Abstract
Background
There is likely variation in approach and management of patient with EoE due to lack of standardized care and variation in guidelines. We aimed to identify current practices regarding diagnosis and treatment in children with eosinophillic esophagitis (EoE) in Australia and New Zealand (ANZ).
Methods
Information on current diagnostic and management approaches for pediatric EoE was collected via an online survey sent to pediatric gastroenterologists (pGE) in ANZ. We performed a cross-sectional study of pGE using a 49-question instrument regarding evaluation, diagnostic, and therapeutic aspects of EoE between October 2019 and December 2019.
Results
Eighty-five percent of the survey responders were from Australia, and 66% were academic. 30% pGE perform > 3 esophageal biopsies for diagnosis of EoE, 40% involve an allergist, 30% use a twice daily PPI trial, and 70% do not exclude other cause of esophageal eosinophilia. For management, only 3% use dietary elimination as an initial therapy, and 24% use less than the recommended doses of swallowed fluticasone. Forty-nine percent were likely to stop treatment in after remission is achieved for 12 months. The EoE endoscopic reference score (EREFS) was not routinely used (49%). Two-thirds of pGE are concerned about long-term effects of recurrent need of general anesthesia.
Conclusions
Diagnostic and management strategies for EoE differed widely among pGE in ANZ, including in diagnostic biopsies, assessing competing causes of esophageal eosinophilia, initials selection of treatments, and maintenance strategies. This variability likely reflects continued uncertainty regarding optimal management strategies and stresses the need for pediatric-specific ANZ guidelines to standardize EoE care.



Similar content being viewed by others
Abbreviations
- EoE:
-
Eosinophilic esophagitis
- pGE:
-
Pediatric gastroenterologist
- EREFS:
-
Eosinophilic esophagitis endoscopic reference score
References
Dellon ES, Erichsen R, Baron JA, et al. The increasing incidence and prevalence of eosinophilic oesophagitis outpaces changes in endoscopic and biopsy practice: national population-based estimates from Denmark. Aliment Pharmacol Ther. 2015;41:662–670.
Noel R, Putnam P, Rothenberg M. Eosinophilic esophagitis. N Engl J Med. 2004;351:940–941.
Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3–20.
Spergel JM, Book WM, Mays E, et al. Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States. J Pediatr Gastroenterol Nutr. 2011;52:300–306.
Sealock RJ, Rendon G, El-Serag HB. Systematic review: the epidemiology of eosinophilic oesophagitis in adults. Aliment Pharmacol Ther. 2010;32:712–719.
Navarro P, Arias A, Arias-Gonzalez L, Laserna-Mendieta EJ, Ruiz-Ponce M, Lucendo AJ. Systematic review with meta-analysis: the growing incidence and prevalence of eosinophilic oesophagitis in children and adults in population-based studies. Aliment Pharmacol Ther. 2019;46:1116–1125.
Dellon ES, Jensen ET, Martin CF, Shaheen NJ, Kappelman MD. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol. 2014;12:e1.
Hirano I, Moy N, Heckman MG, Thomas CS, Gonsalves N, Achem SR. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: validation of a novel classification and grading system. Gut. 2013;62:489–495.
Lucendo AJ, Molina-Infante J, Arias A, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United Eur Gastroenterol J. 2017;5:335–358.
Zifman E, Banai H, Shamir R, et al. Practice differences in the diagnosis and management of eosinophillic esophagitis among adult and pediatric gastroenterologist in Israel. J Pediatr Gastroenterol Nutr. 2018;67:34–39.
Tourlamain G, Garcia-Puig R, Gutiérrez-Junquera C, et al. Differences in management of eosinophilic esophagitis in Europe: an assessment of current practice. J Pediatr Gastroenterol Nutr. 2020;71(1):83–90. https://doi.org/10.1097/MPG.0000000000002672.
