Abstract
A case of cavitary pulmonary sporotrichosis without mucocutaneous involvement caused by Sporothrix schenckii is reported in a sexagenarian woman with a long smoking history. The patient was hospitalized for septic shock with multiorgan failure from a respiratory focus. The diagnosis was delayed due to the fungal etiological agent was not initially considered in the differential diagnosis. A good clinical and radiological evolution was obtained with the antifungal therapy. Occasional cases of primary pulmonary sporotrichosis have been reported in the literature. Due to its low incidence, this is a less-known and underestimated clinical form. Both clinical suspicion and microbiological studies are needed to reach pulmonary sporotrichosis diagnosis.
Similar content being viewed by others
Introduction
Sporotrichosis is a fungal infection that affects both humans and other animals, caused by different species of the dimorphic fungus Sporothrix [1, 2]. The species involved in human diseases include S. brasiliensis, S. schenckii, S. globosa, S. Mexicana, S. luriei and S. chilensis [1, 3,4,5]. Over the last decade, the incidence of sporotrichosis has increased in tropical and subtropical areas, and atypical clinical forms of this disease were frequently reported [6,7,8].
Sporothrix species have been found as saprophytes on living and decaying vegetation, animal excreta, soil, thorny shrubs and other plant materials. The main route of entry is the cutaneous, through traumatisms or excoriations produced by contaminated material. However, occasional cases of primary pulmonary sporotrichosis have also been reported, suggesting that the infection occurs through inhalation of the fungal conidia from the environment and subsequent inoculation in structurally abnormal lungs [7, 9,10,11,12]. Based on whether it is a primary pulmonary or multifocal infection, two distinct radiological patterns can be observed in pulmonary sporotrichosis, cavitary and non-cavitary with differences in the response to the therapy [7, 9, 10, 13].
The aims of this work were report a case of pulmonary sporotrichosis with cavitary pneumonia without cutaneous involvement, and to achieve a literature review about case reports and publications related to primary pulmonary sporotrichosis.
Case Report
A 65-year-old female patient, housewife, from Resistencia city located in Chaco province in the northeastern Argentina, presented with 3 days of fever, odynophagia, cough with mucopurulent expectoration and dyspnea. The patient referred 37 pack/years smoking history, arterial hypertension and myocardial revascularization surgery with placement of two stents due to acute myocardial infarction 8 months earlier.
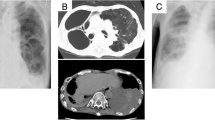
At the moment of admission to intensive care unit, the patient presented septic shock with multiorgan failure from a respiratory focus. The chest X-ray showed right upper lobe cavitation. Serology for HIV, hepatitis A, B and C, toxoplasmosis, cytomegalovirus and syphilis was negative.
During her hospitalized first 2 weeks, the patient required mechanical ventilation, inotropes and hemodialysis. Because of Klebsiella pneumoniae was isolated from sputum sample and subsequently methicillin-resistant Staphylococcus aureus was isolated from endotracheal tube aspiration, she received treatment for 14 days with piperacillin tazobactam and vancomycin. To continue ventilator support, a tracheotomy was performed at third week.
The high-resolution chest tomography (TAC) showed alveolar cavitated consolidation in right upper lobe, bilateral symmetrical pleural effusion, infiltration in right basal alveolar interstitial area with ground glass in the upper left lobe (Fig. 1).
The patient continued with mucopurulent secretions and several antibiotic schemes were realized, without clinical improvement. Due to that, bronchoalveolar lavage (BAL) was performed for microbiological studies. BAL sample was sent to mycology department of Instituto de Medicina Regional, Universidad Nacional del Nordeste, for mycological study.
The patient aggravated clinical and radiologically, so she was referred to a more complex medical center.
Mycological study of the BAL sample revealed the presence of S. schenckii complex. Therefore, a diagnosis of cavitary pulmonary sporotrichosis without mucocutaneous involvement was made. Treatment was started with liposomal amphotericin B 0.7 mg/kg/day to complete 1 g.
Due to a good clinical and radiological evolution, after 60 days of hospitalization, the patient was released, continuing on long-term orally therapy with itraconazole 200 mg/day. The patient did not return to control, so the effectiveness of treatment could not be controlled.
