Abstract
Purpose
Thirty states now report one in three children between 10–17 years of age are either overweight or obese. This disturbing trend will have lasting implications for our children, specifically those known as the Millennial generation born between 1982 and 1993.
Approach
Utilizing evidence in the existing literature, we created an economic model to predict the impact of obesity on the aggregate lifetime earnings for the Millennial generation and the consequences for employers and employees. We provide case reports on successful business strategies that speak to the classic characteristics of the Millennials.
Findings
The lifetime medical expenditure that is attributable to obesity for an obese 20-year-old varies from $5,340 to $29,460, increasing proportionally with rising weight. If the model’s assumptions hold true, Millennial American women will earn an average of $956 billion less while men will earn an average of $43 billion less due to obesity.
Implications
As Millennials enter the workforce, the growing prevalence of obesity among their generation may negatively impact their productivity and resulting economic prosperity. Given that most of one’s adult life is spent on the job, employers have a unique opportunity to contribute to the solution by creating an environmental culture of health.
Originality/Value
This is the first assessment, which we know of, that examines the potential economic impact of obesity on the Millennial generation. We propose a unique approach applying a common health framework, the Chronic Care Model, to business strategies to contain costs and maximize Millennial workers’ health and productivity.
Similar content being viewed by others
Scope of the Problem of Obesity
Over the past three decades, obesity has risen dramatically, resulting in two-thirds of adults in the United States being obese. The state of morbid obesity is increasing even faster than overall obesity rates. This is especially true in children (Pietrobelli and Heymsfield 2002). Between 1976 and 1980, the overweight rate for children between 6 and 17 years old was 5.7%. Twenty-five years later, that rate has tripled: between 2005 and 2006 the obesity rate was 17.2% for boys and 15.9% for girls (Center for Disease Control and Prevention 2009). In fact, in some states the prevalence of obesity in childhood has increased to 31.8% for boys and 30.8% for girls (Hedley et al. 2004).
While the consequences of obesity may not be readily apparent until adulthood, obesity and its complications actually begin in childhood. The scientific evidence has existed for a long time, demonstrating that dyslipidemia such as high cholesterol leads to atherosclerosis, a deposition of fatty streaks in the arteries, and that this begins in childhood and contributes considerably to later adult cardiovascular disease (McGill 1963; McGill et al. 2008). Moreover, rapid infant weight gain often leads to excessive weight gain by age four and is linked to adult obesity and the most commonly thought of health consequences such as heart disease, high blood pressure, and diabetes (Dennison et al. 2006; Leunissen et al. 2009). In fact, without aggressive intervention, the Centers for Disease Control and Prevention estimates that one in three children will go onto have diabetes (Olshansky et al. 2005). But obesity also confers increased risk for many other medical problems, including uterine cancer, cervical cancer and breast cancer in women, and premature testosterone decline, liver cancer and pancreatic cancer in men (Brown et al. 2009). Moreover, these predictions are not unique to the United States, they are consistent with patterns of rising obesity seen in developing countries that have adopted “Western” lifestyles with lower levels of physical activity and increased consumption of processed, nutrient-poor food (Hossain et al. 2007). For example, the World Health Organization predicts that by 2030, India will be home to 80 million diabetics (Wild et al. 2004).
Despite awareness of the current trends, the epidemic continues. A 2009 report from the Robert Wood Johnson Foundation (RWJF) found that no U.S. state had met the 2010 goal of reducing adult obesity rates to 15%. In fact, only 19 states have obesity rates less than 25% (Levi and Trust for America’s Health 2009). Thirty states report one in three children between 10 and 17 years of age is either overweight or obese. Mississippi leads the way with almost 45% of its children meeting criteria for being overweight or obese, though many other states are not far behind. This disturbing trend will have lasting implications for children, specifically those known as the Millennial generation.
Who are the Millennials and What is their Risk Profile?