Miehlke S, von Arnim U, Schlag C, et al. Clinical management of eosinophilic esophagitis—a nationwide survey among gastroenterologists in Germany. Z Gastroenterol. 2019;57:745–752.
Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guidelines: evidence based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. 2013;108:679–692. (quiz 93).
Rosen R, Vandenplas Y, Singendonk M, et al. Paediatric gastroesophageal reflux clinical practice guidelines: joint recommendation of the North American Society for Paediatric Gastroenterology, Hepatology, and Nutrition and The European Society for Paediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2018;66:516–554.
Leung AK, Hon KL. Gastroesophageal reflux in children: an update review. Drugs Context. 2019;8:212591.
Gonsalves N, Policarpio-Nicolas M, Zhang Q, et al. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointest Endosc. 2006;64:313–319.
Huang KZ, Jensen ET, Chen HX, et al. Practice pattern variation in paediatric eosinophillic esophagitis in the Carolinas EoE collaborative: a research model in community and academic practices. South Med J. 2018;111:328–332.
Dellon ES, Liacouras CA, Molina-Infante J, et al. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE conference. Gastroenterology. 2018;155:102233.e10.
Godwin B, Liacouras C, Mehta V, et al. A review of tertiary referrals for management of pediatric esophageal eosinophilia. Front Pediatr. 2018;6:173.
Eluri S, Iglesia EGA, Massaro M, Peery AF, Shaheen NJ, Dellon ES. Practice patterns and adherence to clinical guidelines for diagnosis and management of eosinophilic esophagitis among gastroenterologists. Dis. Esophagus. 2020;33:doaa025. https://doi.org/10.1093/dote/doaa025.
Chang JW, Saini SD, Mellinger JL, Chen JW, Zikmund-Fisher BJ, Rubenstein JH. Management of eosinophilic esophagitis is often discordant with guidelines and not patient-centered: results of a survey of gastroenterologists. Dis Esophagus. 2019;32:133.
Hiremath G, Vaezi MF, Gupta SK, Acra S, Dellon ES. Management of esophageal food impaction varies among gastroenterologists and affects identification of eosinophilic esophagitis. Dig Dis Sci. 2018;63:1428–1437. https://doi.org/10.1007/s10620-018-4972-0.
Peery AF, Shaheen NJ, Dellon ES. Practice patterns for the evaluation and treatment of eosinophilic oesophagitis. Aliment Pharmacol Ther. 2010;32:1373–1382.
Dellon ES, Hirano I. Epidemiology and natural history of eosinophilic esophagitis. Gastroenterology. 2018;154:e3.
Hirano I, Chan E, Rank M, et al. AGA institute and the joint task force on allergy-immunology practice parameters clinical guidelines for the management of eosinophilic esophagitis. Gastroenterology. 2020;158:1776–1786.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Variation in Diagnosis and Treatment of Pediatric Eosinophilic Osophagitis (EoE) Among Pediatric Gastroenterologist in Australia and New Zealand
Appendix: Variation in Diagnosis and Treatment of Pediatric Eosinophilic Osophagitis (EoE) Among Pediatric Gastroenterologist in Australia and New Zealand
A. Diagnosis: The first set of questions is about diagnosis of eosinophilic esophagitis (EoE).
-
1.
Have you ever diagnosed or treated a patient with EoE?
-
Yes
-
No, (skip to Section C)
-
-
2.
How many patients would you estimate on average that you see with EoE over the span of 1 month?
-
1–5
-
5–10
-
10–20
-
More than 20
-
None
-
-
3.
What symptoms would make you consider the diagnosis of EoE? (check all that apply)
-
Heartburn
-
Regurgitation
-
Refractory reflux
-
Chest pain
-
Abdominal pain
-
Dysphagia
-
Odynophagia
-
Food impaction
-
Nausea
-
Vomiting
-
Weight loss
-
Anemia
-
Hematemesis
-
Fussy eater
-
Feed refusal
-
Failure to gain weight
-
-
4.
