Abstract
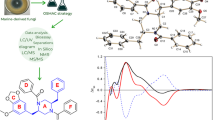
The important role of histone deacetylases (HDACs) in the development of cancer has been demonstrated by various studies. Thus targeting HDACs with inhibitors is a major focus in anticancer drug research. Although few synthetic HDAC inhibitors (HDIs) have been approved for cancer treatment, they have significant undesirable side effects. Therefore emphases have been placed on natural HDIs as substitutes for the synthetic ones. In a bid to identify more HDIs, this study evaluated the binding tendency of compounds derived from Morinda lucida Benth. towards selected HDACs for the discovery of potent HDIs as potential candidates for anticancer therapeutics, based on the report of anticancer potentials of Morinda lucida-derived extracts and compounds. Givinostat and 49 Morinda-lucida derived compounds were docked against selected HDAC isoforms using AutodockVina, while binding interactions were viewed with Discovery Studio Visualizer, BIOVIA, 2016. Druglikeness and Absorption–Distribution–Metabolism–Excretion (ADME) parameters of the top 7 compounds were evaluated using the Swiss online ADME web tool. The results revealed that out of the 49 compounds, 3 phytosterols (campesterol, cycloartenol, and stigmasterol) and 2 triterpenes (oleanolic acid and ursolic acid) exhibited high HDAC inhibitory activity compared to givinostat. These 5 compounds also fulfill oral drugability of Lipinski rule of five. Morinda lucida-derived phytosterols and triterpenes show high binding tendency towards the selected HDACs and exhibited good drugability characteristics and are therefore good candidates for further studies in the search for therapies against abnormalities linked with over-activity of HDACs.










Similar content being viewed by others
References
Reddy DS, Wu X, Golub VM et al (2018) Measuring histone deacetylase inhibition in the brain. Curr Protoc Pharmacol 1–14. https://doi.org/10.1002/cpph.41
Singh AK, Bishayee A, Pandey AK (2018) Targeting histone deacetylases with natural and synthetic agents: an emerging strategy. Nutrients 10:1–31. https://doi.org/10.3390/nu10060731
Kumar S, Ahmad M, Waseem M, Pandey AK (2015) Drug targets for cancer treatment: an overview. Med Chem (Los Angeles) 5:115–123
Sharma U, Sharma A, Pandey AK (2016) Medicinal attributes of major phenylpropanoids present in cinnamon. BMC Complement Altern Med 16:156
Eckschlager T, Plch J, Stiborova M, Hrabeta J (2017) Histone deacetylase inhibitors as anticancer drugs. Int J Mol Sci 18:1–25. https://doi.org/10.3390/ijms18071414
Ganai SA, Farooq Z, Banday S, Altaf M (2018) In silico approaches for investigating the binding propensity of apigenin and luteolin against class i HDAC isoforms. Future Med Chem. https://doi.org/10.4155/fmc-2018-0020
Seto E, Yoshida M (2014) Erasers of histone acetylation: the histone deacetylase enzymes. Cold Spring Harb Perspect Biol 6:a018713
Barneda-Zahonero B, Parra M (2012) Histone deacetylases and cancer. Mol Oncol 6:579–589. https://doi.org/10.1016/j.molonc.2012.07.003
De Ruijter A, Van Gennip A, Caron H et al (2003) Histone deacetylases (HDACs): characterization of the classical HDAC family. Biochem J 370:737–749
Ganai S (2016) Novel approaches towards designing of isoform-selective inhibitors against class ii histone deacetylases: the acute requirement for targetted anticancer therapy. CurrTopMedChem 16:2441–2452
Mottamal M, Zheng S, Huang T, Wang G (2015) Histone deacetylase inhibitors in clinical studies as templates for new anticancer agents. Molecules 20:3898–3941
Ropero S, Esteller M (2007) The role of histone deacetylases (HDACs) in human cancer. Mol Oncol 1:19–25. https://doi.org/10.1016/j.molonc.2007.01.001
Wilson A, Byun D, Popova N (2006) Histone deacetylase 3 (HDAC3) and other class I HDACs regulate colon cell maturation and p21 expression and are deregulated in human colon cancer. J Biol Chem 281:13548–13558
