Abstract
A novel two-layered pain-relieving wound dressing was prepared from a combination of biocompatible polymers: carboxymethylcellulose and polyethyleneoxide, and two types of pain-relieving drugs: the non-steroid anti-inflammatory diclofenac and the local anesthetic lidocaine. To achieve the two-layered structure, electrospinning and impregnation of a commercially available wound dressing Aquacel® were used for preparation of respective layers. The electrospun nanofibers have been shown to possess similar features as found in the extracellular matrix, an important component of the skin. This characteristic could significantly contribute to the efficiency of wound healing. The second layer is based on Aquacel®, an important wound dressing in modern wound care. Since pain can drastically lower the wound healing process, as well as it is known to decrease the overall quality of patient life, pain-relieving drugs are very interesting for wound care applications. For efficient pain reduction, two types of drugs were used. When combined, these can cover different types of wound-related pain (due to the cause and treatment) and hence additionally aid the wound healing process. The combined features of the incorporated pain-relieving drugs and the mentioned materials are therefore very interesting for future studies toward clinical testing of possible prototype products.
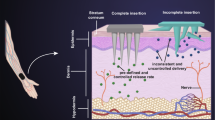
Graphical Abstract








Similar content being viewed by others
References
Alamein MA, Liu Q, Stephens S, Skabo S, Warnke F, Bourke R, Heiner P, Warnke PH (2013) Nanospiderwebs: artificial 3D extracellular matrix from nanofibers by novel clinical grade electrospinning for stem cell delivery. Adv Healthc Mater 2(5):702–717
Francis MP, Sachs PC, Madurantakam PA, Sell SA, Elmore LW, Bowlin GL, Holt SE (2012) Electrospinning adipose tissue-derived extracellular matrix for adipose stem cell culture. J Biomed Mater Res A 100(7):1716–1724
Tuzlakoglu K, Santos MI, Neves N, Reis RL (2011) Design of nano- and microfiber combined scaffolds by electrospinning of collagen onto starch-based fiber meshes: a man-made equivalent of natural extracellular matrix. Tissue Eng A 17(3–4):463–473
Frantz C, Stewart KM, Weaver VM (2010) The extracellular matrix at a glance. J Cell Sci 123(24):4195–4200
Mouw JK, Ou G, Weaver VM (2014) Extracellular matrix assembly: a multiscale deconstruction. Nat Rev Mol Cell Biol 15(12):771–785
Dubsky M, Kubinova S, Sirc J, Voska L, Zajicek R, Zajicova A, Lesny P, Jirkovska A, Michalek J, Munzarova M, Holan V, Sykova E (2012) Nanofibers prepared by needleless electrospinning technology as scaffolds for wound healing. J Mater Sci Mater Med 23(4):931–941
Rho KS, Jeong L, Lee G, Seo BM, Park YJ, Hong SD, Roh S, Cho JJ, Park WH, Min BM (2006) Electrospinning of collagen nanofibers: effects on the behavior of normal human keratinocytes and early-stage wound healing. Biomaterials 27(8):1452–1461
Abrigo M, McArthur SL, Kingshott P (2014) Electrospun nanofibers as dressings for chronic wound care: advances, challenges, and future prospects. Macromol Biosci 14(6):772–792
He T, Wang J, Huang P, Zeng B, Li H, Cao Q, Zhang S, Luo Z, Deng DY, Zhang H, Zhou W (2015) Electrospinning polyvinylidene fluoride fibrous membranes containing anti-bacterial drugs used as wound dressing. Colloids Surf B 130:278–286
Choi JS, Kim HS, Yoo HS (2015) Electrospinning strategies of drug-incorporated nanofibrous mats for wound recovery. Drug Deliv Transl Res 5(2):137–145
Arslan A, Simsek M, Aldemir SD, Kazaroglu NM, Gumusderelioglu M (2014) Honey-based PET or PET/chitosan fibrous wound dressings: effect of honey on electrospinning process. J Biomater Sci Polym Ed 25(10):999–1012
Paaver U, Tamm I, Laidmae I, Lust A, Kirsimae K, Veski P, Kogermann K, Heinamaki J (2014) Soluplus graft copolymer: potential novel carrier polymer in electrospinning of nanofibrous drug delivery systems for wound therapy. BioMed Res Int 2014:789765
Zhou Y, Yang H, Liu X, Mao J, Gu S, Xu W (2013) Electrospinning of carboxyethyl chitosan/poly(vinyl alcohol)/silk fibroin nanoparticles for wound dressings. Int J Biol Macromol 53:88–92