What endoscopic findings do you consider consistent with the diagnosis of EoE? (check all that apply)
-
Esophageal rings
-
Esophageal stricture
-
Esophageal ulcer
-
Esophageal nodule
-
Esophageal mass
-
Narrow caliber esophagus
-
Linear furrows
-
White plaques/exudates
-
Erosive esophagitis
-
Decreased mucosal vascularity
-
Congested esophageal mucosa
-
Desquamation
-
Mucosal tears after passing the endoscope
-
Hiatal hernia
-
Normal appearing esophagus
-
-
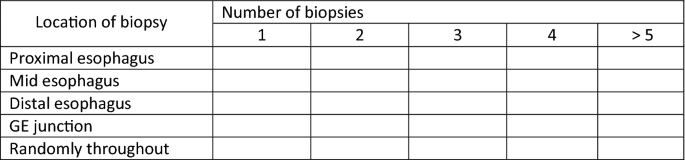
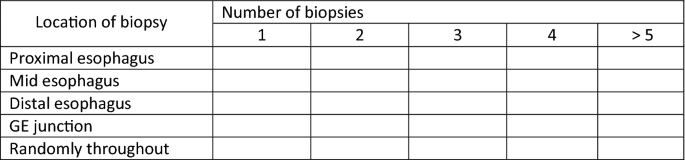
5.
From where in the esophagus do you take biopsies? (check all that apply and state how many biopsies at each location)
-
6.
Do you put biopsies from different locations in different pathology jars?
-
Yes
-
No
-
-
7.
At the time of initial diagnosis, do you take biopsies from the stomach and/or duodenum?
-
Yes
-
No
-
Yes, only if you suspect patient is having non-esophageal symptoms
-
-
8.
On esophageal biopsy, what cut-point (eosinophils/high-power field) do you use for diagnosis of EoE? (check only one)
-
5
-
10
-
15
-
20
-
24
-
30
-
Other (specify)
-
I do not use a specific cut-point
-
-
9.
Do you require that a patient is on a PPI prior to making the diagnosis of EoE?
-
Yes
-
No (go to 12)
-
-
10.
If yes, what dosing of PPI do you use?
-
Once a day
-
Twice a day
-
-
11.
What duration of PPI treatment do you use prior to making the diagnosis of EoE?
-
2 weeks
-
4 weeks
-
6 weeks
-
8 weeks
-
12 weeks
-
Other (specify)
-
-
12.
Do you stop PPI before Endoscopy? If your answer is “NO” please go to Q 14
-
Yes
-
No
-
Does not matter
-
-
13.
If your answer is “Yes” for question 12, Do you stop PPI
-
1.
48 h prior
-
2.
1–2 weeks prior
-
3.
More than 2 weeks prior
-
1.
-
14.
Do you require a negative pH probe prior to making the diagnosis of EoE?
-
Yes
-
No
-
-
15.
In infants > 6 months old, when do you consider EoE as a differential diagnosis (check all that apply).
-
Infant with troublesome reflux symptoms
-
Failing trial of EHF (If formula fed)
-
Failing trial of Dairy and soy elimination in mother’s diet (if breast fed)
-
Failure to thrive
-
Failed empiric PPI trial
-
-
16.
For diagnostic work of EoE, when do you involve allergist/immunologist (Check all that apply)
-
At the time of initial workup leading up to endoscopy
-
Only if there is a strong suspicion of IgE-mediated allergies in history
-
Positive RAST test for staple food
-
Never involve Allergist
-
-
17.
Do you use the EoE endoscopic reference (EREFS) system to grade endoscopic findings in EoE?
-
Yes
-
No
-
I am not familiar with the EREFS system
-
-
18.
Which of the following do you require to make the diagnosis of EoE? (check all that apply)
-
Consistent symptoms
-
Positive endoscopy findings
-
Positive biopsy findings
-
No clinical response to a PPI trial
-
No histologic response to a PPI trial
-
Negative pH testing
-
Exclusion of secondary causes of eosinophilia
-
Exclusion of GERD
-
-
19.
