Abstract
Medical practice is ideally based on robust, relevant research. However, the lack of disease-modifying treatments for Alzheimer’s disease has motivated “innovative practice” to improve patients’ well-being despite insufficient evidence for the regular use of such interventions in health systems treating millions of patients. Innovative or new non-validated practice poses at least three distinct ethical questions: first, about the responsible application of new non-validated practice to individual patients (clinical ethics); second, about the way in which data from new non-validated practice are communicated via the scientific and lay press (scientific communication ethics); and third, about the prospect of making new non-validated interventions widely available before more definitive testing (public health ethics). We argue that the authors of metabolic enhancement protocols for Alzheimer’s disease have overstated the evidence in favor of these interventions within the scientific and lay press, failing to communicate weaknesses in their data and uncertainty about their conclusions. Such unmeasured language may create false hope, cause financial harm, undermine informed consent, and frustrate the production of generalizable knowledge necessary to face the societal problems posed by this devastating disease. We therefore offer more stringent guidelines for responsible innovation in the treatment of Alzheimer’s disease.
Similar content being viewed by others
Notes
For reference, the methods are respectively abbreviated as follows: quantitative electroencephalogram (qEEG), Montreal cognitive assessment (MoCA), magnetic resonance imaging (MRI), Saint Louis University Mental Status (SLUMS), fluorodeoxyglucose-positron emission tomography (FDG-PET), and mini-mental state examination (MMSE).
References
Beauchamp, Tom L., and Yashar Saghai. 2012. The historical foundations of the research-practice distinction in bioethics. Theoretical Medicine and Bioethics 33: 45–56.
National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. 1979. The Belmont report: Ethical principles and guidelines for the protection of human subjects of research. Washington, DC: US Government Printing Office.
Davis, Dena S. 2017. Ethical issues in Alzheimer’s disease research involving human subjects. Journal of Medical Ethics 43: 852–856.
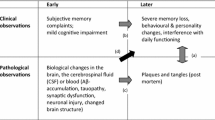
Jack, Clifford R., Jr., David A. Bennett, Kaj Blennow, Maria C. Carrillo, Billy Dunn, Samantha Budd Haeberlein, David M. Holtzman, et al. 2018. NIA-AA research framework: Toward a biological definition of Alzheimer’s disease. Alzheimer’s and Dementia 14: 535–562.
Selkoe, Dennis J., and John Hardy. 2016. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Molecular Medicine 8: 595–608.
Livingston, Gill, Andrew Sommerlad, Vasiliki Orgeta, Sergi G. Costafreda, Jonathan Huntley, Davis Ames, Clive Ballard, et al. 2017. Dementia prevention, intervention, and care. Lancet 390: 2673–2734.
Taylor, Patrick L. 2010. Overseeing innovative therapy without mistaking it for research: A function-based model based on old truths, new capacities, and lessons from stem cells. Journal of Law, Medicine and Ethics 38: 286–302.
World Medical Association. 2013. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310: 2191–2194.
Earl, Jake. 2019. Innovative practice, clinical research, and the ethical advancement of medicine. American Journal of Bioethics 19(6): 7–18.
Agich, George J. 2019. Knowing one’s way around: The challenge of identifying and overseeing innovations in patient care. American Journal of Bioethics 19(6): 1–3.
Levine, Robert J. 1979. Clarifying the concepts of research ethics. Hastings Center Report 9(3): 21–26.
Mastroleo, Ignacio, and Felicitas Holzer. 2019. New non-validated practice: An enhanced definition of innovative practice for medicine. Law, Innovation and Technology 12: 318–346.
Haber, Noah, Emily R. Smith, Ellen Moscoe, Kathryn Andrews, Robin Audy, Winnie Bell, Alana T. Brennan, et al. 2018. Causal language and strength of inference in academic and media articles shared in social media (CLAIMS): A systematic review. PLoS ONE 13(5): e0196346. https://doi.org/10.1371/journal.pone.0196346.
London, Alex John. 2019. Social value, clinical equipoise, and research in a public health emergency. Bioethics 33: 326–334.
Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, and Carol Brayne. 2020. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: 413–446.
Sohn, Emily. 2018. A quest to stave off the inevitable: The idea that certain lifestyle choices could help to prevent Alzheimer’s disease is gaining broader acceptance. Nature 559: S18–S20.
