Abstract
Balanced action of hemagglutinin (HA) and neuraminidase (NA) is an important condition of influenza virus efficient replication, but a role of HA and NA specificities at oligosaccharide level in maintaining such a balance remains poorly studied. Avian virus HA binds exclusively and NA digests efficiently α2–3-sialylated carbohydrate chains, while human virus HA interacts with α2–6 chains and low-active NA cleaves both α2–3- and α2–6-sialosides. Reassortment between viruses leading to appearance of avian virus HA and human virus NA on the virion surface often resulted in decreasing the replicative potential of the formed variants because of disturbance of a functional balance between “alien” HA and NA. A restoration of the reassortant productivity happened due to the appearance of amino acid substitutions in HA and, sometimes, NA. Here, a role of NA and HA oligosaccharide specificities in a restoration of HA–NA functional balance in high-yield passage variants was studied. Postreassortment changes in HA receptor-binding and NA substrate specificities for three reassortant/passage variant virus pairs towards 3′SiaLac, 3′SiaLacNAc, SiaLec, SiaLea, SiaLex, 6′SiaLac, and 6′SiaLacNAc were determined. Selection of the high-yield variants of the human-avian reassortants led either to twofold decrease in the affinity of HA for most α2–3-sialosides and the appearance of affinity for α2–6-sialosides (H3N2 reassortant), or to decreasing the HA affinity for SiaLec and SiaLea (H3N1 reassortant), or to enhancing the ability of NA to discriminate between α2–3/2–6 substrates (H4N1 reassortant). Thus, all postreassortment changes in oligosaccharide specificities of “alien” HA and NA were directed towards their adjustment to each other, but by different manner.



Similar content being viewed by others
Abbreviations
- biot:
-
biotin
- BODIPY:
-
4,4-difluoro-5,7-dimethyl-4-bora-3a,4a-diaza-s-indacene-3-propionic acid
- BSA:
-
bovine serum albumin
- HA:
-
hemagglutinin
- HAU:
-
hemagglutinating unit
- Kd :
-
dissociation constant
- Kaff :
-
affinity constant
- NA:
-
neuraminidase
- Neu5Ac:
-
N-acetylneuraminic acid
- OS:
-
oligosaccharide
- PAA:
-
polyacrylamide
- S0 :
-
initial substrate concentration
- V0 :
-
initial rate of enzymatic hydrolysis
- 3′SiaLac:
-
Neu5Acα2–3Galβ1–4Glc
- 3′SiaLacNAc:
-
Neu5Acα2–3Galβ1–4GlcNAc
- 6′SiaLac:
-
Neu5Acα2–6Galβ1–4Glc
- 6′SiaLacNAc:
-
Neu5Acα2–6Galβ1–4GlcNAc
- SiaLec :
-
Neu5Acα2–3Galβ1–3GlcNAc
- SiaLea :
-
Neu5Acα2–3Galβ1–3(Fucα1–4)GlcNAc
- SiaLex :
-
Neu5Acα2–3Galβ1–4(Fucα1–3)GlcNAc
- 6Su-3′SiaLacNAc:
-
Neu5Acα2–3Galβ1–4(6-HSO3)GlcNAc
- 6Su-6′SiaLacNAc:
-
Neu5Acα2–6Galβ1–4(6-HSO3)GlcNAc
- TN buffer:
-
0.02 M tris-HCl, pH 7.2, with 0.1 M NaCl
References
Barros Jr., J.F., Alviano, D.S., Silva, M.H., Wigg, M.D., Alviano, C.S., Schauer, R., et al.: Characterization of sialidase from an influenza A (H3N2) virus strain: kinetic parameters and substrate specificity. Intervirology 46, 199–206 (2003). doi:10.1159/000072428
Connor, R.J., Kawaoka, Y., Webster, R.G., Paulson, J.C.: Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205, 17–23 (1994). doi:10.1006/viro.1994.1615
Funning, T.G., Reid, A.H., Taubenberger, J.K.: Influenza A virus neuraminidase: regions of the protein potentially involved in virus-host interactions. Virology 276, 417–423 (2000). doi:10.1006/viro.2000.0578
