Abstract
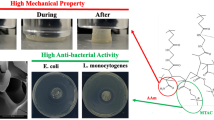
The aim of this work was to evaluate the release profile of vancomycin hydrochloride (VC), as well as the degradation, in vitro antistaphylococcal effect and cytotoxicity in MG-63 osteoblast-like cells of gelatin–starch (GS) films added with different concentrations of microparticles of the bioactive glass 45S5 (m-BG). The biomaterials were obtained through the gel-casting method. Four different composites were prepared at four different weight percentages of m-BG: 0, 5, 10, and 15 %. Glutaraldehyde 0.25 wt% (GA) was used as the cross-linker. The composites were characterized by scanning electron microscopy and the in vitro degradation of the films was studied by measuring the water uptake and weight loss. The drug release kinetics was quantified spectrophotometrically. The inhibition zone test and the plate count method were used to evaluate the antibacterial activity of the samples. Three staphylococcus strains were evaluated: Staphylococcus aureus ATCC6538, S. aureus ATCC29213, and Staphylococcus epidermidis ATCC12228. Cytotoxicity effects were evaluated through the MTT assay. The addition of m-BG to GS films showed no effects on the amount of water uptake, but led to an increase in the weight loss over time, even with m-BG content. The release rate of VC was also affected by the increasing concentration of m-BG in the composite films. However, the antibacterial effects of the composites were not improved by this modulation. All composites strongly inhibited staphylococcal cells with similar strength. On the other hand, liquid extracts from the composites resulted in cytotoxic effects on MG-63 osteoblast-like cells due to the presence of GA, but not to the concentration of VC or m-BG.





Similar content being viewed by others
References
Park K (2014) Controlled drug delivery systems: past forward and future back. J Control Release 190:3–8
Huang CL, Steele TWJ, Widjaja E, Boey FYC, Venkatraman SS, Loo JSC (2013) The influence of additives in modulating drug delivery and degradation of PLGA thin films. NPG Asia Mater 5:e54
Bowling FL, Jude EB, Boulton AJ (2009) MRSA and diabetic foot wounds: contaminating or infecting organisms? Curr Diabetes Rep 9:440–444
Bertesteanu S, Triaridis S, Stankovic M, Lazar V, Chifiriuc MC, Vlad M, Grigore R (2014) Polymicrobial wound infections: pathophysiology and current therapeutic approaches. Int J Pharm 463:119–126
Zafar N, Fessi H, Elaissari A (2014) Cyclodextrin containing biodegradable particles: from preparation to drug delivery applications. Int J Pharm 461:351–366
Ivanova P, Bazaka L, Crawford RJ (eds) (2014) New functional biomaterials for medicine and healthcare, Chapter 2. Woodhead Publishing, Oxford. ISBN 9781782422655
Chiono V, Pulieri E, Vozzi G, Ciardelli G, Ahluwalia A, Giusti P (2008) Genipin-crosslinked chitosan, gelatin blends for biomedical applications. J Mater Sci Mater Med 19:889–898
Santoro M, Tatara AM, Mikos AG (2014) Gelatin carriers for drug and cell delivery in tissue engineering. J Control Release 190:210–218
Gaowa A, Horibe T, Kohno M, Sato K, Harada H, Hiraoka M, Tabata Y, Kawakami K (2014) Combination of hybrid peptide with biodegradable gelatin hydrogel for controlled release and enhancement of anti-tumor activity in vivo. J Control Release 176:1–7
Foox M, Zilberman M (2015) Drug delivery from gelatin-based system. Expert Opin Drug Deliv 5:1–17
Patel ZS, Ueda H, Yamamoto M, Tabata Y, Mikos AG (2008) In vitro and in vivo release of vascular endothelial growth factor from gelatin microparticles and biodegradable composite scaffolds. Pharm Res 25:2370–2378
Young S, Wong M, Tabata Y, Mikos AG (2005) Gelatin as a delivery vehicle for the controlled release of bioactive molecules. J Control Release 109:256–274
