Abstract
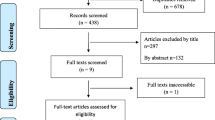
Iodine deficiency is a global public health issue because iodine plays a major role in the thyroid hormone synthesis and is essential for normal neurological development. This review summarizes the publications on iodine status in the WHO Eastern Mediterranean Region (EMR) countries. All related studies available in main national and international databases were systematically searched using some specific keywords to find article published between 1909 and 2015. The prevention of iodine deficiency disorders (IDDs) in the WHO EMR countries is currently under control without significant side effects. Mild to severe IDDs exist in some countries of the Middle East, due to lack of effective iodine supplementation program, but the Islamic Republic of Iran, Jordan, Bahrain and Tunisia have achieved the goal of universal salt iodization. Overall, despite enormous efforts to control IDDs, still IDD remains a serious public health problem in some countries of the region, requiring urgent control and prevention measures.

Similar content being viewed by others
References
Abbag, F. I., Abu-Eshy, S. A., Mahfouz, A. A., Al-Fifi, S. A., El-Wadie, H., Abdallah, S. M., et al. (2015). Iodine-deficiency disorders in the Aseer region, south-western Saudi Arabia: 20 years after the national survey and universal salt iodization. Public Health Nutrition, 18, 2523–2529.
Al-Hosani, H., Osman, H., Abdel Wareth, L., Saade, D., & Salah, M. (2003). Prevalence of iodine deficiency disorders in the United Arab Emirates measured by raised TSH levels. Eastern Mediterranean Health Journal, 9, 123–130.
Al-Hureibi, K. A., Abdulmughni, Y. A., Al-Hureibi, M. A., Al-Hureibi, Y. A., & Ghafoor, M. A. (2004). The epidemiology, pathology, and management of goitre in Yemen. Annals of Saudi Medicine, 24, 119–123.
Al-Jaradi, M., Sallam, A., Jabr, H., Borda, A., Decaussin-Petrucci, M., & Berger, N. (2005). Prevalence of differentiated thyroid cancer in 810 cases of surgically treated goiter in Yemen. Annals of Saudi Medicine, 25, 394–397.
Al-Nuaim, A. R., Al-Mazrou, Y., Kamel, M., Al-Attas, O., Al-Daghari, N., & Sulimani, R. (1997). Iodine deficiency in Saudi Arabia. Annals of Saudi Medicine, 17, 293–297.
Alsanosy, R. M. A., Gaffar, A. M., Khalafalla, H. E. E., Mahfouz, M. S., Zaid, A. N. S., & Bani, I. A. (2012). Current iodine nutrition status and progress toward elimination of iodine deficiency disorders in Jazan, Saudi Arabia. BMC Public Health, 12, 1006.
Al-Yatama, F. I., Al-Bader, M. D., Al-Mazidi, Z. M., Ali, A., Al-Omair, A., Al-Ajmi, N. H., et al. (2007). Iodine status among pregnant women in Kuwait. Journal of Endocrinological Investigation, 30, 914–919.
Al-Yatama, F., Al-Bader, M., Al-Mazidi, Z., Ali, A., Al-Omair, A., Al-Jehma, N., et al. (2009). Assessment of urinary iodine excretion among normal Kuwaiti adults. Biological Trace Element Research, 132, 67–74.
Andersson, M., De Benoist, B., Delange, F., & Zupan, J. (2007). Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the Technical Consultation. Public Health Nutrition, 10, 1606–1611.
Andersson, M., Karumbunathan, V., & Zimmermann, M. B. (2012). Global iodine status in 2011 and trends over the past decade. The Journal of Nutrition, 142, 744–750.
Andersson, M., Takkouche, B., Egli, I., Allen, H. E., & De Benoist, B. (2005). Current global iodine status and progress over the last decade towards the elimination of iodine deficiency. Bulletin of the World Health Organization, 83, 518–525.
Aquaron, R., Zarrouck, K., El Jarari, M., Ababou, R., Talibi, A., & Ardissone, J. P. (1993). Endemic goiter in Morocco (Skoura-Toundoute areas in the high atlas). Journal of Endocrinological Investigation, 16, 9–14.