Which of the following do you do to evaluate for possible competing cause of esophageal eosinophilia prior to definitively diagnosis EoE (Check all that apply)
-
Clinical evaluation (including History and examination)
-
Growth chart (weight and Height tracking)
-
Laboratory evaluation with CBC and raised eosinophils
-
Raised inflammatory markers (CRP/ESR/raised WCC)
-
Total IgE levels
-
RAST test for staple food
-
RAST test for aeroallergens
-
Skin prick test for food allergens
-
PPI trial
-
Empiric treatment for reflux
-
Upper GI barium studies
-
Imaging cross section
-
-
20.
If you see an esophageal stricture when you are doing an endoscopy for a patient you suspect has eosinophilic esophagitis, would you perform dilation at that initial endoscopy? (check only one)
-
Yes—always
-
Yes—but only if it is a critical stricture and the patient is having dysphagia
-
No—I would wait to confirm the diagnosis and perform dilation after the patient is on treatment but still having symptoms
-
No—never
-
-
21.
If you perform a dilation, what method would you typically use? (check only one)
-
Wire-guided bougie dilator (i.e., Savary)
-
Non-guided bougie dilator (i.e., Maloney)
-
Through-the-scope balloon
-
Depends on the patient and the stricture characteristics
B. Treatment: The next set of questions is about treatment of eosinophilic esophagitis (EoE).
-
-
22.
What is your first line of therapy for treating EoE? (check only one)
-
Proton pump inhibitor once daily
-
Proton pump inhibitor twice daily
-
Swallowed topical steroid from an inhaler (i.e., fluticasone)
-
Swallowed topical steroid in liquid form (i.e., budesonide)
-
Swallowed topical steroid in a thickened liquid form (i.e., budesonide slurry)
-
Swallowed steroid plus proton pump inhibitor
-
Systemic steroid (i.e., prednisone)
-
Empiric dietary elimination therapy
-
Targeted dietary elimination therapy based on allergy testing
-
Elemental diet
-
Leukotriene antagonist (i.e., montelukast)
-
Immunomodulator (i.e., 6MP or azathioprine)
-
Biologic (i.e., mepolizumab or reslizumab)
-
-
23.
What is the first line swallowed topical steroid treatment that you typically use?
-
Budesonide liquid
-
Budesonide slurry
-
Fluticasone inhaler (swallowed)
-
Other (free text)
-
-
24.
If Budesonide, what initial total daily dose do you use in pediatric patients.
-
500 mcg
-
1000 mcg
-
1500 mcg
-
2000 mcg
-
> 2000 mcg
-
-
25.
If fluticasone, what initial total daily dose do you use in pediatric patients
-
50 mcg
-
125 mcg
-
200 mcg
-
500 mcg
-
1000 mcg
-
1500 mcg
-
2000 mcg
-
-
26.
For swallowed topical steroid treatment, do you change treatment dosing if there is response to therapy?
-
Yes, I decrease the dose
-
Yes, I discontinue the treatment
-
No, I maintain the initial dose
-
-
27.
How do you monitor response to therapy? (check all that apply)
-
Assess patient symptoms
-
Repeat endoscopy and assess endoscopic findings
-
Repeat endoscopy and assess biopsy findings
-
-
28.
Do you consider a response to therapy: (check all that apply)
-
Resolution of symptoms
-
Resolution of endoscopy findings
-
Improvement in histology (i.e., eosinophils present but less than initially)
-
-
29.
On esophageal biopsy, what cut-point (eosinophils/high-power field) do you use to assess for treatment response? (check only one)
-
0
-
≤ 1
-
< 5
-
≤ 6
-
< 10
-
< 15
-
Other (specify)
-
I do not use a specific cut-point
-
-
30.
