Abstract
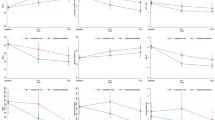
A persistent and significant barrier to the diagnosis and treatment of borderline personality disorder (BPD) in adolescents is clinician reluctance to label an adolescent with a stigmatized, intractable, treatment-resistant diagnosis. The goal of the current study was to evaluate this claim by examining the 18-month longitudinal course of borderline pathology in adolescents after discharge from inpatient treatment. 556 adolescent consecutive admissions (64.6% female; ages 12–17, M = 15.29, SD = 1.46) were assessed during admission to an inpatient treatment facility. They were followed up at discharge, 6 months, 12 months and 18 months after discharge with validated self-and parent report measures of adolescent BPD features. Latent growth modeling was used to evaluate outcomes. BPD features showed a significant decline over the follow-up period with very large effect sizes (> .80) for both parent and adolescent self-report. Rates of change were steeper for adolescent report although adolescent report fell below clinical cut-off 6 months later than parent-report. However, when internalizing and externalizing psychopathology were included in latent growth models, youth-reported BPD features did not show the same level of decline, while parent-reported BPD features maintained the same level of decline. The rate of decline between parents and adolescents was correlated, and baseline levels of BPD features were predictive of rate of change. This is the first study to show that adolescent borderline pathology follows a similar course after discharge from inpatient treatment previously demonstrated for adults. Like adult BPD, adolescent BPD appears to be not as intractable and treatment resistant as previously thought, mitigating against therapeutic nihilism.

Similar content being viewed by others
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms and profiles: An integrated system of multi-informant assessment. Burlington, VT: Research Center for Children, Youth, and Families.
Becker, B. J. (1988). Synthesizing standardized mean-change measures. British Journal of Mathematical & Statistical Psychology, 41, 257–278. https://doi.org/10.1111/j.2044-8317.1988.tb00901.x.
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246).
Biskin, R. S., Paris, J., Renaud, J., Raz, A., & Zelkowitz, P. (2011). Outcomes in women diagnosed with borderline personality disorder in adolescence. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 20(3), 168–174.
Chanen, A., Sharp, C., & Hoffman, P. (2017). Global Alliance for Prevention and Early Intervention for Borderline Personality Disorder. Prevention and early intervention for borderline personality disorder: a novel public health priority. World Psychiatry, 16(2), 215–216. https://doi.org/10.1002/wps.20429.
Chanen, A. M. (2015). Borderline personality disorder in young people: Are we there yet? Journal of Clinical Psychology, 71(8), 778–791. https://doi.org/10.1002/jclp.22205.
Chanen, A. M., Jackson, H. J., McCutcheon, L. K., Jovev, M., Dudgeon, P., Yuen, H. P., & McGorry, P. D. (2008). Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: randomised controlled trial. British Journal of Psychiatry, 193(6), 477–484. https://doi.org/10.1192/bjp.bp.107.048934.
Chanen, A. M., Jackson, H. J., McGorry, P. D., Allot, K. A., Clarkson, V., & Yuen, H. P. (2004). Two-year stability of personality disorder in older adolescent outpatients. Journal of Personality Disorders, 18(6), 526–541. https://doi.org/10.1521/pedi.18.6.526.54798.
Chanen, A. M., & McCutcheon, L. (2013). Prevention and early intervention for borderline personality disorder: current status and recent evidence. British Journal of Psychiatry. Supplement, 54, s24-29. https://doi.org/10.1192/bjp.bp.112.119180.
Chang, B., Sharp, C., & Ha, C. (2011). The criterion validity of the Borderline Personality Feature Scale for Children in an adolescent inpatient setting. Journal of Personality Disorders, 25(4), 492–503.
Clark, L. A., & Ro, E. (2014). Three-pronged assessment and diagnosis of personality disorder and its consequences: Personality functioning, pathological traits, and psychosocial disability. Journal of Personalitiy Disorders, 5(1), 55–69.
Clark, L. A., Nuzum, H., & Ro, E. (2017). Manifestations of personality impairment severity: comorbidity, course/prognosis, psychosocial dysfunction, and “borderline” personality features. Current Opinion in Psychology, 21, 117–121.
Collins, L. M., Schafer, J. L., & Kam, C. M. (2001). A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods, 6(4), 330–351.
Crick, N. R., Murray-Close, D., & Woods, K. (2005). Borderline personality features in childhood: a short-term longitudinal study. Development and Psychopathology, 17(4), 1051–1070.
De Los Reyes, A., & Ohannessian, C. M. (2016). Introduction to the Special Issue: Discrepancies in adolescent-parent perceptions of the family and adolescent adjustment. Journal of Youth and Adolescence, 45(10), 1957–1972. https://doi.org/10.1007/s10964-016-0533-z.
Department of Health & Human Services. (2005). The Victorian burden of disease study. Australia: Melbourne.