Mycological Study and Molecular Identification
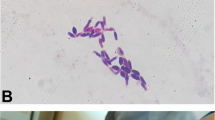
Giemsa stain for direct examination of BAL sample revealed atypical yeast and hyphae (Fig. 2). The sample was inoculated onto brain heart infusion agar containing chloramphenicol (250 mg/L) at 28 and 37 °C. After 14 days of incubation, fungus colonies growth was obtained at 28 °C. The colonies were smooth, wrinkled, pale grey and reverse grey to brownish-black. Micromorphology showed septate, smooth walled, thin and branched hyaline hyphae. Long conidiogenous cells arise from undifferentiated hyphae; apical part forming conidia by sympodial growth adopting a similar arrangement to the petals of a daisy, characteristic of S. schenckii complex. Conidia hyaline, tear-shaped to clavate, smooth and thin walled (3–4 μm diameters).
In order to obtain the yeast phase of the fungus and verify its dimorphism, a subculture in Sabouraud glucose agar at 37 °C was performed. Whitish beige yeast-like colonies were obtained.
To confirm the identification by molecular method, the isolated was sent to Laboratorio de Micosis superficiales y hongos miceliales, Departamento de Micología, INEI-ANLIS “Dr. Carlos Malbrán”, Buenos Aires, Argentina. The sequencing of ITS1, 5.8S, ITS2 and calmodulin using primers CL1 (5-GAR TWC AAG GAG GCC TTCTC-3) and CL2A (5-TTT TTG CAT GAG TTG GAC-3) were performed. The result was compared with published sequences in GenBank using the Basic Local Alignment Search Tool (http://blast.ncbi.nlm.nih.gov/Blast.cgi) showing 99% homology with Sporothrix schenckii EH-234 strain (GenBank accession number KP132784.1).
Discussion
Sporotrichosis, caused by species of the dimorphic fungus of Sporothrix genus, is an occupational disease in gardeners and forestry workers, and the infection is generally acquired by traumatic inoculation through contact with soil, plants, and organic matter contaminated with the fungus [12]. Less commonly, infection can be acquired by inhalation of conidia [2].
The cutaneous forms presenting as firm verrucose/ulcerative/erythematous nodules are the commonest sporotrichosis presentations [10, 12, 14]. Its incidence varies among Latin American countries, with endemic areas in Brazil, Colombia, Costa Rica, Guatemala, Mexico and Uruguay, while is extremely rare in Chile. The estimated prevalence rates range from 0.1 to 0.5% in Brazil, Colombia, El Salvador, Mexico, Uruguay and Venezuela; 0.01 to 0.02% in Argentina, Ecuador and Panama [3, 15,16,17].
Compared with cutaneous forms, pulmonary sporotrichosis is a less-known clinical form. The prevalence and incidence rates of pulmonary sporotrichosis, even in areas of hyperendemicity, are unknown. To date, around 100 cases have been reported [2, 9, 13, 18].
Pulmonary sporotrichosis can be unifocal (primary pulmonary sporotrichosis) involving the respiratory system only [7, 13, 19], or as part of multifocal infection with concurrent disease manifestations in other organs (disseminated) [10, 19,20,21]. It is presumed that the primary pulmonary sporotrichosis is a consequence of direct inhalation of conidia from the environment, while disseminate form is thought to be acquired either by direct inhalation of conidia or possibly by hematogenous/lymphatic dissemination from a distal site favored in immunocompromised patients, being the individual unable to eliminate or contain the infection [9, 22, 23]. Comstock and Wolson were the first to report that pulmonary sporotrichosis can assume as two different radiological patterns, cavitary and non-cavitary form, based on whether it is a primary pulmonary or multifocal infection [10]. They refer that when multiple organs are infected in systemic sporotrichosis, the pulmonary pattern is quite different than when only the lungs are involved. Most of patients with primary pulmonary sporotrichosis display cavitary pattern on radiology [2, 9, 10, 13], different to those with disseminated infection secondary to cutaneous sporotrichosis, that predominantly have bibasal or diffuse reticulonodular infiltrates. In this case, the patient presented the cavitary form, and since no history of trauma or contact with any animal was documented, it was assumed as primary pulmonary sporotrichosis, with probably the fungus penetrated by respiratory tract.