Gambaryan, A.S., Tuzikov, A.B., Piskarev, V.E., Yamnikova, S.S., Lvov, D.K., Robertson, J.S., et al.: Specification of receptor-binding phenotypes of influenza virus isolates from different hosts using synthetic sialylglycopolymers: non-egg-adapted human H1 and H3 influenza A and influenza B viruses share a common high binding affinity for 6′-sialyl(N-acetyllactosamine). Virology 232, 345–350 (1997). doi:10.1006/viro.1997.8572
Ilyushina, N.A., Rudneva, I.A., Shilov, A.A., Klenk, H.-D., Kaverin, N.V.: Postreassortment changes in a model system: HA-NA adjustment in an H3N2 avian–human reassortant influenza virus. Arch. Virol. 150, 1327–1338 (2005). doi:10.1007/s00705-005-0490-4
Kaverin, N.V., Gambaryan, A.S., Bovin, N.V., Rudneva, I.A., Shilov, A.A., Khodova, O.M., et al.: Postreassortment changes in influenza A virus hemagglutinin restoring HA-NA functional match. Virology 244, 315–321 (1998). doi:10.1006/viro.1998.9119
Kaverin, N.V., Matrosovich, M.N., Gambaryan, A.S., Rudneva, I.A., Shilov, A.A., Varich, N.L., et al.: Intergenic HA-NA interactions in influenza A virus: postreassortment substitutions of charged amino acid in the hemagglutinin of different subtypes. Virus Res. 66, 123–129 (2000). doi:10.1016/S0168-1702(99)00131-8
Kilbourne, E.D.: Influenza. Plenum, New York (1987)
Kobasa, D., Kodihalli, S., Luo, M., Castrucci, M.R., Donatelli, I., Suzuki, Y., et al.: Amino acid resides contributing to the substrate specificity of the influenza A virus neuraminidase. J. Virol. 73, 6743–6751 (1999)
Kobasa, D., Wells, K., Kawaoka, Y.: Amino acids responsible for the absolute sialidase activity of the influenza virus neuraminidase: relationship to growth in the duck intestine. J. Virol. 75, 11773–11778 (2001). doi:10.1128/JVI.75.23.11773-11780.2001
Kumari, K., Gulati, S., Smith, D.F., Gulati, U., Cumming, R.D., Air, G.M.: Receptor binding specificity of recent human H3N2 influenza viruses. Virol. J. 4, 42 (2007). doi:10.1186/1743-422X-4-42
Liu, C., Eichelberger, M.C., Compans, R.W., Air, G.M.: Influenza type A virus neuraminidase does not play a role in virus entry, replication, assembly, or budding. J. Virol. 69, 1099–1106 (1995)
Matrosovich, M., Matrosovich, T., Gray, T., Roberts, N.A., Klenk, H.-D.: Neuraminidase is important for the initiation of influenza virus infection in human airway epithelium. J. Virol. 78, 12665–12667 (2004). doi:10.1128/JVI.78.22.12665-12667.2004
Matrosovich, M.N., Klenk, H.-D., Kawaoka, Y.: Receptor specificity, host-range, and pathogenicity of influenza viruses. In: Kawaoka, Y. (ed.) Influenza Virology: Current Topics, pp. 95–137. Caister, Norfolk (2006)
Mitnaul, L.J., Matrosovich, M.N., Castrucci, M.R., Tuzikov, A.B., Bovin, N.V., Kobasa, D., et al.: Balanced hemagglutinin and neuraminidase activities are critical for replication of influenza A virus. J. Virol. 74, 6015–6020 (2000). doi:10.1128/JVI.74.13.6015-6020.2000
Mochalova, L., Gambaryan, A., Romanova, J., Tuzikov, A., Chinarev, A., Katinger, D., et al.: Receptor-binding properties of modern human influenza viruses primarily isolated in Vero and MDCK cells and chicken embryonated eggs. Virology 313, 437–480 (2003). doi:10.1016/S0042-6822(03)00377-5
Mochalova, L.V., Korchagina, E.Y., Kurova, V.S., Shtyrya, J.A., Gambaryan, A.S., Bovin, N.V.: Fluorescent assay for studying the substrate specificity of neuraminidase. Anal. Biochem. 34, 190–193 (2005). doi:10.1016/j.ab.2005.02.019
Mochalova, L., Kurova, V., Shtyrya, J., Korchagina, E., Gambaryan, A., Belyanchikov, I., et al.: Oligosaccharide specificity of influenza H1N1 virus neuraminidases. Arch. Virol. 152, 2047–2057 (2007). doi:10.1007/s00705-007-1024-z