The children of the Millennial generation are the children of the Baby Boomers and the successors of Generation X. In the 1990s, they loved teen pop music and after the turn of the century they brought to life social networking websites like My Space and Facebook. They are generally characterized by optimism and activity. They demand constant access to communication technologies and value flexibility, creativity, independence, and making an impact in the workplace (Howe and Strauss 2000). They are also the victims of the childhood obesity epidemic.
The Millennial generation has poor health habits, including inactivity and poor nutrition, which contribute to the early development of overweight and obesity. A 2008 U.S. national survey of health behavior among high school students showed that two-thirds of students did not meet recommended guidelines for physical activity (U.S. Department of Health and Human Services Centers for Disease Control and Prevention 2008). Instead of physical activity, nearly one quarter spent three or more hours per day playing computer or video games, and over one-third reported watching three or more hours of television (U.S. Department of Health and Human Services Centers for Disease Control and Prevention 2008) per day. The same survey showed similarly discouraging results when youth were asked about their dietary habits. Over 75% of students did not eat the recommended amount of fruits and vegetables. (U.S. Department of Health and Human Services Centers for Disease Control and Prevention 2008). Conversely, over one-third consumed at least one can or bottle of soda per day (U.S. Department of Health and Human Services Centers for Disease Control and Prevention 2008).
Obesity as a Public Health Problem
Being overweight or obese in childhood is associated with low self-esteem, high levels of cholesterol, and high blood pressure. Obesity in children can also be associated with type 2 diabetes (T2DM), liver and gall bladder problems, sleep apnea, orthopedic problems, and depression (Institute of Medicine 2004). In fact, without aggressive intervention, over 30% of children born in the year 2000 will go onto have T2DM and at least 10% of those will develop renal complications, including renal failure. Recognizing that these health complications represent illnesses that tend to be chronic in nature, these problems will plague the Millennial generation for years to come unless dramatic and widespread changes in lifestyle are made soon.
Obesity as an Economic Problem
Obesity-related health burdens carry staggering financial ramifications. The lifetime medical expenditure for an obese 20 year old ranges from $5,340 to $29,460, increasing proportionally with a rising Body Mass Index (BMI) (Finkelstein et al. 2008). The United States as a whole spent $78.5 billion in 2003 on health issues directly related to obesity, accounting for almost 10% of the national healthcare budget. About half of these costs were financed by Medicare/Medicaid, and many more by employer-supported insurance.
In addition to burgeoning obesity-related health care costs, the obesity epidemic directly impacts the nation’s workforce, resulting in decreased productivity and increased organizational expenditures on healthcare. With the childhood obesity epidemic on the rise and with the Millennial generation about to comprise the majority of the workforce, the nation’s economy will soon be faced with an overwhelming economic problem.
What Does this Mean for Millennial Employees?
As Millennials move into the workforce, there is reason to be concerned that changes in their lifestyle and the growing prevalence of obesity among their generation may negatively impact their productivity and their resulting economic prosperity. Indeed, studies have found that obesity is associated with negative labor market outcomes. For example, obese individuals persistently miss more work days and earn lower wages than their non-obese counterparts (Baum and Ford 2004; Finkelstein et al. 2005). Given the risk of obesity for today’s youth, what impact will obesity have on the wages of tomorrow’s workforce?
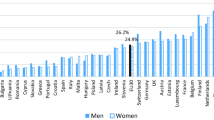
Recent studies provide evidence that obesity causes lower wages. Estimates of this wage penalty range from 12% for women and 0.7% for men, to no perceivable penalty for either (Averett and Korenman 1996; Baum and Ford 2004; Behrman and Rosenzweig 2001; Cawley 2004; Norton and Han 2008). Of the five cited studies, three find evidence of a wage penalty. Of those studies, the wage penalty was consistently higher for women than men, despite the increased prevalence of obesity in men (25.4%) compared to women (21.8%) (MMWR 2009).