Dong, Y., & Peng, C. J. (2013). Principled missing data methods for researchers. SpringerPlus, 2(1), 1–17.
Enders, C. K. (2010). Applied missing data analysis. Guilford Press.
Fischer, E. H., Dornelas, E. A., & Goethe, J. W. (2001). Characteristics of people lost to attrition in psychiatric follow-up studies. Journal of Nervous and Mental Disease, 189(1), 49–55.
Garnet, K. E., Levy, K. N., Mattanah, J. J., Edell, W. S., & McGlashan, T. H. (1994). Borderline personality disorder in adolecents: ubiquitous or specific? American Journal of Psychiatry, 151(9), 1380–1382. https://doi.org/10.1176/ajp.151.9.1380.
Goodman, M., Patil, U., Triebwasser, J., Hoffman, P., Weinstein, Z. A., & New, A. (2011). Parental burden associated with borderline personality disorder in female offspring. Journal of Personality Disorders, 25(1), 59–74.
Griffiths, M. (2011). Validity, utility and acceptability of borderline personality disorder diagnosis in childhood and adolescence: survey of psychiatrists. The Psychiatric Bulletin, 35, 19–22.
Grilo, C. M., Becker, D. F., Edell, W. S., & McGlashan, T. H. (2001). Stability and change of DSM-III-R personality disorder dimensions in adolescents followed up 2 years after psychiatric hospitalization. Comprehensive Psychiatry, 42(5), 364–368. https://doi.org/10.1053/comp.2001.26274.
Gunderson, J. G., Shea, T., Skodol, A. E., & McGlashan, T. H. (2000). The collaborative longitudinal personality disorders study: Development, aims, design, and sample characteristics. Journal of Personality Disorders, 14(4), 300–316.
Gunderson, J. G., Stout, R. L., McGlashan, T. H., Shea, T., Morey, L. C., Grilo, C. M., ... & Skodol, A. E. (2011). Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders Study. Archives of General Psychiatry, 68(8), 827–837. https://doi.org/10.1001/archgenpsychiatry.2011.37.
Ha, C., Balderas, J., Zanarini, M., Oldham, J., & Sharp, C. (2014). Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. Journal of Clinical Psychiatry, 75(5), 457–464.
Hu, L.-T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
Jöreskog, K. G., & Sörbom, D. (1996). LISREL 8: User’s reference guide. Scientific Software International. Retrieved from https://books.google.com/books?hl=en&lr=&id=9AC-s50RjacC&oi=fnd&pg=PR1&dq=joreskog+sorbom+1996&ots=lV4BzWr72K&sig=5_tYjO1HnzLY6846Ayaz576fUqY.
Kessler, R. C., Amminger, G. P., Aguilar-Gaziola, S., Alonso, J., Lee, S., & Ustun, T. B. (2007). Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry, 20(4), 359–364.
Krueger, R. F. (2005). Continuity of Axes I and II: Toward a unified model of personality, personality disorders, and clinical disorders. Journal of Personality Disorders., 19, 233–261. https://doi.org/10.1521/pedi.2005.19.3.233.
Laurenssen, E. M. P., Hutsebaut, J., Feenstra, D. J., Van Busschbach, J. J., & Luyten, P. (2013). Diagnosis of personality disorders in adolescents: a study among psychologists. Child Adolesc Psychiatry Ment Health, 7. https://doi.org/10.1186/1753-2000-7-3.
Lofgren, D. P., Bemporad, J., King, J., Lindem, K., & O’Driscoll, G. (1991). A prospective follow-up study of so-called borderline children. American Journal of Psychiatry, 148(11), 1541–1547.
Mattanah, J. J., Becker, D. F., Levy, K. N., Edell, W. S., & McGlashan, T. H. (1995). Diagnostic stability in adolescents followed up 2 years after hospitalization. American Journal of Psychiatry, 152(6), 889–894. https://doi.org/10.1176/ajp.152.6.889.
Morey, L. (1991). Personality Assessment Inventory. Odessa, FL: Psychological Assessment Resources.
Newman, D. A. (2003). Longitudinal modeling with randomly and systematically missing data: A simulation of ad hoc, maximum likelihood, and multiple imputation techniques. Organizational Research Methods, 6(3), 328–362.
Shaffer, D., Fisher, P., & Lucas, C. P. (2003). The Diagnostic Interview Schedule for Children. In M. Hersen, J. C. Thomas, & G. Goldstein (Eds.), Comprehensive Handbook of Psychological Assessment (pp. 256–270). New York: John Wiley & Sons.
Shanks, C., Pfohl, B., Blum, N., & Black, D. W. (2011). Can negative attitudes toward patients with borderline personality disorder be changed? The effect of attending a STEPPS workshop. Journal of Personality Disorders, 25(6), 806–812. https://doi.org/10.1521/pedi.2011.25.6.806.
