Abstract
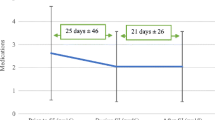
This article describes the rate of suicidal ideation (SI) across three timepoints among treatment-seeking patients recently discharged from psychiatric hospitalization—a group that is at ultrahigh-risk for suicide. Retrospective chart review was used to quantify the rate of SI in 252 consecutive patients discharged to a post-hospital mental health clinic. Data include patients’ lifetime history of SI, SI at the time of hospital intake, and SI at post-hospital outpatient clinic intake, as well as demographics and diagnosis. Overall, 67% of the sample reported a lifetime history of SI, 49% reported SI during hospital intake, and 6% reported SI at post-hospital clinic intake. Age was the only variable associated with history of SI (p = .04), with younger patients more likely (OR = 1.85) to report a history of SI. These results may help inform the development of interventions for the population of ultrahigh-risk patients being discharged from hospital after psychiatric care.
Similar content being viewed by others
References
Agency for Healthcare Research and Quality (AHRQ), Center for Delivery, Organization, and Markets, Healthcare Cost and Utilization Project (HCUP). (2012). National Inpatient Sample (NIS).
Bachman, S. (2018). Epidemiology of suicide and the psychiatric perspective. International Journal of Environmental Research and Public Health, 15(7), 1425.
Bertolote, J. M., & Fleischmann, A. (2002). Suicide and psychiatric diagnosis: A worldwide perspective. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 1(3), 181–185.
Boyer, C. A., McAlpine, D. D., Pottick, K. J., & Olfson, M. (2000). Identifying risk factors and key strategies in linkage to outpatient psychiatric Care. American Journal of Psychiatry, 157(10), 1592–1598.
Brownson, C., Drum, D., Swanbrow Becker, M. A., Saathoff, A., & Hentschel, E. (2016). Distress and suicidality in higher education: Implications for population-oriented paradigms. Journal of College Student Psychotherapy, 30, 98–113.
Centers for Disease Control and Prevention. (2019). WISQARS Leading causes of death report, 2019. https://webappa.cdc.gov/sasweb/ncipc/leadcause.html
Chung, D. T., Ryan, C. J., Hadzi-Pavlovic, D., Singh, S. P., Stanton, C., & Large, M. M. (2017). Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694–702. https://doi.org/10.1001/jamapsychiatry.2017.1044
Drum, D. J., Brownson, C., Burton, D. A., & Smith, S. E. (2009). New data on the nature of suicidal crises in college students: Shifting the paradigm. Professional Psychology: Research and Practice, 40(3), 213–222.
Franklin, J. C., Ribeiro, J. D., Fox, K. R., Bentley, K. H., Kleiman, E. M., Huang, X., Musacchio, K. M., Jaroszewski, A. C., Chang, B. P., & Nock, M. K. (2016). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. https://doi.org/10.1037/bul0000084
Have, M. T., De Graaf, R., Van Dorsselaer, S., Verdurmen, J., Van’t Land, H. J., Vollebergh, W., & Beekman, A. (2009). Incidence and course of suicidal ideation and suicide attempts in the general population. Canadian Journal of Psychiatry, 54, 824–833.
Hedegaard, H., Curtin, S. C., & Warner, M. (2020). Increase in suicide mortality in the United States, 1999–2018. NCHS Data Brief, no 362. Hyattsville, MD: National Center for Health Statistics.
Klonsky, E. D., Saffer, B. Y., & Bryan, C. J. (2018). Ideation-to-action theories of suicide: A conceptual and empirical update. Current Opinion in Psychology, 22, 38–43.
Large, M., Sharma, S., Cannon, E., Ryan, C., & Nielssen, O. (2011). Risk factors for suicide within a year of discharge from psychiatric hospital: A systematic meta-analysis. Australian and New Zealand Journal of Psychiatry, 45(8), 619–628. https://doi.org/10.3109/00048674.2011.590465
National Action Alliance for Suicide Prevention: Crisis Services Task Force. (2016). Crisis now: Transforming services is within our reach. Washington, DC: Education Development Center, Inc.