The causal effect of obesity on wages is often attributed to several possible factors, although these factors have not yet been conclusively proven. For example, it has been noted that obesity may limit the amount or kind of work employees can perform due to health problems. It is also possible that employers simply discriminate against obese workers by compensating them less than non-obese workers, or that employers that provide health insurance pass the incremental health care costs associated with obesity to obese workers in the form of lower wages (Baum and Ford 2004; Bhattacharya and Bundorf 2005).
Utilizing evidence in the existing literature, we created an economic model to predict the impact of obesity on the aggregate lifetime earnings for the Millennial generation. This approach offers the ability to examine the earnings amount that the Millennial generation should expect to lose due to obesity-related health consequences. To obtain this estimate, average wages reported in 2007 dollars from the Current Population Survey were used and supplemented with labor force projections from the Bureau of Labor Statistics and Toossi’s published study (Bureau of Labor Statistics 2007a, b; Current Population Survey 2007; Toossi 2006). Estimated wage penalties were calculated utilizing previous literature that indicates a 67% adult obesity rate, and assumes that Millennials will participate in the workforce during the ages of 20–65.
In Table 1, aggregate lifetime loss in wages due to obesity for Millennial men and women are reported. These estimates are calculated using the mean of the wage penalties from the previous literature (0.14% wage penalty for men and 4.84% wage penalty for women). Upper and lower bound estimates are presented below the mean estimates in brackets. Upper bound estimates are calculated using the highest wage penalty from the previous literature (0.7% wage penalty for men and 11.9% wage penalty for women) and lower bound estimates are simply $0 for men and women since the lowest wage penalty reported in the literature is 0% (i.e., no wage penalty) for both genders.
From the results in Table 1, it is clear that obesity has a much larger potential impact on the aggregate lifetime earnings of Millennial women than men. This is true even accounting for the fact that labor force participation rates for women are lower and women earn less than men. If the assumptions for this model hold true, Millennial U.S. women will earn an average of $956 billion less due to obesity, whereas Millennial men will earn an average of $43 billion less. The overall impact of obesity on the aggregate lifetime earnings of Millennial men and women is close to one trillion dollars. In other words, Millennial men and women, potentially, will earn $998 billion less due to obesity. The reduced income and the accompanying decrease in productivity affect not only the Millennials but also create a complex problem for their employers.
What Does this Mean for Millennial Employers?
Employers are starting to recognize the magnitude of the economic burden of obesity and the role that they must play as the primary providers of health insurance. In a survey of 489 employers with 7.8 million employees, the average annual healthcare expenditure in 2008 was $56 billion, which represents $7,173 per employee per year (Wyatt 2009). In an attempt to minimize these costs, some employers are shifting their focus from treatment of illness to prevention of disease. They understand that their approach must be comprehensive, tailored to the employee population and done with the support of top management (Okie 2007). In fact, two-thirds of employers cite the poor health habits of their employees as the biggest challenge to managing healthcare costs, and 91% of employers believed that they could reduce healthcare costs by influencing employees to adopt healthier lifestyles (Harris Interactive 2007). As a result, more companies are starting wellness programs as they seek to reduce their annual healthcare expenditure: in 2006, 19% of employers with more than 500 employees had wellness programs versus 7% in 2004 (Mercer Human Resource Consulting 2007).
The Workplace Environment Can Maximize Health and Decrease Obesity
As the main constituent of the rising workforce, the 16–27-year-olds of the Millennial generation find themselves at the center of these increased efforts to reverse the obesity epidemic. If the average American works from age 20 to 65, with a 40 h a week occupation, over the span of her work-life she will spend 90,000 h of her life at work. In order to reverse the trend toward obesity and minimize its economic burden, employers cannot rely on programs that were effective for a previous generation of employees. Instead, employers must develop creative and effective wellness programs that cater to, and take advantage of, the mix of optimism and activity that characterizes the Millennial generation (Howe and Strauss 2000). Namely, this group of 75 million Americans is self-inventive, they utilize the Internet and the latest technology, and they embrace diversity of people and ideas (Lancelotta 2008).
