Abstract
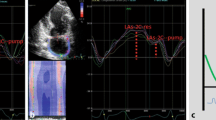
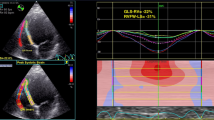
Heart failure with preserved ejection fraction (HFpEF) is a serious clinical disease. The pathophysiology of HFpEF is complex, and specific diagnostic criteria have evolved over time. Limited data are available on the quantification of diastolic function using two-dimensional real-time echocardiography, and a simple parameter has not yet been established. The aim of this work is to evaluate new echocardiographic parameters—the diastolic wall strain of the posterior wall (DWS PW) and the vortex formation time (VFT). Echocardiographic data from 111 subjects with exertional dyspnea and normal left ejection fraction (Group A) and 20 healthy volunteers (Group B) were retrospectively evaluated. In addition to the standard parameters used in the diagnosis of HFpEF, DWS PW and VFT were assessed in all patients. HFpEF was diagnosed in 38 patients with dyspnea (Group A1). The remaining 73 patients did not meet the established criteria for a positive diagnosis of HFpEF (Group A2). We discovered that both observed parameters were significantly lower in patients with HFpEF than in other groups. Multivariate analysis revealed that both DWS PW and VFT independently predicted the presence of HFpEF. DWS PW and VFT are simple parameters in the evaluation of diastolic function and may play a potential role as a part of an integrated approach to the assessment of HFpEF.




Similar content being viewed by others
References
Lam CSP, Donal E, Kraigher-Krainer E, Vasan RS (2011) Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail 13(1):18–28
ElGuindy A, Yacoub MH (2012) Heart failure with preserved ejection fraction. Glob Cardiol Sci Pract 2012(1):10
Oktay AA, Rich JD, Shah SJ (2013) The emerging epidemic of heart failure with preserved ejection fraction. Curr Heart Fail Rep 10(4):401–410
Mandinov L, Eberli FR, Seiler C, Hess OM (2000) Diastolic heart failure. Cardiovasc Res 45(4):813–825
Owan TE, Redfield MM (2005) Epidemiology of diastolic heart failure. Prog Cardiovasc Dis 47(5):320–332
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200
Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28(20):2539–2550
Meluzín J, Sitar J, Křístek J, Prosecký R, Pešl M, Podroužková H et al (2011) The role of exercise echocardiography in the diagnostics of heart failure with normal left ventricular ejection fraction. Eur Heart J 12(8):591–602
Dokainish H, Sengupta R, Pillai M, Bobek J, Lakkis N (2008) Assessment of left ventricular systolic function using echocardiography in patients with preserved ejection fraction and elevated diastolic pressures. Am J Cardiol 101(12):1766–1771
Takeda Y, Sakata Y, Higashimori M, Mano T, Nishio M, Ohtani T et al (2009) Noninvasive assessment of wall distensibility with the evaluation of diastolic epicardial movement. J Card Fail 15(1):68–77
Gharib M, Rambod E, Kheradvar A, Sahn DJ, Dabiri JO (2006) Optimal vortex formation as an index of cardiac health. Proc Natl Acad Sci USA 103(16):6305–6308
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H et al (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2(5):358–367
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57(6):450–458
Tanalp AC, Bitigen A, Cevik C, Demir D, Ozveren O, Tigen K et al (2008) The role of tissue Doppler study in the assessment of left ventricular dysfunction in obesity. Acta Cardiol 63(5):541–546
Ohtani T, Mohammed SF, Yamamoto K, Dunlay SM, Weston SA, Sakata Y et al (2012) Diastolic stiffness as assessed by diastolic wall strain is associated with adverse remodelling and poor outcomes in heart failure with preserved ejection fraction. Eur Heart J 33(14):1742–1749
Martínez-Legazpi P, Bermejo J, Benito Y, Yotti R, Pérez Del Villar C, González-Mansilla A et al (2014) Contribution of the diastolic vortex ring to left ventricular filling. J Am Coll Cardiol 64(16):1711–1721
Poh KK, Lee LC, Shen L, Chong E, Tan YL, Chai P et al (2012) Left ventricular fluid dynamics in heart failure: echocardiographic measurement and utilities of vortex formation time. Eur Heart J 13(5):385–393
Kheradvar A, Assadi R, Falahatpisheh A, Sengupta PP (2012) Assessment of transmitral vortex formation in patients with diastolic dysfunction. J Am Soc Echocardiogr 25(2):220–227
Selvaraj S, Aguilar FG, Martinez EE, Beussink L, Kim K-YA, Peng J et al (2014) Diastolic wall strain: a simple marker of abnormal cardiac mechanics. Cardiovasc Ultrasound 12:40
Bruch C, Gradaus R, Gunia S, Breithardt G, Wichter T (2003) Doppler tissue analysis of mitral annular velocities: evidence for systolic abnormalities in patients with diastolic heart failure. J Am Soc Echocardiogr 16(10):1031–1036
Tan YT, Wenzelburger F, Lee E, Heatlie G, Leyva F, Patel K et al (2009) The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J Am Coll Cardiol 54(1):36–46
Jiamsripong P, Calleja AM, Alharthi MS, Dzsinich M, McMahon EM, Heys JJ et al (2009) Impact of acute moderate elevation in left ventricular afterload on diastolic transmitral flow efficiency: analysis by vortex formation time. J Am Soc Echocardiogr 22(4):427–431
Bermejo J, Benito Y, Alhama M, Yotti R, Martínez-Legazpi P, Del Villar CP et al (2014) Intraventricular vortex properties in nonischemic dilated cardiomyopathy. Am J Physiol Heart Circ Physiol 306(5):H718–H729
Krueger P, Gharib M (2003) The significance of vortex ring formation to the impulse and thrust of a starting jet. Phys Fluids 15(5):1271–1281
Dabiri JO, Gharib M. The role of optimal vortex formation in biological fluid transport. ResearchGate 272(1572):1557–1560
Linden PF, Turner JS. The formation of “optimal” vortex rings, and the efficiency of propulsion devices. ResearchGate 427:61–72
Jiamsripong P, Alharthi MS, Calleja AM, McMahon EM, Katayama M, Westerdale J et al. Impact of pericardial adhesions on diastolic function as assessed by vortex formation time, a parameter of transmitral flow efficiency. Cardiovasc Ultrasound 8:42
Acknowledgements
This work was supported by Grant IGA MZ ČR 14087-3/2013 and Specific University Research MUNI/A/1270/2015 and by the project No LQ 1605 from the National Program of Sustainability II (MEYS CR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Špinarová, M., Meluzín, J., Podroužková, H. et al. New echocardiographic parameters in the diagnosis of heart failure with preserved ejection fraction. Int J Cardiovasc Imaging 34, 229–235 (2018). https://doi.org/10.1007/s10554-017-1230-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1230-z