Hong Y, Li Y, Zhuang X, Chen X, Jing X (2009) Electrospinning of multicomponent ultrathin fibrous nonwovens for semi-occlusive wound dressings. J Biomed Mater Res A 89(2):345–354
Sampson SL, Saraiva L, Gustafsson K, Jayasinghe SN, Robertson BD (2014) Cell electrospinning: an in vitro and in vivo study. Small 10(1):78–82
Jayasinghe SN (2013) Cell electrospinning: a novel tool for functionalising fibres, scaffolds and membranes with living cells and other advanced materials for regenerative biology and medicine. Analyst 138(8):2215–2223
Townsend-Nicholson A, Jayasinghe SN (2006) Cell electrospinning: a unique biotechnique for encapsulating living organisms for generating active biological microthreads/scaffolds. Biomacromolecules 7(12):3364–3369
Salalha W, Kuhn J, Dror Y, Zussman E (2006) Encapsulation of bacteria and viruses in electrospun nanofibres. Nanotechnology 17(18):4675
Gantwerker EA, Hom DB (2012) Skin: histology and physiology of wound healing. Clin Plast Surg 39(1):85–97
Petrulyte S (2008) Advanced textile materials and biopolymers in wound management. Dan Med Bull 55(1):72–77
Solowiej K, Mason V, Upton D (2010) Psychological stress and pain in wound care, part 2: a review of pain and stress assessment tools. J Wound Care 19(3):110–115
Price P, Fogh K, Glynn C, Krasner DL, Osterbrink J, Sibbald RG (2007) Why combine a foam dressing with ibuprofen for wound pain and moist wound healing? Int Wound J 4(Suppl 1):1–3
Maver T, Maver U, Mostegel F, Griesser T, Spirk S, Smrke D, Stana-Kleinschek K (2015) Cellulose based thin films as a platform for drug release studies to mimick wound dressing materials. Cellulose 22(1):749–761
Fogh K, Andersen MB, Bischoff-Mikkelsen M, Bause R, Zutt M, Schilling S, Schmutz J-L, Borbujo J, Jimenez JA, Cartier H, Jørgensen B (2012) Clinically relevant pain relief with an ibuprofen-releasing foam dressing: results from a randomized, controlled, double-blind clinical trial in exuding, painful venous leg ulcers. Wound Repair Regen 20(6):815–821
Steffansen B, Herping SPK (2008) Novel wound models for characterizing ibuprofen release from foam dressings. Int J Pharmaceut 364(1):150–155
Vinklarkova L, Masteikova R, Vetchy D, Dolezel P, Bernatoniene J (2015) Formulation of novel layered sodium carboxymethylcellulose film wound dressings with ibuprofen for alleviating wound pain. BioMed Res Int 2015:892671
Hanci V, Hakimoglu S, Ozacmak H, Bektas S, Ozacmak HS, Ozdamar SO, Yurtlu S, Turan IO (2012) Comparison of the effects of bupivacaine, lidocaine, and tramadol infiltration on wound healing in rats. Revista brasileira de anestesiologia 62(6):799–810
Kumarswamy A, Moretti A, Paquette D, Padilla R, Everett E, Nares S (2012) In vivo assessment of osseous wound healing using a novel bone putty containing lidocaine in the surgical management of tooth extractions. Int J Dent 894:815
Elsner JJ, Zilberman M (2009) Antibiotic-eluting bioresorbable composite fibers for wound healing applications: microstructure, drug delivery and mechanical properties. Acta Biomater 5(8):2872–2883
Vowden K, Vowden P (2014) Wound dressings: principles and practice. Surgery 32(9):462–467
Mayet N, Choonara YE, Kumar P, Tomar LK, Tyagi C, Du Toit LC, Pillay V (2014) A comprehensive review of advanced biopolymeric wound healing systems. J Pharm Sci 103(8):2211–2230
Dornseifer U, Lonic D, Gerstung TI, Herter F, Fichter AM, Holm C, Schuster T, Ninkovic M (2011) The ideal split-thickness skin graft donor-site dressing: a clinical comparative trial of a modified polyurethane dressing and aquacel. Plast Reconstr Surg 128(4):918–924
Ryssel H, Germann G, Riedel K, Reichenberger M, Hellmich S, Kloeters O (2010) Suprathel-acetic acid matrix versus acticoat and aquacel as an antiseptic dressing: an in vitro study. Ann Plast Surg 65(4):391–395
Tickle J (2012) Effective management of exudate with AQUACEL extra. Brit J Commu Nursing Suppl S38:S36–40
Manizate F, Fuller A, Gendics C, Lantis JC 2nd (2012) A prospective, single-center, nonblinded, comparative, postmarket clinical evaluation of a bovine-derived collagen with ionic silver dressing versus a carboxymethylcellulose and ionic silver dressing for the reduction of bioburden in variable-etiology, bilateral lower-extremity wounds. Adv Skin Wound Care 25(5):220–225