Bredesen, Dale E. 2014. Reversal of cognitive decline: A novel therapeutic program. Aging 6: 707–717.
Bredesen, Dale E., Edwin C. Amos, Jonathan Canick, Mary Ackerley, Cyrus Raji, Milan Fiala, and Jamila Ahdidan. 2016. Reversal of cognitive decline in Alzheimer’s disease. Aging 8: 1250–1258.
Bredesen, Dale E., Kenneth Sharlin, David Jenkins, Miki Okuno, Wes Youngberg, Sharon Hausman Cohen, Anne Stefani, et al. 2018. Reversal of cognitive decline: 100 patients. Journal of Alzheimer’s Disease and Parkinsonism 8(5): 1000450. https://doi.org/10.4172/2161-0460.1000450.
Apollo Health. 2020. Frequently asked questions. https://web.archive.org/web/20200716220221/https://www.apollohealthco.com/frequently-asked-questions. Accessed July 16, 2020.
Gustafson, Craig. 2015. Dale E. Bredesen, MD: Reversing cognitive decline. Integrative Medicine 14(5): 26–29.
Impact Journals. 2020. Publication ethics and publication malpractice statements. Aging. https://www.aging-us.com/ethics. Accessed March 2, 2020.
Impact Journals. 2020. Information for authors. Aging. https://www.aging-us.com/for-authors. Accessed March 2, 2020.
Gluckman, Eliane, Hal E. Broxmeyer, Arleen D. Auerbach, Henry S. Friedman, Gordon W. Douglas, Agnès Devergie, Hélène Esperou, et al. 1989. Hematopoietic reconstitution in a patient with Fanconi’s anemia by means of umbilical-cord blood from an HLA-identical sibling. New England Journal of Medicine 321: 1174–1178.
Bredesen, Dale E. 2017. The end of Alzheimer’s: The first program to prevent and reverse cognitive decline. New York: Avery.
CBN News. 2019. New research proves Alzheimer’s symptoms can be reversed naturally. CBN News. https://www1.cbn.com/cbnnews/health/2019/april/new-research-proves-alzheimers-symptoms-can-be-reversed-naturally. Accessed April 24, 2019.
Apollo Health. 2020. Hope through science. https://web.archive.org/web/20200525224055/. https://www.apollohealthco.com. Accessed May 25, 2020.
Apollo Health. 2020. Leadership. https://web.archive.org/web/20200525193926/. https://www.apollohealthco.com/leadership. Accessed May 25, 2020.
Institute for Functional Medicine. 2020. Functional medicine determines how and why illness occurs and restores health by addressing the root causes of disease for each individual. https://web.archive.org/web/20200421095351/https://www.ifm.org/functional-medicine. Accessed April 21, 2020.
Mack, Amy. 2017. AAFP Announces decision on functional medicine CME. Institute for Functional Medicine. https://www.ifm.org/news-insights/news-aafp-announces-decision-functional-medicine-cme. Accessed September 15, 2017.
Institute for Functional Medicine. 2014. The evidence. https://web.archive.org/web/20140714233846/http://functionalmedicine.org/what_is_functional_medicine/why/evidence. Accessed July 14, 2014.
Djulbegovic, Benjamin. 2001. Acknowledgment of uncertainty: A fundamental means to ensure scientific and ethical validity in clinical research. Current Oncology Reports 3(5): 389–395.
Cacciamani, Federica, Caroline Tandetnik, Geoffroy Gagliardi, Hugo Bertin, Marie-Odile Habert, Harald Hampel, Laurie Boukadida, Marie Révillon, Stephane Epelbaum, and Bruno Dubois. 2017. Low cognitive awareness, but not complaint, is a good marker of preclinical Alzheimer’s disease. Journal of Alzheimer’s Disease 59: 753–762.
Dresser, Rebecca. 1993. Defining scientific misconduct: The relevance of mental state. JAMA 269: 895–897.
Beall, Jeffrey. 2010. Update: Predatory open-access scholarly publishers. Charleston Advisor 12: 50. https://doi.org/10.5260/chara.12.1.50.