Su Y, Mo X (2011) Genipin crosslinked gelatin nanofibers for tissue engineering. J Control Release 152(Suppl1):e230–e232
Amadori S, Torricelli P, Rubini K, Fini M, Panzavolta S, Bigi A (2015) Effect of sterilization and crosslinking on gelatin films. J Mater Sci Mater Med 26:69
Leng YG, Huang YQ, Dong CL, Huang MZ (2002) Research of grafting acrylamide on gelatin. Polym Mater Sci Eng 18:93–97
Shalumon KT, Deepthi S, Anupama MS, Nair SV, Jayakumar R, Chennazhi KP (2015) Fabrication of poly (l-lactic acid)/gelatin composite tubular scaffolds for vascular tissue engineering. Int J Biol Macromol 72:1048–1055
Xue J, Zhong Q (2014) Blending lecithin and gelatin improves the formation of thymol nanodispersions. J Agric Food Chem 62:2956–2962
Kowalczyk D, Kordowska-Wiater M, Nowak J, Baraniak B (2015) Characterization of films based on chitosan lactate and its blends with oxidized starch and gelatin. Int J Biol Macromol 77:350–359
Lu DR, Xiao CM, Xu SJ (2009) Starch-based completely biodegradable polymer materials. Express Polym Lett 6:366–375
Vieira AP, Ferreira P, Coelho JF, Gil MH (2008) Photocrosslinkable starch-based polymers for ophthalmologic drug delivery. Int J Biol Macromol 43:325–332
Chen L, Li X, Li L, Guo S (2007) Acetylated starch-based biodegradable materials with potential biomedical potential applications as drug delivery systems. Curr Appl Phys 7S1:e90–c93
Fakhouri FM, Costa D, Yamashita F, Martelli SM, Jesus RC, Alganer K, Collares-Queiroz FP, Innocentini-Mei LH (2013) Comparative study of processing methods for starch/gelatin films. Carbohydr Polym 95:681–689
Phromsopha T, Baimark Y (2014) Preparation of starch/gelatin blend microparticles by a water-in-oil emulsion method for controlled release. Drug Deliv Int J Biomater 2014:829490
Li W, Ding Y, Rai R, Roether JA, Schubert DW, Boccaccini AR (2014) Preparation and characterization of PHBV microsphere/45S5 bioactive glass composite scaffolds with vancomycin releasing function. Mater Sci Eng C Mater Biol Appl 41:320–328
Olalde B, Garmendia N, Sáez-Martínez V, Argarate N, Nooeaid P, Morin F, Boccaccini AR (2013) Multifunctional bioactive glass scaffolds coated with layers of poly(d, l-lactide-co-glycolide) and poly(n-isopropylacrylamide-co-acrylic acid) microgels loaded with vancomycin. Mater Sci Eng C Mater Biol Appl 33:3760–3767
Rivadeneira J, Di Virgilio AL, Audisio MC, Boccaccini AR, Gorustovich AA (2015) Evaluation of the antibacterial effects of vancomycin hydrochloride released from agar–gelatin–bioactive glass composites. Biomed Mater 10:015011
Cabanas MV, Pena J, Roman J, Vallet-Regi M (2009) Tailoring vancomycin release from beta-TCP/agarose scaffolds. Eur J Pharm Sci 37:249–256
Rezwan K, Chen QZ, Blaker JJ, Boccaccini AR (2006) Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 27:3413–3431
Hench LL (2009) Genetic design of bioactive glass. J Eur Ceram Soc 7:1257–1265
Rahman MN, Day DE, Bal BS, Fu Q, Jung SB, Bonewald LF, Tomsia AP (2011) Bioactive glass in tissue engineering. Acta Biomater 7:2355–2373
Miguez-Pacheco V, Hench LL, Boccaccini AR (2015) Bioactive glasses beyond bone and teeth: emerging applications in contact with soft tissues. Acta Biomater 13:1–15
Gorustovich AA, Roether JA, Boccaccini AR (2010) Effect of bioactive glasses on angiogenesis: a review of in vitro and in vivo evidences. Tissue Eng B 16:199–207
Day RM (2005) Bioactive glass stimulates the secretion of angiogenic growth factors and angiogenesis in vitro. Tissue Eng 11:768–777
Leach JK, Kaigler D, Wang Z, Krebsbach PH, Mooney DJ (2006) Coating of VEGF-releasing scaffolds with bioactive glass for angiogenesis and bone regeneration. Biomaterials 27:3249–3255
Yu H, Peng J, Xu Y, Chang J, Li H (2016) Bioglass activated skin tissue engineering constructs for wound healing. ACS Appl Mater Interfaces 8:703–715