In a survey of 489 major companies, Watson Wyatt Worldwide took a close look at companies that were successful at limiting their healthcare costs. The survey separated top performing companies from poor performing companies based on their 5-year healthcare expenditures. Top performing companies had a 10% healthcare expenditure reduction, or twenty-three million dollars saved over 5 years (Wyatt 2009). The empirical analysis of survey data found wellness programs that were successful in limiting costs included appropriate financial incentives, effective information delivery, and the provision of high quality care. Specifically, 34% of top performing companies had incentives to encourage participation in a weight loss program. These companies were twice as likely to have higher levels of participation. Top performing companies were more likely to: (1) have consumer directed health plans when compared with poor performing companies (17% vs. 7%); (2) motivate employees to manage their lifestyle risks and health conditions (45% vs. 40%); and (3) have a higher percentage of employees who participated in disease management programs with biometric screening (36% vs. 24%). Moreover, 55% of top performing companies had senior leadership visibly supporting the importance of a healthy work environment, compared with 37% of poor performing companies.
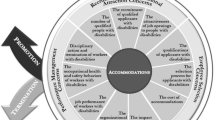
Applying the Chronic Care Model of Disease to Maximize Employee Health
The strategies of companies that are successful at reducing healthcare costs parallel a common conceptual framework applied to addressing chronic illness in the healthcare setting, the chronic care model of disease. This model highlights six key components that can systemically improve the health of patients with chronic conditions such as diabetes or obesity: (1) self-managed support; (2) decision support; (3) effective delivery of healthcare; (4) community resource utilization; (5) clinical information resource utilization; and (6) healthcare organizational structure (Fig. 1, Wagner et al. 2001)
In Table 2, each chronic care component is paired with business strategies that have been employed with success. Additionally, each of these strategic components is then associated with Millennial generation characteristics, highlighting how this generation might respond to different workplace strategies to improve health and wellness, and subsequent productivity. For example, recognizing the importance of technology to the Millennial generation, wellness programs have created interactive online health questionnaires, risk assessments, and educational modules to promote healthy eating and exercise among their employees, providing employees with information on how to improve their own health. This approach utilizes multiple chronic care components including self-managed support, decision support, and clinical information resource utilization. While this model addresses the system of health care delivery, it provides insights into how these components can be applied in the context of a business organization. In an evaluation of the chronic care model of disease, Wagner et al. found that lack of leadership support was a primary predictor of treatment failure. In order for business wellness programs to be effective, the company leadership must lead by example and facilitate a culture change to facilitate improved healthy behaviors. Based on the Watson and Wyatt report, it is clear that companies that conform to a chronic care model of wellness are able to effectively impact the wellness of their employees—to the tune of $21 million per year in healthcare savings (Wyatt 2009).
Brief Case Reports
Combating obesity in the workplace will require the commitment of companies to partner with their employees over time. IBM, GM, and Medtronic have each created unique approaches to reducing obesity by tailoring their wellness programs to the characteristics of their employees. Below, each case report highlights some successful strategies that integrate components of the chronic care model (noted in italics) and appeal to the classic Millennial generation.
Case Report One
IBM prides itself in creating strong trusting relationships with its employees and in creating an environment that is conducive to healthy living. For example, IBM’s campuses are walkable, they have healthy choices in the cafeterias and 75% of employees have completed an incentive program that focuses on exercise and nutrition (Wyatt 2009). IBM’s approach demonstrates the effectiveness of self-managed support by empowering employees to recognize their central role in their own wellness through the completion of training modules on exercise and nutrition.
Case Report Two
General Mills (GM) instituted a health risk questionnaire, weight loss campaigns, and competitions and provided free access to nutritionists. They have ballroom dancing and yoga classes on campus, and running races and dodgeball tournaments. As a result of these programs, 188 people lost an average of 6.4% of their beginning weight, and the company is starting to see a decrease in insurance claims related to heart disease (Wyatt 2009). This approach recognizes the importance of flexibility and creativity, allowing weight loss to happen in a team environment. It provides a unique way of looking at effective delivery of healthcare. Companies using creative approaches to wellness make their employees more likely to participate and more likely to achieve lasting results.