In patients who respond to therapy, do you use maintenance therapy: (check only one)
-
Yes
-
Sometimes
-
No
-
-
31.
In patients who responded to therapy and are in maintenance therapy, how often do you do surveillance scope. (Tick as many as apply)
-
6–12 months
-
Every year
-
2 yearly
-
Only if becomes symptomatic
-
Never
-
-
32.
In patients who do not respond to initial treatment, what is your second line of therapy for treating EoE? (check only one)
-
Proton pump inhibitor once daily
-
Proton pump inhibitor twice daily
-
Swallowed topical steroid from an inhaler (i.e., fluticasone)
-
Swallowed topical steroid in liquid form (i.e., budesonide)
-
Swallowed topical steroid in a thickened liquid form (i.e., budesonide slurry)
-
Systemic steroid (i.e., prednisone)
-
Empiric dietary elimination therapy
-
Targeted dietary elimination therapy based on allergy testing
-
Elemental diet
-
Leukotriene antagonist (i.e., montelukast)
-
Immunomodulator (i.e., 6MP or azathioprine)
-
Biologic (i.e., mepolizumab or reslizumab)
-
Clinical trial
-
-
33.
Do you worry about long-term neurocognitive issues with recurrent GA for young children for EoE surveillance needing repeated EGD? (check only one)
-
Never
-
Sometimes
-
Often
-
Always
-
-
34.
What is your main objective for EoE management? (Check all if apply)
-
Clinical remission
-
Endoscopic remission
-
Histological remission
-
-
35.
Once you have reached end point of EoE treatment either on diet elimination, steroids, or on PPI. Do you stop treatment?
-
Yes
-
No
-
Stop treatment after more than 12 months of remission
-
-
36.
Once you achieve remission in EoE, do you do surveillance endoscopy?
-
Yes
-
No
-
Only if symptoms recur
-
-
37.
How familiar are you with the consensus guidelines for diagnosis and treatment of EoE?
-
Very familiar
-
Somewhat familiar
-
Not familiar
-
-
38.
How often do you have problems with pharmacologist not covering prescribed topical steroid medications (i.e., fluticasone MDI or budesonide respules) for treatment of EoE?
-
Never (skip to Section C)
-
Sometimes
-
Often
-
Always
-
-
39.
Do problems with obtaining medications from pharmacy/PBS for topical steroid medications (i.e., fluticasone MDI or budesonide respules) cause you to change your treatment choice to a different agent?
-
Yes
-
No
C. The last set of questions is about you and your practice setting.
-
-
40.
What is your practice setting?
-
Academic/Hospital setting
-
If you practice at an academic center, what is your current role?
-
Pure clinician
-
Clinician and researcher
-
Clinical researcher
-
What is your rank:
-
Lecturer
-
Associate
-
Professor
-
-
-
Private practice
-
Please select a choice that best describes your practice type
-
Solo practice
-
GI group practice
-
Multi-specialty group practice
-
-
-
41.
What type of a region do you practice in?
-
Capital City
-
Regional center
-
-
42.
What state do you currently practice in?
-
ACT, VIC, SA, WA, QLD, NT, TAS, NZ
-
-
43.
What is the average number of patients with EoE you see in a year?
-
Free text
-
-
44.
How many years have you been in practice post-fellowship?
-
Free text
-
-
45.
What are your major areas of sub-specialization? (check all that apply)
-
Esophageal disease
-
Inflammatory bowel disease
-
Functional GI disease
-
Hepatology
-
Therapeutic endoscopy
-
Motility
-
No subspecialty—general GI practice
-
Rights and permissions
About this article
Cite this article
Sharma, A., Eluri, S., Philpott, H. et al. EoE Down Under Is Still EoE: Variability in Provider Practice Patterns in Australia and New Zealand Among Pediatric Gastroenterologists. Dig Dis Sci 66, 2301–2310 (2021). https://doi.org/10.1007/s10620-020-06534-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06534-6