Abstract
Background
Biannual ultrasound (US) is recommended as the clinical screening tool for hepatocellular carcinoma (HCC). The effectiveness of surveillance according to the place where US is performed has not been previously reported.
Aims
To compare the effectiveness of US performed in the center responsible for follow-up as opposed to US proceeding from centers other than that of follow-up.
Methods
This is a multicenter cohort study from Argentina. The last US was categorized as done in the same center or done in a different center from the institution of the patient’s follow-up. Surveillance failure was defined as HCC diagnosis not meeting Barcelona Clinic Liver Cancer (BCLC) stages 0-A or when no nodules were observed at HCC diagnosis.
Results
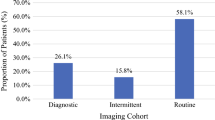
From 533 patients with HCC, 62.4% were under routine surveillance with a surveillance failure of 38.8%. After adjusting for a propensity score matching, BCLC stage and lead-time survival bias, surveillance was associated with a significant survival benefit [HR of 0.51 (CI 0.38; 0.69)]. Among patients under routine surveillance (n = 345), last US was performed in the same center in 51.6% and in a different center in 48.4%. Similar rates of surveillance failure were observed between US done in the same or in a different center (32% vs. 26.3%; P = 0.25). Survival was not significantly different between both surveillance modalities [HR 0.79 (CI 0.53; 1.20)].
Conclusions
Routine surveillance for HCC in the daily practice improved survival either when performed in the same center or in a different center from that of patient’s follow-up.




Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- BSC:
-
Best supportive care
- CI:
-
Confidence interval
- CT:
-
Computerized tomography
- ECOG:
-
Eastern Cooperative Oncology Group
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- LT:
-
Liver transplantation
- LR:
-
Liver resection
- MRI:
-
Magnetic resonance imaging
- NAFL:
-
Nonalcoholic fatty liver
- PEI:
-
Percutaneous ethanol injection
- RFA:
-
Radiofrequency ablation
- TACE:
-
Transarterial chemoembolization
References
Sherman M. Hepatocellular carcinoma: epidemiology, surveillance, and diagnosis. Semin Liver Dis. 2010;30:003–016.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–231.
Galle PR, Forner A, Llovet JM, et al. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Heimbach J, Kulik LM, Finn R, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358–380.
Méndez-Sánchez N, Ridruejo E. Latin American Association for the Study of the Liver (LAASL) clinical practice guidelines: management of hepatocellular carcinoma. Ann Hepatol. 2014;13:1–37.
Zhang B-H, Yang B-H, Tang Z-Y. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417–422.
Chen J-G, Parkin DM, Chen Q-G, et al. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. J Med Screen. 2003;10:204–209.
Singal A, Volk ML, Waljee A, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37–47.
Duvoux C, Thoraval FR, Decaens T, et al. Liver transplantation for hepatocellular carcinoma: a model including α-fetoprotein improves the performance of Milan criteria. Gatroenterology. 2012;143:986–994.
Piñero F, Tisi Baña M, de Ataide EC, et al. Liver transplantation for hepatocellular carcinoma: evaluation of the AFP model in a multicenter cohort from Latin America. Liver Int. 2016;36:1657–1667.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–1314.
Singal AG, Nehra M, Adams-Huet B, et al. Detection of hepatocellular carcinoma at advanced stages among patients in the HALT-C trial: where did surveillance fail? Am J Gastroenterol. 2013;108:425–432.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457.
Duffy SW, Nagtegaal ID, Wallis M, et al. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am J Epidemiol. 2008;168:98–104.
Fassio E, Díaz S, Santa C, et al. Etiology of hepatocellular carcinoma in Latin America: a prospective, multicenter, international study. Ann Hepatol. 2010;9:63–69.
Piñero F, Marciano S, Anders M, et al. Screening for liver cancer during transplant waiting list. Eur J Gastroenterol Hepatol. 2015;27:355–360.
Debes JD, Chan AJ, Balderramo D, et al. Hepatocellular carcinoma in South America: evaluation of risk factors, demographics and therapy. Liver Int. 2018;38:136–143.
Sherman M. Screening for liver cancer: another piece of the puzzle? Hepatology. 2014;59:1673–1675.
Trinchet J-C, Chaffaut C, Bourcier V, et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology. 2011;54:1987–1997.
Santi V, Trevisani F, Gramenzi A, et al. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010;53:291–297.
Singal AG, Tiro JA, Marrero JA, et al. Mailed outreach program increases ultrasound screening of patients with cirrhosis for hepatocellular carcinoma. Gastroenterology. 2016;2016:1–37.