Kaiser, Jocelyn. 2013. U.S. government accuses Open Access publisher of trademark infringement. Science, May 9, 2013. https://www.sciencemag.org/news/2013/05/us-government-accuses-open-access-publisher-trademark-infringement.
Beall, Jeffrey. 2017. List of standalone journals. Scholarly Open Access. Updated January 9, 2017. https://web.archive.org/web/20170111172309/https://scholarlyoa.com/individual-journals.
Ngandu, Tiia, Jenni Lehtisalo, Alina Solomon, Esko Levälahti, Satu Ahtiluoto, Riitta Antikainen, Lars Bäckman, Tuomo Hänninen, et al. 2015. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 385: 2255–2263.
Vandenbroucke, Jan P., Erik von Elm, Douglas G. Altman, Peter C. Gøtzsche, Cynthia D. Mulrow, Stuart J. Pocock, Charles Poole, James J. Schlesselman, and Matthias Egger. 2014. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. International Journal of Surgery 12: 1500–1524.
Society of Professional Journalists. 2014. Code of ethics. Revised September 6, 2014. https://www.spj.org/ethicscode.asp.
Kimmelman, Jonathan, and Alex John London. 2015. The structure of clinical translation: Efficiency, information, and ethics. Hastings Center Report 45(2): 27–39.
Hebert, Liesi E., Jennifer Weuve, Paul A. Scherr, and Denis A. Evans. 2013. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology 80: 1778–1783.
Congressional Budget Office. 2020. The budget and economic outlook: 2020 to 2030. Washington, DC: Congressional Budget Office. https://www.cbo.gov/system/files/2020-01/56020-CBO-Outlook.pdf.
C.K. 2018. Beware! Review of The end of Alzheimer’s: The first program to prevent and reverse cognitive decline, by Dale E. Bredesen. Amazon.com, August 28, 2018. https://www.amazon.com/gp/customer-reviews/R1YWBSWB9HIUN2/ref=cm_cr_getr_d_rvw_ttl?ie=UTF8&ASIN=0735216207.
Rosenberg, A., F. Mangialasche, T. Ngandu, A. Solomon, and M. Kivipelto. 2020. Multidomain interventions to prevent cognitive impairment, Alzheimer’s disease, and dementia: From FINGER to World-Wide FINGERS. Journal of Prevention of Alzheimer’s Disease 7: 29–36.
Baker, Laura D., Daniel P. Beavers, MaryJo Cleveland, Claire E. Day, Charles Decarli, Mark A. Espeland, Sarah E. Tomaszewski-Farias, et al. 2019. O4–11-03: U.S. Pointer: Study design and launch. Alzheimer’s and Dementia 15(7S): P1262–P1263. https://doi.org/10.1016/j.jalz.2019.06.4802.
Richards, Bernadette, and Katrina Hutchison. 2016. Consent to innovative treatment: No need for a new legal test. Journal of Law and Medicine 23: 938–948.
QuesGen Systems. 2020. Reversal of Cognitive Decline (ReCODE) Study (RECODE) (Identifier NCT03883633). Updated March 18, 2020. https://clinicaltrials.gov/ct2/show/NCT03883633.
Hellmuth, Joanna. 2020. Can we trust The End of Alzheimer’s? Lancet Neurology 19: 389–390.
Pan American Health Organization. 2020. Reliance for emergency use authorization of medicines and other health technologies in a pandemic (e.g. COVID-19). https://covid19-evidence.paho.org/handle/20.500.12663/1189
Kimmelman, Jonathan, and Carole Federico. 2017. Consider drug efficacy before first-in-human trials. Nature 542: 25–27. https://doi.org/10.1038/542025a.
Acknowledgments
The authors thank Katelyn MacDougald for her invaluable copyediting. Timothy Daly thanks the Fondation Médéric Alzheimer for financial support for his doctoral work, and acknowledges helpful support and input from Hervé Maisonneuve, Anouk Barberousse, Mathieu Bourdenx, and Felicitas Holzer.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Daly, T., Mastroleo, I., Gorski, D. et al. The ethics of innovation for Alzheimer’s disease: the risk of overstating evidence for metabolic enhancement protocols. Theor Med Bioeth 41, 223–237 (2020). https://doi.org/10.1007/s11017-020-09536-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11017-020-09536-7