Abstract
Purpose
To explore the attitudes of reproductive endocrinology and infertility (REI) and maternal–fetal medicine (MFM) subspecialists regarding the necessity and appropriateness of body mass index (BMI) cutoffs for women seeking fertility treatment.
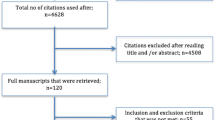
Methods
Members of the Society for Reproductive Endocrinology and Infertility (SREI) and the Society for Maternal Fetal Medicine (SMFM) were invited to participate in a survey querying their knowledge of existing institutional or clinic BMI policies and personal opinions regarding upper and lower BMI cutoffs for a range of fertility treatments, including oral ovulation agents, gonadotropins, and in vitro fertilization.
Results
Respondents included 398 MFMs and 201 REIs. The majority of REI and MFM providers agreed with upper limit BMI cutoffs (72.5% vs 68.2%, p = 0.29), but REIs were twice as likely to support lower limit BMI restrictions compared to MFMs (56.2% vs 28.4%, p < 0.0001). Those who supported upper BMI restrictions were more likely to be female and report existing institutional BMI cutoffs. The majority of respondents (99.3%) believed that an official statement to guide clinicians should be issued by a national professional organization.
Conclusions
Although practice patterns widely vary, the majority of REIs and MFMs believe that there should be a BMI cutoff above which women should not be offered immediate fertility treatment. Furthermore, there is a reported need for a written statement by a national professional organization to guide clinical practice and to ensure that OB/GYN subspecialists are providing consistent, fair, and safe recommendations to infertile women at the extremes of BMI.

Similar content being viewed by others
References
Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. Centers for Disease Control and Prevention (CDC). CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005-2013. MMWR Suppl. 2014;63:3–27.
Kent S, Fusco F, Gray A, Jebb SA, Cairns BJ, Mihaylova B. Body mass index and healthcare costs: a systematic literature review of individual participant data studies. Obes Rev. 2017;18:869–79.
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;1–8.
Persson M, Cnattingius S, Villamor E, Söderling J, Pasternak B, Stephansson O, et al. Risk of major congenital malformations in relation to maternal overweight and obesity severity: cohort study of 1.2 million singletons. BMJ. 2017;357:j2563.
Torloni MR, Betrán AP, Daher S, Widmer M, Dolan SM, Menon R, et al. Maternal BMI and preterm birth: a systematic review of the literature with meta-analysis. J Matern Fetal Neonatal Med. 2009;22:957–70.
American College of Obstetricians and Gynecologists. ACOG Committee opinion no. 549: obesity in pregnancy. Obstet Gynecol. 2013;121:213–7.
Scott-Pillai R, Spence D, Cardwell CR, Hunter A, Holmes VA. The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004-2011. BJOG. 2013;120:932–9.
Joy S, Istwan N, Rhea D, Desch C, Stanziano G. The impact of maternal obesity on the incidence of adverse pregnancy outcomes in high-risk term pregnancies. Am J Perinatol. 2009;26:345–9.
Lynch AM, Hart JE, Agwu OC, Fisher BM, West NA, Gibbs RS. Association of extremes of prepregnancy BMI with the clinical presentations of preterm birth. Am J Obstet Gynecol. 2014;210:428.e1–9.
Mahutte N, Kamga-Ngande C, Sharma A, Sylvestre C. Obesity and reproduction. J Obstet Gynaecol Can. 2018;40:950–66.
Brewer CJ, Balen AH. The adverse effects of obesity on conception and implantation. Reproduction. 2010;140:347–64.
Kominiarek MA, Jungheim ES, Hoeger KM, Rogers AM, Kahan S, Kim JJ. American Society for Metabolic and Bariatric Surgery position statement on the impact of obesity and obesity treatment on fertility and fertility therapy endorsed by the American College of Obstetricians and Gynecologists and the Obesity Society. Surg Obes Relat Dis. 2017;13:750–7.
Davies MJ. Evidence for effects of weight on reproduction in women. Reprod BioMed Online. 2006;12:552–61.
Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss. Fertil Steril. 2008;89:1603.
Provost MP, Acharya KS, Acharya CR, Yeh JS, Steward RG, Eaton JL, et al. Pregnancy outcomes decline with increasing body mass index: analysis of 239,127 fresh autologous in vitro fertilization cycles from the 2008-2010 Society for Assisted Reproductive Technology registry. Fertil Steril. 2016;105:663–9.
Kawwass JF, Kulkarni AD, Hipp HS, Crawford S, Kissin DM, Jamieson DJ. Extremities of body mass index and their association with pregnancy outcomes in women undergoing in vitro fertilization in the United States. Fertil Steril. 2016;106:1742–50.
Rittenberg V, Seshadri S, Sunkara SK, Sobaleva S, Oteng-Ntim E, El-Toukhy T. Effect of body mass index on IVF treatment outcome: an updated systematic review and meta-analysis. Reprod BioMed Online. 2011;23:421–39.
Sarais V, Pagliardini L, Rebonato G, Papaleo E, Candiani M, Viganò P. A comprehensive analysis of body mass index effect on in vitro fertilization outcomes. Nutrients. 2016;8:109.
MacKenna A, Schwarze JE, Crosby JA, Zegers-Hochschild F. Outcome of assisted reproductive technology in overweight and obese women. JBRA Assist Reprod. 2017;21:79–83.
Luke B, Brown MB, Missmer SA, Bukulmez O, Leach R, Stern JE, et al. The effect of increasing obesity on the response to and outcome of assisted reproductive technology: a national study. Fertil Steril. 2011;96:820–5.
Veleva Z, Tiitinen A, Vilska S, Hydén-Granskog C, Tomás C, Martikainen H, et al. High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod. 2008;23:878–84.
Dayan N, Spitzer K, Laskin CA. A focus on maternal health before assisted reproduction: results from a pilot survey of Canadian IVF medical directors. J Obstet Gynaecol Can. 2015;37:648–55.
Kaye L, Sueldo C, Engmann L, Nulsen J, Benadiva C. Survey assessing obesity policies for assisted reproductive technology in the United States. Fertil Steril. 2016;105:703–706.e2.
Zachariah M, Fleming R, Acharya U. Management of obese women in assisted conception units: a UK survey. Hum Fertil. 2006;9:101–5.
Practice Committee of American Society for Reproductive Medicine. Recommendations for reducing the risk of viral transmission during fertility treatment with the use of autologous gametes: a committee opinion. Fertil Steril. 2013;99:340–6.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–26.
Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7:130–8.
Ethics Committee of the American Society for Reproductive Medicine. Disparities in access to effective treatment for infertility in the United States: an Ethics Committee opinion. Fertil Steril. 2015;104:1104–10.
Quinn M, Fujimoto V. Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril. 2016;105:1119–23.
Mutsaerts MAQ, van Oers AM, Groen H, Burggraaff JM, Kuchenbecker WKH, Perquin DAM, et al. Randomized trial of a lifestyle program in obese infertile women. N Engl J Med. 2016;374:1942–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kelley, A.S., Badon, S.E., Lanham, M.S.M. et al. Body mass index restrictions in fertility treatment: a national survey of OB/GYN subspecialists. J Assist Reprod Genet 36, 1117–1125 (2019). https://doi.org/10.1007/s10815-019-01448-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01448-3