Cucchetti A, Trevisani F, Bucci L, et al. Years of life that could be saved from prevention of hepatocellular carcinoma. Aliment Pharmacol Ther. 2016;43:814–824.
Wong C, Garcia RT, Trinh HN, et al. Adherence to screening for hepatocellular carcinoma among patients with cirrhosis or chronic hepatitis B in a community setting. Dig Dis Sci. 2009;54:2712–2721. https://doi.org/10.1007/s10620-009-1015-x.
Davila JA, Morgan RO, Richardson PA, Du XL, McGlynn KA, El-Serag HB. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology. 2010;52:132–141.
Singal AG, Tiro J, Li X, Adams-Huet B, Chubak J. Hepatocellular carcinoma surveillance among patients with cirrhosis in a population-based integrated health care delivery system. J Clin Gastroenterol. 2017;51:650–655.
Sherman M, Peltekian KM, Lee C. Screening for hepatocellular carcinoma in chronic carriers of hepatitis B virus: incidence and prevalence of hepatocellular carcinoma in a North American urban population. Hepatology. 1995;22:432–438.
Costentin CE, Layese R, Bourcier V, et al. Compliance with hepatocellular carcinoma surveillance guidelines associated with increased lead-time adjusted survival of patients with compensated viral cirrhosis: a multi-center cohort study. Gastroenterology. 2018;155:431–442.
Zhang B, Yang B. Combined alpha fetoprotein testing and ultrasonography as a screening test for primary liver cancer. J Med Screen. 1999;6:108–110.
Zoli M, Magalotti D, Bianchi G, Gueli C, Marchesini G, Pisi E. Efficacy of a surveillance program for early detection of hepatocellular carcinoma. Cancer. 1996;78:977–985.
Bolondi L, Sofia S, Siringo S, et al. Surveillance programme of cirrhotic patients for early diagnosis and treatment of hepatocellular carcinoma: a cost effectiveness analysis. Gut. 2001;48:251–259.
Trevisani F, De Notariis S, Rapaccini G, et al. Semiannual and annual surveillance of cirrhotic patients for hepatocellular carcinoma: effects on cancer stage and patient survival (Italian experience). Am J Gastroenterol. 2002;97:734–744.
van Meer S, de Man RA, Coenraad MJ, et al. Surveillance for hepatocellular carcinoma is associated with increased survival: results from a large cohort in the Netherlands. J Hepatol. 2015;63:1156–1163.
Johnson P, Berhane S, Kagebayashi C, et al. Impact of disease stage and aetiology on survival in hepatocellular carcinoma: implications for surveillance. Br J Cancer. 2017;116:441–447.
Kim HY, Lee JH, Lee HA, et al. Intensity of surveillance for hepatocellular carcinoma determines survival in patients at risk in a hepatitis B-endemic area. Aliment Pharmacol Ther. 2018;47:1490–1501.
Toyoda H, Kumada T, Tada T, et al. Impact of hepatocellular carcinoma etiology and liver function on the benefit of surveillance: a novel approach for the adjustment of lead-time bias. Liver Int. 2018. (Epub ahead of print). https://doi.org/10.1111/liv.13927.
Cucchetti A, Trevisani F, Cescon M, et al. Cost-effectiveness of semi-annual surveillance for hepatocellular carcinoma in cirrhotic patients of the Italian Liver Cancer population. J Hepatol. 2012;56:1089–1096.
Davila JA, Henderson L, Kramer JR, et al. Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus-infected veterans in the United States. Ann Intern Med. 2011;154:85–93.
Kim SY, An J, Lim Y-S, et al. MRI with liver-specific contrast for surveillance of patients with cirrhosis at high risk of hepatocellular carcinoma. JAMA Oncol. 2017;3:456.
Acknowledgments
We thank the Latin American Liver Research, Education and Awareness Network (LALREAN) for the support of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose as described by the Digestive Diseases and Sciences.
Financial support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10620_2018_5390_MOESM1_ESM.tiff
Supplementary Figure 1. Receiving Operator Curve from the final logistic regression model assessing probability of surveillance (TIFF 3072 kb)
10620_2018_5390_MOESM2_ESM.tiff
Supplementary Figure 2. Proportional hazard assumption and observed versus predicted curves from an adjusted survival model regarding surveillance (TIFF 3072 kb)
Rights and permissions
About this article
Cite this article
Piñero, F., Rubinstein, F., Marciano, S. et al. Surveillance for Hepatocellular Carcinoma: Does the Place Where Ultrasound Is Performed Impact Its Effectiveness?. Dig Dis Sci 64, 718–728 (2019). https://doi.org/10.1007/s10620-018-5390-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5390-z