Case Report Three
Medtronic has made a major shift in its healthcare investment, shifting from a focus on treatment to a focus on health. They have developed onsite wellness seminars. Their cafeteria has reduced prices on healthy choices. Employees receive $100 if they work with a health coach for individualized improvements. This resulted in 92% of their employees completing health risk questionnaires, 78% decreasing their cholesterol levels and a collective weight loss for their company of 12 tons! Additionally, they avoided $1.4 million in healthcare costs as a result of testing their exercise capacity. One highlight of Medtronic’s approach is a high percentage of health risk questionnaires completed. This is an example of combining the appeal of technology with the importance of Clinical Information System Utilization to combat obesity.
By examining the characteristics of effective wellness programs, it becomes clear that using the chronic care model of disease as a framework can provide insights into potentially successful business strategies to improve employee health for a robust workforce. Whether encouraging self-managed support through wellness seminars or using effective information delivery with online training modules, companies that combine the chronic care model of disease components with the unique aspects of the Millennial generation has proven successful.
Conclusion
The burden of obesity represents a critical public health and economic health crisis that will impact the Millennial generation as they enter the workforce. Both in terms of work productivity and health care burden, obesity threatens this generation like no generation before. Given that most of one’s adult life is spent on the job, employers have a unique opportunity to contribute to the solution by creating an environmental culture of health. The time to act is now.
References
Averett, S., & Korenman, S. (1996). The economic reality of the beauty myth. Journal of Human Resources, 31(2), 304–330.
Baum, C. L., 2nd, & Ford, W. F. (2004). The wage effects of obesity: A longitudinal study. Health Economics, 13(9), 885–899.
Behrman, J. R., & Rosenzweig, M. R. (2001). The returns to increasing body weight. Retrieved August 4, 2009, from http://ssrn.com/abstract=297919.
Bhattacharya, J., & Bundorf, K. (2005). The incidence of the healthcare costs of obesity. http://www.nber.org/papers/w11303.pdf?new_window=1.
Brown, W. V., Fujioka, K., Wilson, P. W., & Woodworth, K. A. (2009). Obesity: Why be concerned? American Journal of Medicine, 122(4 Suppl 1), S4–11.
Bureau of Labor Statistics (2007a). Employment projections. Civilian labor force participation rates by sex, age, race and hispanic origin. Retrieved July 16, 2009, from http://www.bls.gov/emp/emplab05.htm.
Bureau of Labor Statistics. (2007b). Employment projections. civilian noninstitutional population by sex, age, race and hispanic origin. Retrieved July 16, 2009, from http://www.bls.gov/emp/emplab02.htm.
Cawley, J. (2004). The impact of obesity on wages. Journal of Human Resources, 39(2), 451–474.
Center for Disease Control and Prevention. (2009). Overweight children ages 6–17: Increased from 6% in 1976–1980 to 17% in 2005–2006. Retrieved September 30, 2009, from http://www.cdc.gov/Features/dsOverweightchildren/.
Current Population Survey. (2007). Annual social and economic supplement 2007. Retrieved July 16, 2009, from http://www.census.gov/hhes/www/macro/032008/perinc/new08_000.htm.
Dennison, B. A., Edmunds, L. S., Stratton, H. H., & Pruzek, R. M. (2006). Rapid infant weight gain predicts childhood overweight. Obesity, 14(3), 491–499.
Finkelstein, E., Fiebelkorn, C., & Wang, G. (2005). The costs of obesity among full-time employees. American Journal of Health Promotion, 20(1), 45–51.
Finkelstein, E. A., Trogdon, J. G., Brown, D. S., Allaire, B. T., Dellea, P. S., & Kamal-Bahl, S. J. (2008). The lifetime medical cost burden of overweight and obesity: Implications for obesity prevention. Obesity, 16(8), 1843–1848.