Lagger S, Meunier DMM et al (2010) Crucial function ofhistone deacetylase 1 for differentiation of teratomas in mice and humans. EMBO J 29:3992–4007
Halkidou K, Gaughan L, Cook S et al (2004) Upregulation and nuclear recruitment of HDAC1 in hormone refractory prostate cancer. Prostate 59:177–189
Song J, Noh J, Lee J (2005) Increased expression ofhistone deacetylase 2 is found in human gastric cancer. APMIS 113:264–268
Huang B, Laban M, Leung C (2005) Inhibition of histone deacetylase 2 increases apoptosis and p21Cip1/WAF1 expression, independent ofhistone deacetylase 1. Cell Death Differ 12:395–404
Muller BM, Jana LKA et al (2013) Differential expression of histone deacetylases HDAC1, 2 and 3 in human breast cancer-overexpression ofHDAC2 and HDAC3 is associated with clinicopathological indicators of disease progression. BMC Cancer 13:215
Spurling C, Godman C, Noonan E et al (2008) HDAC3 overexpression and colon cancer cell proliferation and differentiation. Mol Carcinog 47:137–147
Oehme I, Deubzer H, Wegener D (2009) Histone deacetylase 8 in neuroblastoma tumorigenesis. Clin Cancer Res 5:91–99
Park S, Jun J, Jeong K (2011) Histone deacetylases 1, 6 and 8 are critical for invasion in breast cancer. Oncol Rep 25:677–1681
Ahn M-Y, Yoon J-H (2017) Histone deacetylase 7 silencing induces apoptosis and autophagy in salivary mucoepidermoid carcinoma cells. J Oral Pathol Med 46:276–283. https://doi.org/10.1111/ijlh.12426
Pandey M, Kaur P, Shukla S et al (2012) Plant flavone apigenin inhibits HDAC and remodels chromatin to induce growth arrest and apoptosis in human prostate cancer cells: in vitro and in vivo study. Mol Carcinog 51:952–962
Attoub S, Hassan A, Vanhoecke B (2011) Inhibition of cell survival, invasion, tumor growth and histone deacetylase activity by the dietary flavonoid luteolin in human epithelioid cancer cells. Eur J Pharmacol 651:18–25
Soflaei SS, Momtazi-Borojeni AA, Majeed M et al (2018) Curcumin: a natural Pan-HDAC inhibitor in cancer. Curr Pharm Des 24:123–129. https://doi.org/10.2174/1381612823666171114165051
Murugan K, Sangeetha S, Ranjitha S et al (2015) HDACiDB: a database for histone deacetylase inhibitors. Drug Des Devel Ther 9:2257–2264
Sowemimo AA, Fakoya FA, Awopetu I et al (2007) Toxicity and mutagenic activity of some selected Nigerian plants. J Ethnopharmacol 113:427–432. https://doi.org/10.1016/j.jep.2007.06.024
Ashidi JS, Houghton PJ, Hylands PJ, Efferth T (2010) Ethnobotanical survey and cytotoxicity testing of plants of South-western Nigeria used to treat cancer, with isolation of cytotoxic constituents from Cajanus cajan Millsp. leaves. J Ethnopharmacol 128:501–512. https://doi.org/10.1016/j.jep.2010.01.009
Durodola JI (1974) Anti-neoplastic property of crystalline compound extracted from Morinda lucida. Planta Med 26:208–211
Appiah-opong R, Tuffour I, Annor GK et al (2016) Antiproliferative, antioxidant activities and apoptosis induction by Morinda lucida and Taraxacum officinale in human HL-60 leukemia cells. J Glob Biosci 5:4281–4291
Nweze NE (2012) In vitro anti-trypanosomal activity of Morinda lucida leaves. African J Biotechnol 11:1812–1817. https://doi.org/10.5897/AJB11.862
Samje M, Metuge J, Mbah J et al (2014) In vitro anti- Onchocerca ochengi activities of extracts and chromatographic fractions of Craterispermum laurinum and Morinda lucida. BMC Complement Altern Med 14:1–12. https://doi.org/10.1186/1472-6882-14-325
Suzuki M, Tung HN, Kwofie KD et al (2015) New anti-trypanosomal active tetracyclic iridoid isolated from Morinda lucida Benth. Biorgan Med Chem Lett http://dx:1–4. https://doi.org/10.1016/j.bmcl.2015.05.003
O’Boyle NM, Banck M, James CA et al (2011) Open babel: an open chemical toolbox. J Cheminform 3:33. https://doi.org/10.1186/1758-2946-3-33