Palese, P., Tobita, K., Ueda, M., Compans, R.W.: Characterization of temperature-sensitive influenza virus mutants defective in neuraminidase. Virology 61, 397–410 (1974). doi:10.1016/0042-6822(74)90276-1
Pazynina, G., Tuzikov, A., Chinarev, A., Obukhova, P., Bovin, N.: Simple stereoselective synthesis of alfa2–6 sialo-oligosaccharides. Tetrahedron Lett. 43, 8011–8013 (2002). doi:10.1016/S0040-4039(02)01983-4
Pazynina, G.V., Sablina, M.A., Tuzikov, A.B., Chinarev, A.A., Bovin, N.V.: Synthesis of complex 2–3 sialo-oligosaccharides, including sulfated and fucosylated ones, using Neu5Ac alfa2–3Gal as a building block. Mendeleev Commun. 13, 245–248 (2003). doi:10.1070/MC2003v013n06ABEH001845
Rudneva, I.A., Kovaleva, V.P., Varich, N.L., Farashyan, V.R., Gubareva, L.V., Yamnikova, S.S., et al.: Influenza A virus reassortants with surface glycoprotein genes of the avian parent viruses: effects of HA and NA gene combinations on virus aggregation. Arch. Virol. 133, 437–450 (1993). doi:10.1007/BF01313781
Rudneva, I.A., Sklyanskaya, E.I., Barulina, O.S., Yamnikova, S.S., Kovaleva, V.P., Tsvetkova, I.V., et al.: Phenotypic expression of HA-NA combinations in human-avian influenza A virus reassortants. Arch. Virol. 141, 1091–1099 (1996). doi:10.1007/BF01718612
Shtyrya, Y., Mochalova, L., Gambarayn, A., Korchagina, E., Xu, X., Klimov, A., et al: Neuraminidases of H9N2 influenza viruses isolated from different hosts display various substrate specificity. In Options for the control of influenza VI Conference, p.14. Toronto (2007)
Suzuki, Y., Kato, H., Naeve, W., Webster, R.: Single-amino-acid Substitution in an antigenic site of influenza virus hemagglutinin can alter the specificity of binding to cell membrane-associated gangliosides. J. Virol. 63, 4298–4302 (1989)
Tumpey, T.M., Maines, T.R., Hoeven, N.V., Glaser, L., Solorzano, A., Pappas, C., et al.: A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315, 655–659 (2007). doi:10.1126/science.1136212
Tuzikov, A.B., Gambaryan, A.S., Juneja, L.R., Bovin, N.V.: Conversion of complex sialo-oligosaccharides into polymeric conjugates and their anti-influenza virus inhibitory potency. J. Carbohydr. Chem. 19, 1191–1200 (2000). doi:10.1080/07328300008544143
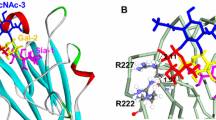
Varghese, J.N., Colman, P.M., van Donkelaar, A., Blick, T.J., Sharasrabudhi, A.: McKimm –Breshkin JL, Structural evidence for a second sialic acid binding site in avian influenza virus neuraminidases. Biochemistry 94, 11808–11812 (1997)
Wagner, R., Wolff, T., Herwig, A., Pleschka, S., Klenk, H.-D.: Interdependence of hemagglutinin glycosylation and neuraminidase as regulators of influenza virus growth: a study by reverse genetics. J. Virol. 74, 6316–6323 (2000). doi:10.1128/JVI.74.14.6316-6323.2000
Wagner, R., Matrosovich, M., Klenk, H.-D.: Functional balance between hemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12, 159–166 (2002). doi:10.1002/rmv.352
Acknowledgments
The work was supported by grants of Russian Foundation for Basic Research 07-04-00663 and 06-04-48085, and the Russian Academy of Sciences Presidium Program “Molecular and Cell Biology”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shtyrya, Y., Mochalova, L., Voznova, G. et al. Adjustment of receptor-binding and neuraminidase substrate specificties in avian–human reassortant influenza viruses. Glycoconj J 26, 99–109 (2009). https://doi.org/10.1007/s10719-008-9169-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10719-008-9169-x