Regardless of the clinical form, primary pulmonary or disseminated, close to 50% of the reported cases with pulmonary involvement have an identifiable potential occupational or environmental exposure to this fungus, such as plant materials, animals or animal products and soil [7, 19]. Additionally, in more than 40% of reported cases, alcohol abuse was noted as a common risk factor. In particular, primary pulmonary sporotrichosis was associated with chronic obstructive pulmonary disease, smoking, alcoholism, chronic use of corticosteroids and immunosuppressive diseases [9, 19, 22, 23].
Considering that our patient referred a long history of smoking, pulmonary compromises might predispose to the clinical form presented in this case.
Primary pulmonary sporotrichosis is a hidden entity, at times mimicking tuberculosis, that usually characterized by cough, low-grade fever, weight loss, mediastinal lymphadenitis, cavitation, fibrosis, and rarely massive hemoptysis [7, 13, 20, 22]. Possibility of pulmonary sporotrichosis should be considered in the patients with chronic cough and cavitary parenchymal disease, particularly in chronic alcoholics, gardeners and forest worker. The diagnosis of this disease is often delayed due to the rarity of pulmonary infection and is usually diagnosed accidentally when the fungus is isolated from the pulmonary discharges of patients with other infections suspected [2]. Moreover, achieve a diagnosis differs from others fungal infections. Sporothrix yeasts are small, scarce and consequently difficult to detect by direct examination of clinical specimens. Observation of yeasts or budding yeasts through direct examination is not conclusive for sporotrichosis diagnosis. Definitive diagnosis is based on the isolation from culture and identification of the etiological agent [2, 20]. This situation occurred in this case, because the possibility of a fungal etiological agent was recently considered as consequence of the lack of clinical improvement and no response to the therapy. Although, yeasts were observed on direct mycological examination, the diagnosis was achieved 14 days later that the fungus was isolated.
The optimal management of pulmonary sporotrichosis remains unclear. Pulmonary sporotrichosis is difficult to treat in both immunocompetent and immunocompromised hosts, especially on cavitary forms. Recommended treatment for pulmonary sporotrichosis is guided in the clinical practice guidelines for the management of sporotrichosis published in 2007 by the Infectious Diseases Society of America (IDSA). In 2011, some of these recommendations were further endorsed by the American Thoracic Society (ATS) in an official statement on the treatment of fungal infections in adult pulmonary and critical care patients. These treatment guidelines were based on a low-level of case report evidences and recommend long term itraconazole as first line agent for less severe disease [24, 25]. Although, the triazole agent efficacy in cutaneous and articular sporotrichosis treatment is well-established, current experience with itraconazole in pulmonary sporotrichosis is still very limited. Amphotericin B is reserved for severe or life-threatening situations, followed by oral daily itraconazole. In patients with localized pulmonary involvement and/or display radiological features of advanced cavitary disease, combination with surgery is recommended [9, 22, 24, 25]. In this case, patient was treated with liposomal amphotericin B in usual doses, but not subjected to surgery, with good improvement. Consequently, the patient was discharged home on-long term itraconazole therapy, as recommended the clinical practice guidelines [24].
More than 90% of pulmonary sporotrichosis cases reported in literature inform S. schenckii as the etiologic agent, but identification of these isolates were performed by conventional methods [7, 13, 19]. Considering the taxonomy revision of this genus, apply molecular technics is necessary to differentiate species within the Sporothrix complex [4, 11]. To our knowledge, this is the first case of S. schenckii pulmonary infection reported in Argentina.
Conclusion
Pulmonary sporotrichosis is a rare fungal infection. Include this etiology is important for differential diagnosis in patients with cavitary pneumonia without response to conventional antibiotic treatments. Because of sporotrichosis diagnosis is based on the isolation and identification of the etiological agent, mycological cultures are needed to achieve the diagnosis.
References
Rodrigues AM, Teixeira MM, de Hoog GS, Schubach TMP, Pereira SA, Fernandes GF, et al. Phylogenetic analysis reveals a high prevalence of Sporothrix brasiliensis in feline sporotrichosis outbreaks. PLoS Negl Trop Dis. 2013;7(6):e2281.
Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev. 2011;24:633–54.
Rodrigues AM, Cruz Choappa R, Fernandes GF, de Hoog GS, de Camargo ZP. Sporothrix chilensis sp. nov. (Ascomycota: Ophiostomatales), a soil-borne agent of human sporotrichosis with mild-pathogenic potential to mammals. Fungal Biol. 2016;120:246–64.