Trott O, Olson AJ (2010) AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J Comput Chem 31:455–461
McGinnity DF, Collington J, Austin RP, Riley RJ (2007) Evaluation of human pharmacokinetics, therapeutic dose and exposure predictions using marketed oral drugs. Curr Drug Metab. https://doi.org/10.2174/138920007780866799
Paul Gleeson M, Hersey A, Hannongbua S (2011) In-silico ADME models: a general assessment of their utility in drug discovery applications. Curr Top Med Chem. https://doi.org/10.2174/156802611794480927
Daina A, Michielin O, Zoete V (2014) ILOGP: a simple, robust, and efficient description of n-octanol/water partition coefficient for drug design using the GB/SA approach. J Chem Inf Model 54:3284–3301. https://doi.org/10.1021/ci500467k
Daina A, Zoete V (2016) A BOILED-egg to predict gastrointestinal absorption and brain penetration of small molecules. ChemMedChem 11:1117–1121
Daina A, Michielin O, Zoete V (2017) SwissADME: a free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci Rep 7:42717. https://doi.org/10.1038/srep42717
Huang SY, Zou X (2010) Advances and challenges in protein-ligand docking. Int J Mol Sci 11(8):3016–3034
Raj RA, John Milton MC, Prakasam A et al (2018) In silico molecular docking of bioactive compound Pregnan-20-one,5,6-epoxy-3,17,dihydroxy-16 methyl-[3a,5a,6a,16a] with brain cancer protein(1qh4): a promising molecular target. 9:51–55
Hsu KC, Liu CY, Lin TE et al (2017) Novel class IIA-selective histone deacetylase inhibitors discovered using an in silico virtual screening approach. Sci Rep 7(1):3228. https://doi.org/10.1038/s41598-017-03417-1
Yoon S, Eom GH (2016) HDAC and HDAC inhibitor: from cancer to cardiovascular diseases. Chonnam Med J 52(1):1 https://doi.org/10.4068/cmj.2016.52.1.1
Tambunan USF, Bramantya N, Parikesit AA (2011) In silico modification of suberoylanilide hydroxamic acid (SAHA) as potential inhibitor for class II histone deacetylase (HDAC). BMC Bioinform. https://doi.org/10.1186/1471-2105-12-S13-S23
Awad AB, Fink CS (2000) Phytosterols as anticancer dietary components: evidence and mechanism of action. J Nutr 130:2127–2130
Zhang Z, Luo Z, Shi H et al (2017) Research advance of functional plant pharmaceutical cycloartenol about pharmacological and physiological activity. J Chinese Mater medica 42:433–437
da Silva I, Kaluderovic G, de Oliveira P et al (2018) Apoptosis caused by triterpenes and phytosterols and antioxidant activity of an enriched flavonoid extract from Passiflora mucronata. Anticancer Agents Med Chem. https://doi.org/10.2174/1871520618666180315090949
Choi J, Lee E, Lee H et al (2007) Identification of campesterol from Chrysanthemum coronarium L. and its antiangiogenic activities. Phyther Res 21:954–959. https://doi.org/10.1002/ptr
Kangsamaksin T, Chaithongyot S, Wootthichairangsan C (2017) Lupeol and stigmasterol suppress tumor angiogenesis and inhibit cholangiocarcinoma growth in mice via downregulation of tumor necrosis factor- α. PLoS One 12:1–16. https://doi.org/10.1371/journal.pone.0189628
Petronelli A, Pannitteri G, Testa U (2009) Triterpenoids as new promising anticancer drugs. Anticancer Drugs 20:880–892. https://doi.org/10.1097/CAD.0b013e328330fd90
Chen I, Lu M, Du Y et al (2009) Cytotoxic triterpenoids from the stems of Microtropis japonica. J Nat Prod 72:6–11
Lipinski CA (2000) Drug-like properties and the causes of poor solubility and poor permeability. J Pharmacol Toxicol Methods 44:235–249
Liu J (1995) Pharmacology of oleanolic acid and ursolic acid. J Ethnopharmacol 49:57–68
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ishola, A.A., Adewole, K.E. Phytosterols and triterpenes from Morinda lucida Benth. exhibit binding tendency against class I HDAC and HDAC7 isoforms. Mol Biol Rep 46, 2307–2325 (2019). https://doi.org/10.1007/s11033-019-04689-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-019-04689-8