Abstract
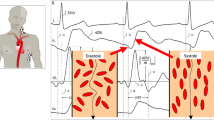
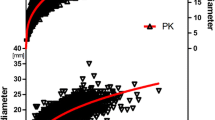
Electrical cardiometry (EC) is a non-invasive and inexpensive method for hemodynamic assessment and monitoring. However, its feasibility for widespread clinical use, especially for the obese population, has yet to be determined. In this study, we evaluated the agreement and reliability of EC compared to transthoracic Doppler echocardiography (TTE) in normal, overweight, and obese children and adolescents. We measured stroke volume (SV) and cardiac output (CO) of 131 participants using EC and TTE simultaneously. We further divided these participants according to BMI percentiles for subanalyses: <85% normal weight (n = 41), between 85 and 95% overweight (n = 7), and >95% obese (n = 83). Due to small sample size of the overweight group, we combined overweight and obese groups (OW+OB) with no significant change in results (SV and CO) before and after combining groups. There were strong correlations between EC and TTE measurements of SV (r = 0.869 and r = 0.846; p < 0.0001) and CO (r = 0.831 and r = 0.815; p < 0.0001) in normal and OW+OB groups, respectively. Bias and percentage error for CO measurements were 0.240 and 29.7%, and 0.042 and 29.5% in the normal and OW+OB groups, respectively. Indexed values for SV were lower in the OW+OB group than in the normal weight group when measured by EC (p < 0.0001) but no differences were seen when measured by TTE (p = 0.096). In all weight groups, there were strong correlations and good agreement between EC and TTE. However, EC may underestimate hemodynamic measurements in obese participants due to fat tissue.




Similar content being viewed by others
References
Liebman F, Pearl J, Bagno S. The electrical conductance properties of blood in motion. Phys Med Biol. 1962;7(2):177.
Liebman F, Bagno S. The behavior of the red blood cells in flowing blood which accounts for conductivity changes. Biomed Sci Instrum. 1968;4:25.
Sakamoto K, Kanai H. Electrical characteristics of flowing blood. IEEE Trans on Biomed Eng. 1979;26(12):686–95.
Visser IKR. Electric properties of flowing blood and impedance cardiography. Ann Biomed Eng. 1989;17(5):463–73.
Fujii M, Nakajima K, Sakamoto K, Kanai H. Orientation and deformation of erythrocytes in flowing blood. Ann N Y Acad Sci. 1999;873(1):245–61.
Hoetink A, Faes TJ, Visser K, Heethaar RM. On the flow dependency of the electrical conductivity of blood. IEEE transactions on Biomedical Engineering. 2004;51(7):1251–61.
Gaw RL, Cornish BH, Thomas BJ (2007) The electrical impedance of pulsatile blood flowing through rigid tubes: an experimental investigation. In: Scharfetter H, Merwa R (eds) 13th International Conference on Electrical Bioimpedance and the 8th Conference on Electrical Impedance Tomography: ICEBI 2007, August 29th - September 2nd 2007, Graz, Austria. Springer, Berlin, pp 73–6. doi:10.1007/978-3-540-73841-1_22.
Gaw RL, Cornish BH, Thomas BJ. The electrical impedance of pulsatile blood flowing through rigid tubes: a theoretical investigation. IEEE Trans Biomed Eng. 2008;55(2):721–7.
Bernstein DP. Impedance cardiography: Pulsatile blood flow and the biophysical and electrodynamic basis for the stroke volume equations. J Electr Bioimpedance. 2010;1(1):2–17.
Thiele RH, Bartels K, Gan TJ. Cardiac output monitoring: a contemporary assessment and review. Crit Care Med. 2015;43(1):177–85.
Staelens A, Tomsin K, Grieten L, Oben J, Mesens T, Spaanderman M, Jacquemyn Y, Gyselaers W. Non-invasive assessment of gestational hemodynamics: benefits and limitations of impedance cardiography versus other techniques. Expert Rev Med Devices. 2013;10(6):765–79.
Siedlecka J, Siedlecki P, Bortkiewicz A. Impedance cardiography-old method, new opportunities. Part I. Clinical applications. Int J Occup Med Environ Health. 2015;28(1):27–33.
Brown CV, Martin MJ, Shoemaker WC, Wo CC, Chan L, Azarow K, Demetriades D. The effect of obesity on bioimpedance cardiac index. Am J Surg. 2005;189(5):547–51.