Azizi, F. (2002). Assessment, monitoring and evaluation of iodine deficiency disorders in the Middle East and Eastern Mediterranean Region. Teheran: Sara.
Azizi, F., & Mehran, L. (2004). Experiences in the prevention, control and elimination of iodine deficiency disorders: A regional perspective. Eastern Mediterranean Health Journal, 10, 761–770.
Azizi, F., Mehran, L., Sheikholeslam, R., Ordookhani, A., Naghavi, M., Hedayati, M., et al. (2008). Sustainability of a well-monitored salt iodization program in Iran: Marked reduction in goiter prevalence and eventual normalization of urinary iodine concentrations without alteration in iodine content of salt. Journal of Endocrinological Investigation, 31, 422–431.
Azizi, F., Navai, L., & Fattahi, F. (2002). Goiter prevalence, urinary iodine excretion, thyroid function and anti-thyroid function and anti-thyroid antibodies after 12 years of salt iodization in Shahriar, Iran. International Journal for Vitamin and Nutrition Research, 72, 291–295.
Bani, I. (2007). Accelerating progress on salt iodisation in Sudan: Time for action. Disasters, 31, S139–S149.
Caughey, J., & Follis, R. (1965a). Endemic goitre and iodine malnutrition in Iraq. The Lancet, 285, 1032–1034.
Caughey, J. E., & Follis, R. H. (1965b). Endemic goitre and iodine malnutrition in Iraq. The Lancet, 1, 1032–1034.
De Benoist, B., Andersson, M., Egli, I., Takkouche, B., & Allen, H. (2004). Iodine status wordwide, WHO Global Database on Iodine Deficiency. Geneva: World Health Organization.
De Benoist, B., & Delange, F. (2002). Iodine deficiency: Current situation and future prospects. Sante, 12, 9–17.
Delange, F., De Benoist, B., Pretell, E., & Dunn, J. T. (2001). Iodine deficiency in the world: Where do we stand at the turn of the century? Thyroid, 11, 437–447.
Delshad, H., Mehran, L., & Azizi, F. (2010). Appropriate iodine nutrition in Iran: 20 years of success. Acta Medica Iranica, 48, 361–366.
Ebrahim, S., & Muhammed, N. (2012). Consumption of iodized salt among households of Basra city, South Iraq. Eastern Mediterranean Health Journal, 18, 980–984.
El May, M. V., Boukhris, K., Kraiem, A., & Mtimet, S. (1993). Goiter and iodine in Tunisia. Annales de Biologie Clinique (Paris), 51, 723–724.
Elahi, S., Rizvi, N. B., & Nagra, S. A. (2009). Iodine deficiency in pregnant women of Lahore. The Journal of the Pakistan Medical Association, 59, 741–743.
El-Mougi, F. A., Abd-El-Ghaffar, S., Fayek, N. A., & Mohammed, M. S. (2004). Urinary iodine and other iodine deficiency indicators in a sample of school-age children in Egypt. Eastern Mediterranean Health Journal, 10, 863–870.
El-Sayed, N. A., Mahfouz, A. A., Nofal, L., Ismail, H. M., Gad, A., & Zeid, H. A. (1998). Iodine deficiency disorders among school children in upper Egypt: An epidemiologic study. Journal of Tropical Pediatrics, 44, 270–274.
Eltom, M., Hofvander, Y., Torelm, I., & Fellström, B. (1984). Endemic goitre in the Darfur region (Sudan). Acta Medica Scandinavica, 215, 467–475.
Emami, A., Shahbazi, H., Sabzevari, M., Gawam, Z., Sarkissian, N., Hamedi, P., et al. (1969). Goiter in Iran. The American Journal of Clinical Nutrition, 22, 1584–1588.
Erdoğan, M., Ağbaht, K., Altunsu, T., Özbaş, S., Yücesan, F., Tezel, B., et al. (2009). Current iodine status in Turkey. Journal of Endocrinological Investigation, 32, 617–622.