Nock, M. K., Borges, G., Bromet, E. J., Alonso, J., Angermeyer, M., Beautrais, A., Bruffaerts, M., Chiu, W. T., de Girolamo, G., Bluzman, S., e Graaf, R., Gureje, O., Haro, J. M., Huang, Y., Karam, E., Kessler, R. C., Lepine, J. P., Levinson, D., Medina-Mora, M. E., … Williams, D. (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry, 192(2), 98–105.
Olfson, M., Marcus, S. C., & Doshi, J. A. (2010). Continuity of care after inpatient discharge of patients with schizophrenia in the Medicaid program: A retrospective longitudinal cohort analysis. Journal of Clinical Psychiatry, 71(7), 831–838.
Olfson, M., Wall, M., Wang, S., Crystal, S., Liu, S. M., Gerhard, T., & Blanco, C. (2016). Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiatry, 73(11), 1119–1126. https://doi.org/10.1001/jamapsychiatry.2016.2035
Paris, J. (2002). Chronic suicidality among patients with borderline personality disorder. Psychiatric Services, 53(6), 738–742. https://doi.org/10.1176/appi.ps.53.6.738
Pinninti, N., Steer, R. A., Rissmiller, D. J., Nelson, S., & Beck, A. T. (2002). Use of the Beck Scale for Suicide Ideation with psychiatric inpatients diagnosed with schizophrenia, schizoaffective, or bipolar disorders. Behaviour Research and Therapy, 40(9), 1071–1079.
Ribeiro, J. D., Huang, X., Fox, K. R., & Franklin, J. C. (2018). Depression and hopelessness as risk factors forsuicide ideation, attempts and death: Meta-analysis of longitudinal studies. The British Journal of Psychiatry, 212(5), 279–286.
Substance Abuse and Mental Health Services Administration. (2014). Crisis services: Effectiveness, cost-effectiveness, and funding strategies. NASMHDP Publications.
Substance Abuse and Mental Health Services Administration. (2019). 2018 National survey on drug use and health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
Steer, R. A., Rismiller, D. J., Ranieri, W. F., & Beck, A. T. (1993). Dimensions of suicidal ideation in psychiatric inpatients. Behavioral Research and Therapy, 31(2), 229–36. https://doi.org/10.1016/0005-7967(93)90090-h
Valtonen, H., Suominen, K., Mantere, O., Leppämäki, S., Arvilommi, P., & Isometsä, E. T. (2005). Suicidal ideation and attempts in bipolar I and II disorders. The Journal of Clinical Psychiatry, 66(11), 1456–1462.
WHO. (2014). Preventing suicide: A global imperative. WHO.
Funding
Partial financial support for this study was provided by Merit Review Award I01BX003195 from the U.S. Department of Veterans Affairs Biomedical Laboratory Research and Development Service (to JOC) and the National Center for Advancing Translational Studies (Translational Sciences Training Award TL1 TR002647 to GAP). The content is the sole the responsibility of the authors and does not necessarily represent the views of the U.S. Department of Veterans Affairs, United States Government, and National Center for Advancing Translational Studies.
Author information
Authors and Affiliations
Contributions
All authors certify their responsibility for this manuscript. GP was lead author and data coder; CS conducted primary statistical analyses and was lead author of the methods; JO collaborated in study design, interpretation of data, and draft editing, KK was secondary coder and contributed to draft editing, DR conceptualized the study, oversaw data collection, and co-wrote all drafts.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest
Ethical Approval
This study was approved by the UTHSCSA Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Porter, G.A., Straud, C., O’Connor, J.C. et al. Suicidal Ideation Across Three Timepoints in Patients Discharged from Psychiatric Hospitalization. Community Ment Health J 58, 806–811 (2022). https://doi.org/10.1007/s10597-021-00889-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-021-00889-4