Marimon R, Gene J, Cano J, Trilles L, Dos Santos Lazera M, Guarro J. Molecular phylogeny of Sporothrix schenckii. J Clin Microbiol. 2006;44:3251–6.
Marimon R, Gené J, Cano J, Guarro J. Sporothrix luriei: a rare fungus from clinical origin. Med Mycol. 2008;46:621–5.
Ramírez-Soto M, Lizárraga-Trujillo J. Esporotricosis granulomatosa: presentación de dos casos inusuales. Rev Chil Infectol. 2013;30:548–53.
Bravo TC, Carrada B. Esporotricosis pulmonar cavitada: diagnóstico y tratamiento. Med Interna Méx. 2006;22:457–61.
Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53:3–14.
Aung AK, Teh BM, McGrath C, Thompson PJ. Pulmonary sporotrichosis: case series and systematic analysis of literature on clinico-radiological patterns and management outcomes. Med Mycol. 2013;51:534–44.
Comstock C, Wolson AH. Roentgenology of sporotrichosis. Am J Roentgenol Radium Ther Nucl Med. 1975;125:651–5.
Rodrigues AM, de Hoog S, de Camargo ZP. Emergence of pathogenicity in the Sporothrix schenckii complex. Med Mycol. 2013;51:405–12.
Cabrera ER, Ramirez PP, Torrico FT. Lymphangitic sporotrichosis: case report. Gac Med Bol. 2010;33:55–8.
Beland JE, Mankiewicz E, MacIntosh D. Primary pulmonary sporotrichosis. Can Med Assoc J. 1968;99:813–6.
Freitas DFS, do Valle ACF, de Almeida Paes R, Bastos FI, Galhardo MCG. Zoonotic sporotrichosis in Rio de Janeiro, Brazil: a protracted epidemic yet to be curbed. Clin Infect Dis. 2010;50:453.
Díaz Conti I. Epidemiology of sporotrichosis in Latin America. Mycopathologia. 1989;108:113–6.
Bustamante B, Campos PE. Endemic sporotrichosis. Curr Opin Infect Dis. 2001;14:145–9.
Queiroz-Telles F, Nucci M, Colombo AL, Tobón A, Restrepo A. Mycoses of implantation in Latin America: an overview of epidemiology, clinical manifestations, diagnosis and treatment. Med Mycol. 2011;49:225–36.
Aung A, Spelman D, Thompson P. Pulmonary sporotrichosis: an evolving clinical paradigm. Semin Respir Crit Care Med. 2015;36:756–66.
Rawat V, Jha P, Goyal R, Singhai M, Verma P, Shree D, et al. Primary pulmonary sporotrichosis in a sub-himalayan patient. J Lab Physicians. 2012;4:48.
Haponik E, Hill M, Craighead C. Pulmonary sporotrichosis with massive hemoptysis. Am J Med Sci. 1989;297:251–3.
Ramirez J, Byrd R, Roy T. Chronic cavitary pulmonary sporotrichosis: efficacy of oral itraconazole. J Ky Med Assoc. 1998;96:103–5.
Orofino-Costa R, Unterstell N, Carlos Gripp A, de Macedo PM, Brota A, Dias E, et al. Pulmonary cavitation and skin lesions mimicking tuberculosis in a HIV negative patient caused by Sporothrix brasiliensis. Med Mycol Case Rep. 2013;2:65–71.
Silva-Vergara ML, de Camargo ZP, Silva PF, Abdalla MR, Sgarbieri RN, Rodrigues AM, et al. Disseminated sporothrix brasiliensis infection with endocardial and ocular involvement in an HIV-infected patient. Am J Trop Med Hyg. 2012;86:477–80.
Kauffman CA, Bustamante B, Chapman SW, Pappas PG. clinical practice guidelines for the management of sporotrichosis: update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;2007(45):1255–65.
Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A, et al. An official American Thoracic Society statement: treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011;183:96–128.
Acknowledgements
We gratefully acknowledge to Prof. Mariana Climent for checked the English of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rojas, F.D., Fernández, M.S., Lucchelli, J.M. et al. Cavitary Pulmonary Sporotrichosis: Case Report and Literature Review. Mycopathologia 182, 1119–1123 (2017). https://doi.org/10.1007/s11046-017-0197-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-017-0197-6