FAO. (2005). Syrian Arab Republic Nutrition Profile—Food and Nutrition Division. FAO.
Izzeldin Hussein, A. G., & Al Osfor, D. (2010). An effective iodized salt program in oman. Oman: IDD Newsletter Oman.
Kandhro, G. A., Kazi, T. G., Kolachi, N. F., Kazi, N., Afridi, H. I., Baig, J. A., et al. (2011). Effects of selenium supplementation on iodine and thyroid hormone status in a selected population with goitre in Pakistan. Clinical Laboratory, 57, 575–585.
Kharabsheh, S., Belbesi, A., Qarqash, W., & Azizi, F. (2004). Goiter prevalence and urinary iodine excretion in schoolchildren of Jordan. International Journal for Vitamin and Nutrition Research, 74, 301–304.
Knudsen, N., Laurberg, P., Perrild, H., Bulow, I., Ovesen, L., & Jorgensen, T. (2002). Risk factors for goiter and thyroid nodules. Thyroid, 12, 879–888.
Kut, A., Gursoy, A., Senbayram, S., Bayraktar, N., Budakoglu, I., & Akgun, H. S. (2010). Iodine intake is still inadequate among pregnant women eight years after mandatory iodination of salt in Turkey. Journal of Endocrinological Investigation, 33, 461–464.
Mahfouz, M. S., Gaffar, A. M., & Bani, I. A. (2012). Iodized salt consumption in Sudan: Present status and future directions. Journal of Health, Population and Nutrition, 30, 431–438.
Mccarrison, R. (1909). Observations on endemic cretinism in the Chitral and Gilgit valleys. Journal of the Royal Society of Medicine, 2, 1–36.
Mirmiran, P., Golzarand, M., Serra-Majem, L., & Azizi, F. (2012). Iron, iodine and vitamin a in the middle East; A systematic review of deficiency and food fortification. Iranian Journal of Public Health, 41, 8–19.
Mohamed, S., El Tawila, M., Ismail, H., & Gomaa, N. (2010). Evaluation of the level of micronutrients in fortified foods in Alexandria, Egypt. Eastern Mediterranean Health Journal, 16(7), 793–800.
Moosa, K., Abdul Wahab, A. W., Al-Sayyad, J., & Baig, B. Z. (2001). National study on the prevalence of iodine deficiency disorders among schoolchildren 8–12 years of age in Bahrain. Eastern Mediterranean Health Journal, 7, 609–616.
Moussa W. (1998). Assignment report. Syrian Arab Republic.
Oberlin, O., Plantin-Carrenard, E., Rigal, O., & Wilkinson, C. (2006). Goitre and iodine deficiency in Afghanistan: A case–control study. British Journal of Nutrition, 95, 196–203.
Oguz Kutlu, A., & Kara, C. (2012). Iodine deficiency in pregnant women in the apparently iodine-sufficient capital city of Turkey. Clinical Endocrinology (Oxford), 77, 615–620.
Pearce, E. N., Andersson, M., & Zimmermann, M. B. (2013). Global iodine nutrition: Where do we stand in 2013? Thyroid, 23, 523–528.
Ramalingaswami, V. (1973). Endemic goiter in Southeast Asia. New clothes on an old body. Annals of Internal Medicine, 78, 277–283.
Regional Meeting for the Promotion of Iodized Salt in the Eastern Mediterranean, East and North Africa Region. Dubai: United Arab Emirates 2000.
Syrian Ministry of Health. (1997). A survey on the household utilization of the iodized salt, in collaboration with United Nations Children’s Fund (UNICEF). Syrian Ministry of Health 1997.
Syrian Ministry of Health. (2004). A study on Syrian families’ utilization of the iodized salt, in collaboration with WHO and UNICEF. Syrian Ministry of Health.
UNICEF. (2000). Multiple indicator cluster suvey (MICS). Sudan—final report. Federal Ministry of Health, Republic of Sudan 200180.
UNICEF. (2002). Iodine Deficiency Disorders and Universal Salt Iodisation: South Asia Priorities. New York: UNICEF.
