Abstract
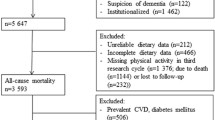
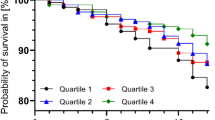
Background The associations between dietary indices and mortality have not been evaluated in populations from the Middle East, which have different dietary patterns compared to the US and Europe. In this study, we evaluated the association between six dietary indices and mortality in the Golestan Cohort Study (GCS) in Iran, which is the largest prospective study in the Middle East with 50,045 participants. Methods The six dietary indices, namely the Healthy Eating Index (HEI-2015), Alternative Healthy Eating Index (AHEI-2010), Alternative Mediterranean Diet (AMED), Dietary Approach to Stop Hypertension created by Fung (DASH-Fung) and Mellen (DASH-Mellen), and the World Cancer Research Fund (WCRF/AICR) index, were applied to data from a food frequency questionnaire, computed and divided into quintiles. Adjusted Cox models were used to estimate hazards ratio (HR) and 95% confidence intervals (CI) for overall and cause-specific mortality, using the lowest quintile as a reference group. Results Among 42,373 participants included in the current analyses, 4424 subjects died during 10.6 years of follow-up. Participants with the highest quintile dietary scores, compared with the lowest quintile dietary scores, had significantly decreased overall mortality in the AHEI-2010, AMED, DASH-Fung, and WCRF/AICR indices (HR 0.88, 95% CI = 0.80–0.97; 0.80, 0.70–0.91; 0.77, 0.70–0.86; and 0.79, 0.70–0.90, respectively). A reduced cardiovascular mortality was found for high AHEI-2010 and DASH-Fung scores (17% and 23%, respectively), and a reduced cancer mortality for high HEI-2015, AMED, and DASH-Fung scores (21, 37 and 25%, respectively). Conclusion Various indices of dietary quality are inversely associated with overall mortality, and selectively with cancer and cardiovascular mortality in the GCS, which contribute to the generalizability and validity of dietary guidelines.
Similar content being viewed by others
References
Micha R, et al. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–24.
Eslamparast T, et al. Nut consumption and total and cause-specific mortality: results from the Golestan Cohort Study. Int J Epidemiol. 2017;46(1):75–85.
Schwingshackl L, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2017;105(6):1462–73.
Ilic M, et al. Association of the consumption of common food groups and beverages with mortality from cancer, ischaemic heart disease and diabetes mellitus in Serbia, 1991–2010: an ecological study. BMJ Open. 2016;6(1):e008742.
Reedy J, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6):881–9.
Kennedy ET, et al. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–8.
National Cancer Institute; National Institutes of Health. Dietary Patterns Methods Project. https://epi.grants.cancer.gov/hei/hei-2015-table1.html.
McCullough ML, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–71.
Chiuve SE, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–18.
Dinu M, et al. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2017;27(1):e21.
Mellen PB, et al. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168(3):308–14.
World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC: AICR; 2007.
Fung TT, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20.
Romaguera D, et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr. 2012;96(1):150–63.
Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780–800.
Liese AD, et al. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393–402.
Sheikh M, et al. Individual and combined effects of environmental risk factors for esophageal cancer based on results from the Golestan Cohort Study. Gastroenterology. 2019. https://doi.org/10.1053/j.gastro.2018.12.024.
Pourshams A, et al. Cohort profile: the Golestan Cohort Study–a prospective study of oesophageal cancer in northern Iran. Int J Epidemiol. 2010;39(1):52–9.
Khademi H, et al. Verbal autopsy: reliability and validity estimates for causes of death in the Golestan Cohort Study in Iran. PLoS ONE. 2010;5(6):e11183.
Malekshah AF, et al. Validity and reliability of a new food frequency questionnaire compared to 24 h recalls and biochemical measurements: pilot phase of Golestan cohort study of esophageal cancer. Eur J Clin Nutr. 2006;60(8):971–7.
Azar M, Sarkisian E. Food composition table of Iran. Tehran: National Nutrition and Food Technology Research Institute of Iran; 1981.
U.S. Department of Agriculture, A.R.S., USDA National Nutrient Database for Standard Reference. Release 23, Nutrient Data Laboratory. http://www.ars.usda.gov/ba/bhnrc/ndl.
Bowman SA, C.J., Friday JE, Lynch KL, and Moshfegh AJ, Food patterns equivalents database 2013–14: Methodology and User Guide. Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture, Beltsville, Maryland. http://www.ars.usda.gov/nea/bhnrc/fsrg.