Lin C, Mao C, Zhang J, Li Y, Chen X (2012) Healing effect of bioactive glass ointment on full-thickness skin wounds. Biomed Mater 7:045017
Bigi A, Cojazzi G, Panzavolta S, Rubini K, Roveri N (2001) Mechanical and thermal properties of gelatin films at different degrees of glutaraldehyde crosslinking. Biomaterials 2001(22):763–768
Gallant-Behm CL, Yin HQ, Liu S, Heggers JP, Langford RE, Olson ME, Hart DA, Burrell RE (2005) Comparison of in vitro disc diffusion and time kill-kinetic assays for the evaluation of antimicrobial wound dressing efficacy. Wound Repair Regen 13:412–421
Rivadeneira J, Di Virgilio AL, Audisio MC, Boccaccini AR, Gorustovich AA (2014) Evaluation of antibacterial and cytotoxic effects of nano-sized bioactive glass/collagen composites releasing tetracycline hydrochloride. J Appl Microbiol 116:1438–1446
Thakur G, Mitra A, Basak A, Sheet D (2012) Characterization and scanning electron microscopic investigation of crosslinked freeze dried gelatin matrices for study of drug diffusivity and release kinetics. Micron 43:311–320
Coimbra P, Gil MH, Figueiredo M (2014) Tailoring the properties of gelatin films for drug delivery applications: influence of the chemical cross-linking method. Int J Biol Macromol 70:10–19
Mota J, Yu N, Caridade SG, Luz GM, Gomes ME, Reis RL, Jansen JA, Walboomers XF, Mano JF (2012) Chitosan/bioactive glass nanoparticle composite membranes for periodontal regeneration. Acta Biomater 8:4173–4180
Maquet V, Boccaccini AR, Pravata L, Notingher I, Jérôme R (2003) Preparation, characterization, and in vitro degradation of bioresorbable and bioactive composites based on Bioglass filled polylactide foams. J Biomed Mater Res A 66A:335–346
Maquet V, Boccaccini AR, Pravata L, Notingher I, Jérôme R (2004) Porous poly(alphahydroxyacid)/bioglass composite scaffolds for bone tissue engineering: I. Preparation and in vitro characterization. Biomaterials 25:4185–4194
Misra SK, Mohn D, Brunner TJ, Stark WJ, Philip SE, Roy I, Salih V, Knowles JC, Boccaccini AR (2008) Comparison of nanoscale and microscale bioactive glass on the properties of P(3HB)/bioglass composites. Biomaterials 29:1750–1761
Grover CN, Cameron RE, Best SM (2012) Investigating the morphological, mechanical and degradation properties of scaffolds comprising collagen, gelatin and elastin for use in soft tissue engineering. J Mech Behav Biomed Mater 10:62–74
Misra SK, Ansari T, Mohn D, Valappil SP, Brunner TJ, Stark WJ, Roy I, Knowles JC, Sibbons PD, Jones EV, Boccaccini AR, Salih V (2010) Effect of nanoparticulate bioactive glass particles on bioactivity and cytocompatibility of poly(3-hydroxybutyrate) composites. J R Soc Interface 7:453–465
Larrañaga A, Aldazabal P, Martin FJ, Sarasua JR (2014) Hydrolytic degradation and bioactivity of lactide and caprolactone based sponge-like scaffolds loaded with bioactive glass particles. Polym Degrad Stab 110:121–128
Boccaccini AR, Maquet V (2003) Bioresorbable and bioactive polymer/bioglass composites with tailored pore structure for tissue engineering applications. Compos Sci Technol 63:2417e29
Blaker J, Nazhat SN, Maquet V, Boccaccini AR (2011) Long-term in vitro degradation of PDLLA/bioglass bone scaffolds in a cellular simulated body fluid. Acta Bio-mater 7:829e40
Yao Q, Nooeaid P, Roether JA, Dong Y, Zhang Q, Boccaccini AR (2013) Bioglass -based scaffolds incorporating polycaprolactone and chitosan coatings for controlled vancomycin delivery. Ceram Int 39:7517–7522
Mabrouk M, Mostafa AA, Oudadesse H, Mahmoud AA, El-Gohary MI (2014) Effect of ciprofloxacin incorporation in PVA and PVA bioactive glass composite scaffolds. Ceram Int 40:4833–4845