UNICEF. (2007). State of the world’s children 2007, women and children: The double dividend of gender equality. New York: UNICEF.
UNICEF. (2008). Sustainable Elimination of Iodine Deficiency. New York: The United Nations Children’s Fund (UNICEF).
UNICEF. (2013a). Review of national legislation for universal salt iodization: South Asia and East Asia and the Pacific. New York: UNICEF.
UNICEF. (2013b). Improving child nutrition: The achievable imperative for global progress. Geneva: United Nations Children’s Fund (UNICEF).
Uzun, H., Gozkaya, S., Yesildal, N., Okur, M., Arslanoglu, I., Kocabay, K., et al. (2014). The prevalence of goiter and hypothyroidism among school children 6 years after introduction of a mandatory salt iodination program in a severely iodine-deficient area of the West Black Sea region of Turkey. Journal of Tropical Pediatrics, 60, 318–321.
Van Den Briel, T., West, C. E., Hautvast, J. G., Vulsma, T., De Vijlder, J. J., & Ategbo, E. A. (2001). Serum thyroglobulin and urinary iodine concentration are the most appropriate indicators of iodine status and thyroid function under conditions of increasing iodine supply in schoolchildren in Benin. The Journal of Nutrition, 131, 2701–2706.
WHO. (2008). Elimination of iodine deficiency disorders: A manual for health workers. Geneva: WHO.
World Health Organization. (1993). Indicators for assessing iodine deficiency disorders and their control programmes. Geneva: World Health Organization.
World Health Organization. (2007). Assessment of iodine deficiency disorders and monitoring their elimination: A guide for programme managers. Geneva: World Health Organization.
Yamamah, G. A. E. N., Kamel, A. F., Abd-El Dayem, S., Hussein, A. S., & Salama, H. (2013). Thyroid volumes and iodine status in Egyptian South Sinai schoolchildren. Archives of Medical Science, 9, 548–554.
Yordam, N., Ozon, A., Alikasifoglu, A., Ozgen, A., Ceren, N., Zafer, Y., et al. (1999). Iodine deficiency in Turkey. European Journal of Pediatrics, 158, 501–505.
Zein, A., Al-Haithamy, S., Obadi, Q., & Noureddin, S. (2000). The epidemiology of iodine deficiency disorders (IDD) in Yemen. Public Health Nutrition, 3, 245–252.
Zimmermann, M. B. (2008). Iodine requirements and the risks and benefits of correcting iodine deficiency in populations. Journal of Trace Elements in Medicine and Biology, 22, 81–92.
Zimmermann, M. B. (2012). The effects of iodine deficiency in pregnancy and infancy. Paediatric and Perinatal Epidemiology, 26(Suppl 1), 108–117.
Zimmermann, M. B., Wegmueller, R., Zeder, C., Chaouki, N., Biebinger, R., Hurrell, R. F., et al. (2004a). Triple fortification of salt with microcapsules of iodine, iron, and vitamin A. The American Journal of Clinical Nutrition, 80, 1283–1290.
Zimmermann, M. B., Wegmueller, R., Zeder, C., Chaouki, N., Rohner, F., Saissi, M., et al. (2004b). Dual fortification of salt with iodine and micronized ferric pyrophosphate: A randomized, double-blind, controlled trial. The American Journal of Clinical Nutrition, 80, 952–959.
Zimmermann, M. B., Wegmuller, R., Zeder, C., Chaouki, N., & Torresani, T. (2004c). The effects of vitamin A deficiency and vitamin A supplementation on thyroid function in goitrous children. The Journal of Clinical Endocrinology and Metabolism, 89, 5441–5447.
Acknowledgements
The authors wish to acknowledge Ms. Niloofar Shiva for critical editing of English grammar and syntax of the manuscript.
Funding
The study was funded by the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Neither author has any conflict of interests to declare in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Mohammadi, M., Azizi, F. & Hedayati, M. Iodine deficiency status in the WHO Eastern Mediterranean Region: a systematic review. Environ Geochem Health 40, 87–97 (2018). https://doi.org/10.1007/s10653-017-9911-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10653-017-9911-z