Bowman SA, M.C., Carlson JL, Clemens JC, Lin B-H, and Moshfegh AJ, Food intakes converted to retail commodities databases: 2003–08: methodology and user guide, A.R.S. U.S. Department of Agriculture, Beltsville, MD, and U.S. Department of Agriculture, Economic Research Service, Editor. 2013: Washington, D.C. p. 48.
Miller PE, et al. Sugar-sweetened beverage consumption in the U.S.: novel assessment methodology. Am J Prev Med. 2013;45(4):416–21.
Fung TT, et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–73.
Muller DC, et al. Modifiable causes of premature death in middle-age in Western Europe: results from the EPIC cohort study. BMC Med. 2016;14:87.
Islami F, et al. Socio-economic status and oesophageal cancer: results from a population-based case-control study in a high-risk area. Int J Epidemiol. 2009;38(4):978–88.
Hashemian M, et al. Dietary intake of minerals and risk of esophageal squamous cell carcinoma: results from the Golestan Cohort Study. Am J Clin Nutr. 2015;102(1):102–8.
Etemadi A, et al. Impact of body size and physical activity during adolescence and adult life on overall and cause-specific mortality in a large cohort study from Iran. Eur J Epidemiol. 2014;29(2):95–109.
Harmon BE, et al. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101(3):587–97.
George SM, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616–25.
Neelakantan N, et al. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among Chinese adults. J Nutr. 2018;148(8):1323–32.
Lohse T, et al. Adherence to the cancer prevention recommendations of the World Cancer Research Fund/American Institute for Cancer Research and mortality: a census-linked cohort. Am J Clin Nutr. 2016;104(3):678–85.
Miller PE, et al. Comparison of 4 established DASH diet indexes: examining associations of index scores and colorectal cancer. Am J Clin Nutr. 2013;98(3):794–803.
Baer HJ, et al. Risk factors for mortality in the nurses’ health study: a competing risks analysis. Am J Epidemiol. 2011;173(3):319–29.
Soliman GA. Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients. 2018;10(6):780.
Kanter MM, et al. Exploring the factors that affect blood cholesterol and heart disease risk: is dietary cholesterol as bad for you as history leads us to believe? Adv Nutr. 2012;3(5):711–7.
Macpherson H, Pipingas A, Pase MP. Multivitamin-multimineral supplementation and mortality: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2013;97(2):437–44.
Michaelsson K, et al. Long term calcium intake and rates of all cause and cardiovascular mortality: community based prospective longitudinal cohort study. BMJ. 2013;346:f228.
Li K, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012;98(12):920–5.
Xiao Q, et al. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639–46.
Fang X, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. 2016;14(1):210.
Hashemian M, et al. Systematic review of zinc biochemical indicators and risk of coronary heart disease. ARYA Atheroscler. 2015;11(6):357–65.
Eshak ES, et al. Associations between copper and zinc intakes from diet and mortality from cardiovascular disease in a large population-based prospective cohort study. J Nutr Biochem. 2018;56:126–32.
Hashemian M, et al. Systematic review of zinc biomarkers and esophageal cancer risk. Middle East J Dig Dis. 2014;6(4):177–85.
Khademi H, et al. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50,000 adults in Iran. BMJ. 2012;344:e2502.
Abnet CC, et al. Reliability and validity of opiate use self-report in a population at high risk for esophageal cancer in Golestan, Iran. Cancer Epidemiol Biomark Prev. 2004;13(6):1068–70.
Acknowledgements
We are grateful to all participants of the study, and the Golestan Cohort Study for expert help in collecting the data.
Funding
This work was supported by the World Cancer Research Fund International (Grant Number: WCRF 2016/1633), Tehran University of Medical Sciences (Grant Number: 81/15), Cancer Research UK (grant number: C20/A5860), the Intramural Research Program of the U.S. National Cancer Institute, National Institutes of Health, and the International Agency for Research on Cancer.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Review Boards of the U.S. National Cancer Institute (NCI), the International Agency for Research on Cancer (IARC), and the Digestive Disease Research Institute of the Tehran University of Medical Sciences (DDRI). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hashemian, M., Farvid, M.S., Poustchi, H. et al. The application of six dietary scores to a Middle Eastern population: a comparative analysis of mortality in a prospective study. Eur J Epidemiol 34, 371–382 (2019). https://doi.org/10.1007/s10654-019-00508-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-019-00508-3