Lee JH, Lim SJ, Oh DH, Ku SK, Li DX, Yong CS, Choi HG (2010) Wound healing evaluation of sodium fucidate-loaded polyvinylalcohol/sodium carboxymethylcellulose-based wound dressing. Arch Pharmacal Res 33(7):1083–1089
Broumand A, Emam-Djomeh Z, Khodaiyan F, Davoodi D, Mirzakhanlouei S (2014) Optimal fabrication of nanofiber membranes from ionized-bicomponent cellulose/polyethyleneoxide solutions. Int J Biol Macromol 66:221–228
Rice JB, Desai U, Cummings AKG, Birnbaum HG, Skornicki M, Parsons NB (2014) Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care 37:651–658
Charras G, Sahai E (2014) Physical influences of the extracellular environment on cell migration. Nat Rev Mol Cell Biol 15(12):813–824
Wimpenny I, Markides H, El Haj AJ (2012) Orthopaedic applications of nanoparticle-based stem cell therapies. Stem Cell Res Ther 3(2):13
Maver T, Maver U, Mostegel F, Grieser T, Spirk S, Smrke D, Stana Kleinschek K (2015) Cellulose based thin films as a platform for drug release studies to mimick wound dressing materials. Cellulose 22:749–761
Maver U, Bele M, Jamnik J, Gaberšček M, Planinšek O (2013) A fast and simple method for preparation of calcium carbonate-drug composites for fast drug release. Mater Res Bull 48(1):137–145
Žužek Rožman K, Pečko D, Šturm S, Maver U, Nadrah P, Bele M, Kobe S (2012) Electrochemical synthesis and characterization of Fe 70Pd 30 nanotubes for drug-delivery applications. Mater Chem Phys 133(1):218–224
Lao LL, Peppas NA, Boey FYC, Venkatraman SS (2011) Modeling of drug release from bulk-degrading polymers. Int J Pharmaceut 418(1):28–41
Kanjickal DG, Lopina ST (2004) Modeling of drug release from polymeric delivery systems—a review. Crit Rev Ther Drug 21(5):345–386
Costa P, Manuel J, Lobo S (2001) Modeling and comparison of dissolution profiles. Eur J Pharm Sci 13(2):123–133
Haith LR, Stair-Buchmann ME, Ackerman BH, Herder D, Reigart CL, Stoering M, Guilday RE, Patton ML, Ross KM (2014) Evaluation of aquacel Ag for autogenous skin donor sites. J Burn Care Res. doi:10.1097/BCR.0000000000000212
Glavan N, Bosak A, Glavan-Gacanin L, Jonjic N (2015) Efficacy of aquacel Ag dressing in the treatment of deep burns in children. Burns 41(1):199–202
Barnea Y, Weiss J, Gur E (2010) A review of the applications of the hydrofiber dressing with silver (Aquacel Ag) in wound care. Ther Clin Risk Manag 6:21–27
Harding K, Gottrup F, Jawien A, Mikosinski J, Twardowska-Saucha K, Kaczmarek S, Sopata M, Shearman C, Pieronne A, Kommala D (2012) A prospective, multi-centre, randomised, open label, parallel, comparative study to evaluate effects of AQUACEL(R) Ag and Urgotul(R) Silver dressing on healing of chronic venous leg ulcers. Int Wound J 9(3):285–294
Nawalakhe R, Shi Q, Vitchuli N, Noar J, Caldwell JM, Breidt F, Bourham MA, Zhang X, McCord MG (2013) Novel atmospheric plasma enhanced chitosan nanofiber/gauze composite wound dressings. J Appl Polym Sci 129(2):916–923
Zahedi P, Rezaeian I, Ranaei-Siadat S-O, Jafari S-H, Supaphol P (2010) A review on wound dressings with an emphasis on electrospun nanofibrous polymeric bandages. Polym Advan Technol 21(2):77–95
Maver T, Hribernik S, Mohan T, Smrke DM, Maver U, Stana-Kleinschek K (2015) Functional wound dressing materials with highly tunable drug release properties. RSC Advances 5(95):77873–77884
Acknowledgments
The authors acknowledge the financial support from the Ministry of Higher Education, Science and Technology of the Republic of Slovenia, as well as the financial contributions from the WoodWisdom-NET+ funded project AEROWOOD with the Grant Number 3330-14-500041 and mnt-era.net funded project WoundSens with the Grant Number 3211-12-00002.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maver, T., Kurečič, M., Smrke, D.M. et al. Electrospun nanofibrous CMC/PEO as a part of an effective pain-relieving wound dressing. J Sol-Gel Sci Technol 79, 475–486 (2016). https://doi.org/10.1007/s10971-015-3888-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10971-015-3888-9