Rauch R, Welisch E, Lansdell N, Burrill E, Jones J, Robinson T, Bock D, Clarson C, Filler G, Norozi K. Non-invasive measurement of cardiac output in obese children and adolescents: comparison of electrical cardiometry and transthoracic Doppler echocardiography. J Clin Monit Comput. 2013;27(2):187–93.
van der Meer B, de Vries JP, Schreuder W, Bulder E, Eysman L, de Vries PM. Impedance cardiography in cardiac surgery patients: abnormal body weight gives unreliable cardiac output measurements. Acta Anaesthesiol Scand. 1997;41(6):708–12.
Woltjer H, Bogaard H, Van der Spoel H, De Vries P. The influence of weight on stroke volume determination by means of impedance cardiography in cardiac surgery patients. Intensive Care Med. 1996;22(8):766–71.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL (2002) 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics Series 11, Data from the national health survey (246):1–190.
Norozi K, Beck C, Osthaus W, Wille I, Wessel A, Bertram H. Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth. 2008;100(1):88–94.
Bernstein D, Lemmens H. Stroke volume equation for impedance cardiography. Med Biol Eng Comput. 2005;43(4):443–50.
Mukaka M. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71.
Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–10.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15(2):85–91.
Chew MS, Poelaert J. Accuracy and repeatability of pediatric cardiac output measurement using Doppler: 20-year review of the literature. Intensive Care Med. 2003;29(11):1889–94.
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies–with specific reference to the measurement of cardiac output. Crit Care. 2009;13(1):1–6.
Du Bois D, Du Bois E. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5(5):303.
de Simone G, Devereux RB, Daniels SR, Mureddu G, Roman MJ, Kimball TR, Greco R, Witt S, Contaldo F. Stroke volume and cardiac output in normotensive children and adults assessment of relations with body size and impact of overweight. Circulation. 1997;95(7):1837–43.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–815.
Egan JR, Festa M, Cole AD, Nunn GR, Gillis J, Winlaw DS. Clinical assessment of cardiac performance in infants and children following cardiac surgery. Intensive Care Med. 2005;31(4):568–73.
Suehiro K, Joosten A, Murphy LS-L, Desebbe O, Alexander B, Kim S-H, Cannesson M. Accuracy and precision of minimally-invasive cardiac output monitoring in children: a systematic review and meta-analysis. J Clin Monit Comput. 2016;30(5):603–20.
Erlandsson K, Odenstedt H, Lundin S, Stenqvist O. Positive end-expiratory pressure optimization using electric impedance tomography in morbidly obese patients during laparoscopic gastric bypass surgery. Acta Anaesthesiol Scand. 2006;50(7):833–9.
Song R, Rich W, Kim J, Finer N, Katheria A. The use of electrical cardiometry for continuous cardiac output monitoring in preterm neonates: a validation study. Am J Perinatol. 2014;31(12):1105–10.
Absi MA, Lutterman J, Wetzel GT. Noninvasive cardiac output monitoring in the pediatric cardiac intensive care unit. Curr Opin Cardiol. 2010;25(2):77–9.
Blohm ME, Obrecht D, Hartwich J, Mueller GC, Kersten JF, Weil J, Singer D. Impedance cardiography (electrical velocimetry) and transthoracic echocardiography for non-invasive cardiac output monitoring in pediatric intensive care patients: a prospective single-center observational study. Crit Care. 2014;18(6):1–9.
Hapfelmeier A, Cecconi M, Saugel B. Cardiac output method comparison studies: the relation of the precision of agreement and the precision of method. J Clin Monit Comput. 2016;30(2):149–55.
Acknowledgements
We would like to thank Elizabeth Burrill (NP) and Jody Jones (RDMS) for their support recruiting patients and performing echocardiography; and Adam A. Dempsey for his assistance with manuscript revisions.
Funding
This study was partially supported by research grants from Western University (ADF-5609-8), Children’s Health Research Institute (LHRF 7712), Innovation Fund of the Alternative Funding Plan of the Academic Health Sciences Centres of Ontario (AMOSO, #INN 12-003) and grant from Children’s Health Foundation, London, Ontario to Dr. K. Norozi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Western University Health Science Research Ethics Board (REB # 16266E). All children and adolescents gave written consent to participate in this study. For those under 16 years of age, we obtained written consent from caregivers.
Rights and permissions
About this article
Cite this article
Altamirano-Diaz, L., Welisch, E., Rauch, R. et al. Does obesity affect the non-invasive measurement of cardiac output performed by electrical cardiometry in children and adolescents?. J Clin Monit Comput 32, 45–52 (2018). https://doi.org/10.1007/s10877-017-9994-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-017-9994-1