomas. Cancers 5:320–333
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140:883–899
Hockel M, Vaupel P (2001) Tumor hypoxia: definitions and current clinical, biologic, and molecular aspects. J Natl Cancer Inst 93:266–276
Sun SQ, Cai C, Murphy RK et al (2014) Management of atypical cranial meningiomas, part 2: predictors of progression and the role of adjuvant radiation after subtotal resection. Neurosurgery 75:356–363
Bredholt G, Mannelqvist M, Stefansson IM et al (2015) Tumor necrosis is an important hallmark of aggressive endometrial cancer and associates with hypoxia, angiogenesis and inflammation responses. Oncotarget 6(37):39676–39691
Koong AC, Chen EY, Giaccia AJ (1994) Hypoxia causes the activation of nuclear factor kappa B through the phosphorylation of I kappa B alpha on tyrosine residues. Cancer Res 54:1425–1430
Marciscano AR, Stemmer-rachamimov O, Niemierko A, Larvie M, Curry WT, Barker FG, Martuza RL, Mcguone D, Oh KS, Loeffler JS, Shih H (2016) Benign meningiomas (WHO Grade I) with atypical histological features: correlation of histopathological features with clinical outcomes. J Neurosurg 124:106–114
Jellinger K (1988) Histopathological features predicting recurrence of meningiomas after (sub)total resection. Clin Neuropathol 7:174
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interests to report or financial disclosures related to this manuscript.
Rights and permissions
About this article
Cite this article
Góes, P., Santos, B.F.O., Suzuki, F.S. et al. Necrosis is a consistent factor to recurrence of meningiomas: should it be a stand-alone grading criterion for grade II meningioma?. J Neurooncol 137, 331–336 (2018). https://doi.org/10.1007/s11060-017-2721-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2721-4