Harris Interactive. (2007). Strategic health perspectives data sheet questionnaires. New York.
Hedley, A. A., Ogden, C. L., Johnson, C. L., Carroll, M. D., Curtin, L. R., & Flegal, K. M. (2004). Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA, 291(23), 2847–2850.
Hossain, P., Kawar, B., & El Nahas, M. (2007). Obesity and diabetes in the developing world—a growing challenge. New England Journal of Medicine, 356(3), 213–215.
Howe, N., & Strauss, W. (2000). Millennials rising: The next great generation. New York: Vintage Books.
Institute of Medicine. (2004). Childhood obesity in the United States: Facts and figures. Retrieved August 4, 2009, from http://www.iom.edu/Object.File/Master/22/606/FINALfactsandfigures2.pdf.
Lancelotta, R. (2008). Millennials: The new generation of individuals born between 1977–1998. Retrieved June 1, 2009, from http://www.associatedcontent.com/article/704463/millennials_the_new_generation_of_individuals.html?cat=9.
Leunissen, R. W., Kerkhof, G. F., Stijnen, T., & Hokken-Koelega, A. (2009). Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA, 301(21), 2234–2242.
Levi, J., & Trust for America’s Health. (2009). F as in Fat: How obesity policies are failing in America, 2009. Robert Wood Johnson Foundation.
McGill, H. C., Jr. (1963). Natural history of human atherosclerotic lesions. In M. Sandler & G. Boune (Eds.), Atherosclerosis and its origin (pp. 39–65). New York: Academic Press.
McGill, H. C., Jr., McMahan, C. A., & Gidding, S. S. (2008). Preventing heart disease in the 21st century: Implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study. Circulation, 117(9), 1216–1227.
Mercer Human Resource Consulting. (2007). National Survey of Employer-Sponsored Health Plans: 2006 Survey Report. In. New York.
MMWR. (2009). Differences in prevalence of obesity among Black, White, and Hispanic Adults—United States, 2006–2008. Retrieved August 3, 2009, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5827a2.htm.
Norton, E. C., & Han, E. (2008). Genetic information, obesity, and labor market outcomes. Health Economics, 17(9), 1089–1104.
Okie, S. (2007). The employer as health coach. New England Journal of Medicine, 357(15), 1465–1469.
Olshansky, S. J., Passaro, D. J., Hershow, R. C., Layden, J., Carnes, B. A., Brody, J., et al. (2005). A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine, 352(11), 1138–1145.
Pietrobelli, A., & Heymsfield, S. B. (2002). Establishing body composition in obesity. Journal of Endocrinological Investigation, 25(10), 884–892.
Toossi, M. (2006). A new look at long-term labor force projections to 2050. Monthly Labor Review, 129(11), 19–39.
U.S. Department of Health and Human Services Centers for Disease Control and Prevention. (2008). 2007 National youth risk behavior survey overview. Retrieved August 4, 2009, from http://www.cdc.gov/HealthyYouth/yrbs/pdf/yrbs07_us_overview.pdf.
Wagner, E. H., Austin, B. T., Davis, C., Hindmarsh, M., Schaefer, J., & Bonomi, A. (2001). Improving chronic illness care: translating evidence into action. Health Affairs, 20(6), 64–78.
Wild, S., Roglic, G., Green, A., Sicree, R., & King, H. (2004). Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care, 27(5), 1047–1053.
Wyatt, W. (2009). The 14th annual national business group on health/watson wyatt employer survey on purchasing value in health care—The keys to continued success: lessons learned from consistent performers. Washington, DC.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Barkin, S.L., Heerman, W.J., Warren, M.D. et al. Millennials and the World of Work: The Impact of Obesity on Health and Productivity. J Bus Psychol 25, 239–245 (2010). https://doi.org/10.1007/s10869-010-9166-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10869-010-9166-5