Sharp, C., & Fonagy, P. (2015). Practitioner Review: Borderline personality disorder in adolescence–recent conceptualization, intervention, and implications for clinical practice. Journal of Child Psychology and Psychiatry, 56(12), 1266–1288. https://doi.org/10.1111/jcpp.12449.
Sharp, C., Ha, C., Michonski, J., Venta, A., & Carbone, C. (2012). Borderline personality disorder in adolescents: evidence in support of the Childhood Interview for DSM-IV Borderline Personality Disorder in a sample of adolescent inpatients. Comprehensive Psychiatry, 53(6), 765–774. https://doi.org/10.1016/j.comppsych.2011.12.003.
Sharp, C., Michonski, J., Steinberg, L., Fowler, J. C., Frueh, B. C., & Oldham, J. M. (2014). An investigation of differential item functioning across gender of BPD criteria. Journal of Abnormal Psychology, 123(1), 231–236. https://doi.org/10.1037/a0035637.
Sharp, C., Mosko, O., Chang, B., & Ha, C. (2011). The cross-informant concordance and concurrent validity of the Borderline Personality Features Scale for Children in a sample of male youth. Clinical Child Psychology and Psychiatry, 16(3), 35–49.
Sharp, C., Mosko, O., Chang, B., & Ha, C. (2010). The cross-informant concordance and concurrent validity of the Borderline Personality Features Scale for Children in a sample of male youth. Clinical Child Psychology and Psychiatry, 16(3), 335–350. https://doi.org/10.1177/1359104510366279.
Sharp, C., Steinberg, L., Michonski, J., Kalpakci, A., Fowler, C., Frueh, B. C., & Fonagy, P. (2018). DSM borderline criterion function across age-groups: A cross-sectional mixed-method study. Assessment, https://doi.org/10.1177/1073191118786587.
Steiger, J. H., & Lind, J. M. (1980). Statistically based tests for the number of common factors. Iowa City: Paper presented at the Psychometric Society.
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics. Boston: Pearson Education.
Tucker, L., & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10.
Wall, K., Kerr, S., & Sharp, C. (2020). Barriers to care for adolescents with borderline personality disorder. Current Opinion in Psychology.
Wall, K., Ahmed, Y., & Sharp, C. (2019). Parent-adolescent concordance in borderline pathology and why it matters. Journal of Abnormal Child Psychology, 47(4), 669–683. 1–14.
Wenning, K. (1990). Borderline children: a closer look at diagnosis and treatment. American Journal of Orthopsychiatry, 60(2), 225–232.
Westen, D., Shedler, J., Durrett, C., Glass, S., & Martens, A. (2003). Personality diagnoses in adolescence: DSM-IV axis II diagnoses and an empirically derived alternative. American Journal of Psychiatry, 160(5), 952–966. https://doi.org/10.1176/appi.ajp.160.5.952.
Winsper, C., Marwaha, S., Lereya, S. T., Thompson, A., Eyden, J., & Singh, S. P. (2015). Clinical and psychosocial outcomes of borderline personality disorder in childhood and adolescence: a systematic review. Psychological Medicine, 45(11), 2237–2251. https://doi.org/10.1017/S0033291715000318.
Winsper, C., Wolke, D., & Lereya, T. (2015). Prospective associations between prenatal adversities and borderline personality disorder at 11–12 years. Psychological Medicine, 45(5), 1025–1037. https://doi.org/10.1017/S0033291714002128.
Wright, A. G., Zalewski, M., Hallquist, M. N., Hipwell, A. E., & Stepp, S. D. (2016). Developmental trajectories of borderline personality disorder symptoms and psychosocial functioning in adolescence. Journal of Personality Disorders, 30(3), 351–372. https://doi.org/10.1521/pedi_2015_29_200.
Zanarini, M. C. (2003). The Child Interview for DSM-IV Borderline Personality Disorder. Belmont, MA: McLean Hospital.
Zanarini, M. C., Frankenburg, F. R., Hennen, J., Reich, D. B., & Silk, K. R. (2006). Prediction of the 10-year course of borderline personality disorder. American Journal of Psychiatry, 163(5), 827–832. https://doi.org/10.1176/appi.ajp.163.5.827.
Zanarini, M. C., Frankenburg, F. R., Hennen, J., & Silk, K. R. (2003). The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry, 160(2), 274–283.
Funding
The study was supported by the McNair Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no competing interests and wish to thank the families and teens who participated in the study.
Ethical Approval
The study was approved by the relevant ethical board.
Informed Consent
Informed consent was obtained from adolescents and their parents.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharp, C., Vanwoerden, S., Gallagher, M.W. et al. The Course of Borderline Psychopathology in Adolescents with Complex Mental Health Problems: An 18 Month Longitudinal Follow-up Study. Res Child Adolesc Psychopathol 49, 545–557 (2021). https://doi.org/10.1007/s10802-020-00756-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-020-00756-y