Das Gupta V, Stewart KR, Nohria S (1986) Stability of vancomycin hydrochloride in 5 % dextrose and 0.9 % sodium chloride, injections. Am J Hosp Pharm 43:1729–1731
Li H, Chang J (2005) In vitro degradation of porous degradable and bioactive PHBV/wollastonite composite scaffolds. Polym Degrad Stabil 87:301–307
Loher S, Reboul V, Brunner TJ, Simonet M, Dora C, Neuenschwander P, Stark WJ (2006) Improved degradation and bioactivity of amorphous aerosol derived tricalcium phosphate nanoparticles in poly(lactide-co-glycolide). Nanotechnology 17:2054–2061
Guo S, DiPietro LA (2010) Factors affecting wound healing. J Dent Res 89:219–229
Roh D-H, Kang S-Y, Kim J-Y, Kwon Y-B, Kweon HY, Lee K-G et al (2006) Wound healing effect of silk fibroin/alginate-blended sponge in full thickness skin defect of rat. J Mater Sci Mater Med 17:547–552
Vasconcelos A, Pêgo AP, Henriques L, Lamghari M, Cavaco-Paulo A (2010) Protein matrices for improved wound healing: elastase inhibition by a synthetic peptide model. Biomacromolecules 11:2213–2220
Reddy N, Reddy R, Jiang Q (2015) Crosslinking biopolymers for biomedical applications. Trends Biotechnol 33:362–369
Kouhi M, Morshed M, Varshosaz J, Fathi MH (2013) Poly(e-caprolactone) incorporated bioactive glass nanoparticles and simvastatin nanocomposite nanofibers: preparation, characterization and in vitro drug release for bone regeneration applications. Chem Eng J 228:1057–1065
Wang Q, Du YZ, Kennedy J (2007) Controlled release of ciprofloxacin hydrochloride from chitosan/polyethylene glycol blend films. Carbohydr Polym 69:336–343
Li W, Ding Y, Rai R, Roether JA, Schubert DW, Boccaccini AR (2014) Preparation and characterization of PHBV microsphere/45S5 bioactive glass composite scaffolds with vancomycin releasing function. Mater Sci Eng C 41:320–328
Allan I, Newman H, Wilson M (2001) Antibacterial activity of particulate bioglass against supra- and subgingival bacteria. Biomaterials 22:1683–1687
Waltimo T, Brunner TJ, Vollenweider M, Stark WJ, Zehnder M (2007) Antimicrobial effect of nanometric bioactive glass 45S5. J Dent Res 86:754–757
Hu S, Chang J, Liu M, Ning C (2009) Study on antibacterial effect of 45S5 bioglass. J Mater Sci Mater Med 20:81–86
Rivadeneira J, Audisio MC, Boccaccini AR, Gorustovich AA (2013) In vitro antistaphylococcal effects of a novel 45S5 bioglass/agar–gelatin biocomposite films. J Appl Microbiol 115:604–612
Dashti A, Ready D, Salih V, Knowles JC, Barralet JE, Wilson M, Donos N, Nazhat SN (2010) In vitro antibacterial efficacy of tetracycline hydrochloride adsorbed onto Bio-Oss bone graft. J Biomed Mater Res B Appl Biomater 93:394–400
Elsner JJ, Berdicevsky I, Zilberman M (2011) In vitro microbial inhibition and cellular response to novel biodegradable composite wound dressings with controlled release of antibiotics. Acta Biomater 7:325–336
Huang X, Brazel CS (2001) On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release 73:121–136
Robson MC, Mannari RJ, Smith PD, Payne WG (1999) Maintenance of wound bacterial balance. Am J Surg 178:399–402
Edwards R, Harding KG (2004) Bacteria and wound healing. Curr Opin Infect Dis 17:91–96
Umashankar PR, Mohanan PV, Kumari TV (2012) Glutaraldehyde treatment elicits toxic response compared to decellularization in bovine pericardium. Toxicol Int 1:51–58
Bigi A, Cojazzi G, Panzavolta S, Roveri N, Rubini K (2002) Stabilization of gelatin films by crosslinking with genipin. Biomaterials 23:4827–4832
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Rivadeneira, J., Di Virgilio, A.L., Audisio, M.C. et al. 45S5 Bioglass® concentrations modulate the release of vancomycin hydrochloride from gelatin–starch films: evaluation of antibacterial and cytotoxic effects. J Mater Sci 52, 9091–9102 (2017). https://doi.org/10.1007/s10853-016-0512-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-016-0512-5